The United States lags about 15 years behind the rest of the world in surgical technologies getting into the hands of clinicians. Therefore, to get a sense of the future of eye care, it is helpful to look at the experiences of those lucky enough to have early access to exciting technologies.
ADVANCED LASERS
After performing the first 500-Hz excimer surgeries in the United States, I came to realize what we have all suspected for some time: speed matters. The fast repetition rate in this laser likely leads to less stromal dehydration possibly resulting in faster recovery times. The human cornea’s tolerance for thermal energy has been well described in the literature, and these advanced lasers are well within these limits. One example of this technology is the Schwind Amaris, which is a 500-Hz repetition rate laser with advanced tracking capabilities and on-board OCT. The fastest laser in the world currently is a prototype 1,000-Hz model by Wavelight (Alcon Laboratories, Inc.), which is currently used in Europe and treats 1.00 D per second.
Speed is not the only upgrade to laser technology, however. Topography-guided ablation patterns have been used for years in Europe, Asia, and Canada. In addition to producing excellent outcomes in normal, healthy eyes, this feature provides surgeons the ability to correct irregular astigmatism and highly aberrated eyes therapeutically. Significant advances in femtosecond flap makers are also occurring. The new Ziemer Z6 (Ziemer Ophthalmic Systems AG) has an option for on-board OCT, allowing for postablation cuts and opening the door for simultaneous dual interface creation, which means the potential to create a pocket under a thin LASIK flap for corneal inlays.
Crosslinking
Corneal collagen crosslinking (CXL) has been used for years in Europe to treat patients with keratoectasia (Figure 1). Safety and efficacy data have been published and are well accepted. The primary indication for CXL is for stabilizing eyes with keratoectasia. There are a number of exciting new modifications to the procedure, including epithelial-on (epi-on) treatments with bioenhanced riboflavin solutions such as Ricrolin TE (SOOFT Italia). Epi-on treatments have the clear benefit of faster recovery and less discomfort to the patient with a more favorable safety profile. More comparative evidence is needed to determine the efficacy of epi-on procedures compared to the traditional epithelium-off (epi-off), but the initial results are promising.

Figure 1. New indications and techniques are expanding the
scope of CXL.
LASIK extra, or LASIK combined with limited crosslinking for patients who may be borderline candidates or at higher risk for regression is another exciting new use of the procedure. Some early evidence from Japan suggests that this procedure is safe and may lead to improved refractive stability after LASIK. Topography-guided customized treatments are also being developed to preferentially treat the most severely affected parts of the cornea. Finite element models have suggested that this may lead to an improved corneal shape after crosslinking.
Advanced Astigmatism correcting IOLs
The AcrySof IQ Restor +3.0 Multifocal Toric IOL (Alcon Laboratories, Inc.) has been a mainstay of simultaneous treatment of presbyopia and astigmatism outside the United States since it was introduced at the European Society of Cataract & Refractive Surgeons annual meeting in 2010. Early data on the Crystalens toric accommodative IOL (Bausch + Lomb) are also encouraging.
Another interesting advanced technology lens is the Light-Adjustable Lens (Calhoun Vision, Inc.), which is constructed of a photosensitive silicone that can be adjusted postoperatively to increase or decrease the lens power to correct sphere or astigmatism (by changing power in one axis). Patients undergo routine IOL implantation and the lens power is adjusted 2 weeks postoperatively; once on target, the IOL power is “locked in.” A central add may be induced in the future to increase spherical aberration for increased depth of focus.
Presbyopic Inlays
A number of corneal inlays for the surgical management of presbyopia are currently approved outside the US and are gaining popularity where available. These inlays can be implanted through a corneal pocket or under a lamellar corneal flap; all are typically implanted in the nondominant eye, and can be easily removed if needed.
The Kamra intracorneal inlay (AcuFocus, Inc.) is a 5-μm thick biocompatible inlay made of polyvinylidine fluoride, inserted either under a lamellar flap or into a corneal pocket (Figure 2). The inlay has a 1.6-mm central annulus that acts as a pinhole, and its outer diameter is 3.8 mm. This small aperture selects for nonbent rays of light, providing a broad depth of focus for all distances. A key benefit of a small aperture inlay is the stability of near and intermediate acuity despite the progressive nature of presbyopia.
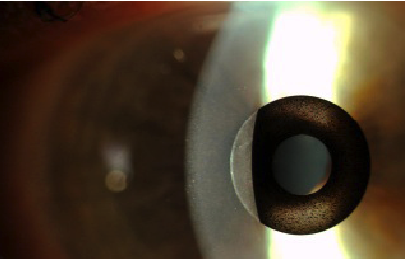
Figure 2. The Kamra intracorneal inlay is one of several inlays designed to address presbyopia at the corneal plane.
The Icolens (Neoptics) is a 3-mm diameter multifocal corneal inlay, which uses the peripheral zone for near vision correction and a central zone for distance vision. This lens is made of a hydrophilic acrylic hydrogel, and it is the most recent corneal inlay to be introduced into this space.
The Presbia Flexivue Microlens (PresbiTech, Inc.) uses refractive add power to improve reading vision. The hydrophilic acrylic lens is 3 mm in diameter and about 15 µm in edge thickness. The device is placed in a pocket in the nondominant eye at a depth of 300 µm.
The Raindrop (ReVision Optics, Inc.), is a 2-mm diameter permeable hydrogel lenticule which is implanted under a lamellar flap (about 120-130 µm depth) in the nondominant eye for the treatment of plano presbyopia. It creates a central steepening for near and intermediate vision, and light rays paracentral to the inlay remain focused on the retina. Distance acuity is minimally affected as light rays paracentral to the 2-mm inlay remain primarily focused on the retina, particularly with a dilated pupil. Pupillary constriction creates a pseudoaccommodative state, utilizing the steepened central cornea.
Diagnostics
The Corvis ST (Oculus Optikgeräte GmbH) is a dynamic tonometer combined with a rotating Schiempflug camera. The Corvis is one of a few devices being developed to measure biomechanical properties of the cornea, an area of great interest to cornea and refractive surgeons. Dynamic videos of corneal deformation with an applied force are generated, and metrics are extrapolated based on a number of biomechanical factors. This device has great potential for evaluating ectatic eyes after CXL and potentially for screening for refractive surgery, particularly in patients with subclinical ectasia.
The Salzburg Reading Desk (SRD Vision) represents a new paradigm in diagnostics: functional vision testing. This is one of the first devices of its kind that objectively measures reading speed at different distances. A number of peer-reviewed articles have been published demonstrating the applications and efficacy of the device. With several options for surgical correction of presbyopia emerging, devices such as these are likely to become more commonplace.
CONCLUSION
Technologies are rapidly advancing in the worldwide marketplace. This article not only summarizes some of these technologies currently available outside the United States, but also serves as a glimpse of what we can expect here in the future.
Global Product Links
Advancing Lasers
Crosslinking
Advanced Astigmatism Correcting IOLs
Restor +3.0 Multifocal Toric IOL



