Today’s cataract patients are younger and their expectations of cataract surgery are higher than ever before. Two big trends are driving this change in the type of cataract patient we typically see: (1) the baby boomers are reaching Medicare age, and (2) more individuals are undergoing cataract surgery at a younger age.
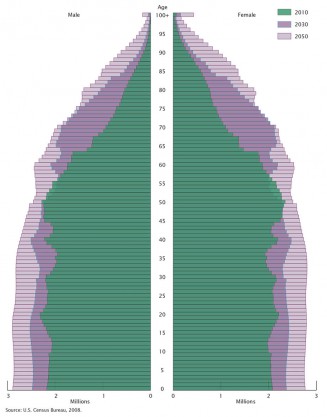
As the baby boomers get older, the age pyramid in the United States is becoming more of a rectangle.
Every day, 10,000 baby boomers—those born between 1946 and 1964—turn 65. By 2030, everyone in this demographic bulge will be over age 65 (Figure 1). Compared with previous generations, baby boomers are better educated and more likely to be in professional and managerial positions.1 They are expected to live longer and spend more time in the workforce. Although obesity and chronic conditions such as hypertension, diabetes, and hypercholesterolemia are common,2 baby boomers are considered to be quite interested in ongoing vitality. They have demonstrated a willingness to spend their resources on health and wellness, luxury goods, and lifestyle pursuits.
At the same time that this large pool of patients is reaching the point at which age-related diseases are common, more people are having cataract surgery and at younger ages.3 I certainly see this in my practice and think it is likely due to a combination of factors.
Today’s middle-aged and older adults have significantly higher visual demands than generations past. Not only are people working longer, but their leisure activities are more varied and much more likely to involve computers and handheld devices that challenge near and intermediate visual acuity. My sense is that this increases sensitivity to mild visual changes due to cataracts.
Many of my patients, in fact, are so bothered by early lens changes that they don’t even want to wait until they qualify for cataract surgery and instead request a refractive lens exchange. This is particularly true of post-LASIK patients who are experiencing lens changes and the onset of presbyopia. They are excited to learn that femtosecond laser surgery with multifocal IOL implantation can solve both of those problems as well as correct any residual astigmatism from prior surgery.
Finally, health or medication factors that may also contribute to earlier cataract development include the widespread use of inhaled steroids4 and the higher incidence of diabetes.
TREATING YOUNGER PATIENTS
There are advantages to performing lens surgery in younger patients. The lenses can be removed more easily, without excessive ultrasound energy, and their pupils tend to dilate very well compared with older, more tamsulosin (Flomax)-affected eyes. Younger eyes heal faster and have less edema, so their visual recovery is fast and predictable.
On the flip side, these patients have many years of vision ahead of them and have high expectations for visual performance, so the stakes of “getting it right” are higher. Today’s technology has greatly increased the precision of cataract surgery and the predictability of outcomes to the point that I am very comfortable performing cataract surgery or refractive lensectomy in eyes with modest lenticular changes.
Additionally, we can now get closer to patients’ goals of seeing well at all distances, without side effects or major “gaps” in their vision.
OPTIONS FOR MULTIFOCALITY
In the United States, our options for presbyopes have been limited to monovision, with its well-known tradeoffs; an accommodating IOL with somewhat inconsistent near vision; and two diffractive multifocal IOLs, the AcrySof ReStor (Alcon) with a +3.00 D or +4.00 D add and the Tecnis Multifocal (Abbott Medical Optics), which has a +4.00 D add.
My patients have been happy with the near vision achieved with the Tecnis Multifocal, but the gap in intermediate vision can be bothersome, especially given the growing importance of intermediate computer tasks. Additionally, about 10% to 15% of my patients experienced some glare and halos at night with this lens.
New low-add multifocals, which have been used in Europe for some time but are just becoming available in the United States, may solve these problems. I recently began implanting the new +3.25 D and +2.75 D add versions of the Tecnis Multifocal (ZLB00 and ZKB00, respectively).
A nice feature of the lower add powers is that they are optically identical to the +4.00 D Tecnis Multifocal, with the reading distance being the only difference. This makes them very compatible if one wants to mix and match IOLs within the platform. Initially, I thought this would be the best approach and performed surgery for several patients with a +4.00 D multifocal in one eye and a +2.75 D multifocal in the other. This was a very good combination that patients appreciated.
However, with more experience, I find that I am leaning toward bilateral implantation of the +2.75 D Tecnis Multifocal. It provides excellent distance and intermediate vision, and patients don’t seem to notice a deficit at near. None of the patients I’ve implanted with this lens have complained about not being able to read, and they can all see their computer and distance. This is probably related to the excellent defocus curve of the ZKB00, which shows 20/15 to 20/25 vision from distance to about +2.50 D of defocus (Figure 2). Additionally, the rate of night vision problems has dropped to <1%, which is encouraging.
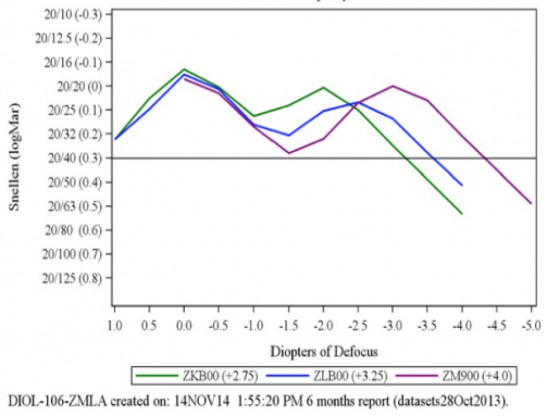
The new low-add Tecnis Multifocal (ZKB00) maintains 20/25 or better vision from distance to about +2.50 D of defocus.
CONCLUSION
There is certainly still a role for higher-add multifocal IOLs in patients whose hobbies or professions require extensive near tasks and in shorter patients who may naturally hold devices or reading material at a closer distance. However, for most of my presbyopic patients, I believe bilateral low-add multifocal IOLs will provide the best vision at all distances with the fewest side effects—nicely matching up with their expectations of contemporary cataract surgery.
1. Pruchno R. Not your mother’s old age: baby boomers at age 65. The Gerontologist. 2012.
2. King DE, Matheson E, Chirina S, et al. The status of baby boomers’ health in the United States: the healthiest generation? JAMA Intern Med. 2013;173(5):385-386.
3. Gollogly HE, Hodge DO, St. Sauver JL, Erie JC. Increasing incidence of cataract surgery: Population based study. J Cataract Refract Surg. 2013;39(9):1383-1389.
4. Weatherall M, Clay J, James K, et al. Dose-response relationship of inhaled corticosteroids and cataracts: a systematic review and meta-analysis. Respirology. 2009;14(7):983-990.