Participants

George O. Waring IV, MD, FACS, moderator, is the founder and medical director of Waring Vision Institute, Mt. Pleasant, South Carolina. He is a consultant to Johnson & Johnson Vision. Dr. Waring can be reached at gwaring@waringivision.com.

Kendall E. Donaldson, MD, MS, is associate professor of ophthalmology, cornea/external disease/cataract/refractive surgery, medical director and cornea fellowship codirector at the Bascom Palmer Eye Institute, Plantation, Florida. She is a consultant to Johnson & Johnson Vision. Dr. Donaldson can be reached at kdonaldson@med.miami.edu.

Eva Liang, MD, practices at the Center for Sight in Las Vegas, Nevada, and she is founder of the nonprofit organization Sight for Life. She is a consultant to Johnson & Johnson Vision. Dr. Liang can be reached at eva.liang@c4slv.com.

Gary Wörtz, MD, practices at Commonwealth Eye Surgery in Lexington, Kentucky. He is founder and chief medical officer of Omega Ophthalmics. He is a consultant to Johnson & Johnson Vision. Dr. Wörtz can be reached at garywortzmd@gmail.com.
FLACS Landscape
George O. Waring IV, MD: Cataract surgeons in the United States began using femtosecond lasers in 2011, and we have seen steady growth ever since. Results of a Market Scope study showed that 62% of ophthalmologists who attended the 2015 MillennialEYE Live Meeting were offering femtosecond laser-assisted cataract surgery (FLACS) versus the national average, which was 39%.1
Dr. Donaldson, tell us about your experience with the femtosecond laser in your academic practice.
Kendall E. Donaldson, MD: We acquired our CATALYS Precision Laser System (Johnson & Johnson Vision) in 2012, and being involved in the introduction of femtosecond laser technology for cataract surgery has been exciting. Not only is it exciting for us to have a new tool, but the possible use of laser technology is exciting for our patients, who associate lasers with precision.
Dr. Waring: In 2016, Market Scope reported that approximately half of surgeons polled are either currently offering femtosecond laser technology to their cataract patients or are planning to offer it in the next year (Figure 1).2 To have this sort of paradigm shift in only 5 years is remarkable. What has been your experience in terms of adoption in your community, Dr. Liang?
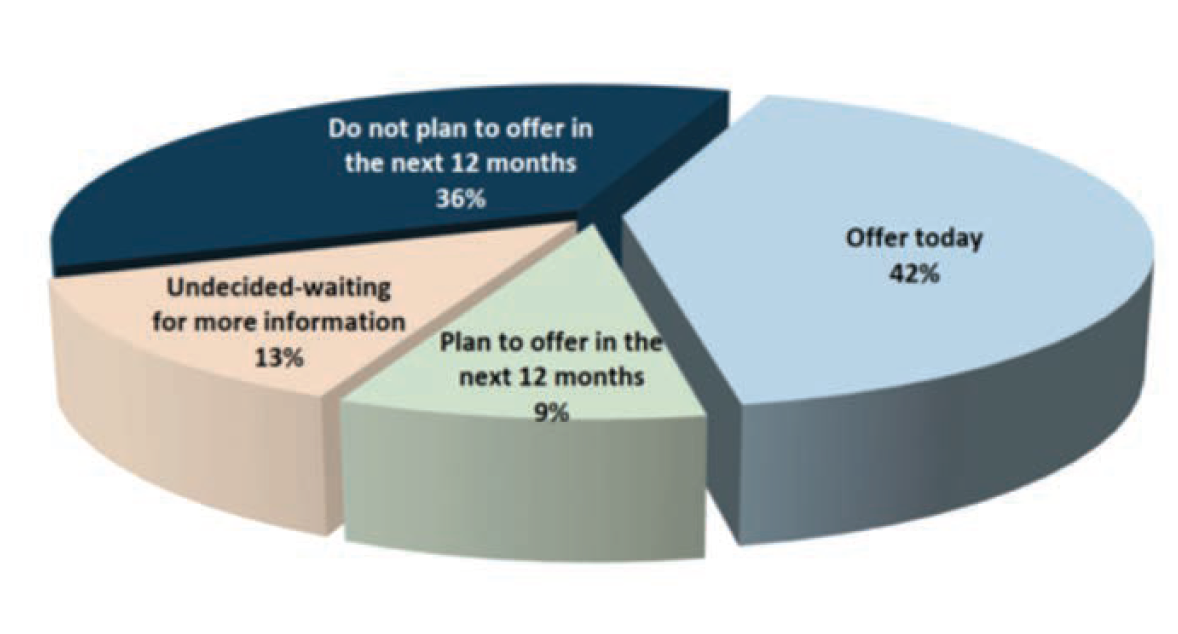
(Courtesy of George O. Waring IV, MD)
Figure 1. In 2016, Market Scope reported that approximately half of surgeons polled offer femtosecond laser cataract surgery or intend to offer it within the next year.
Eva Liang, MD: Just a few of us in the community were offering femtosecond cataract surgery in 2013 when I opened my practice, but over the years, more surgeons have come on board. I believe conversion rates depend on the platform you use and the confidence you have in your equipment (See Not All Femtosecond Lasers Are Created the Same below).
Dr. Waring: Nearly three-fourths of surgeons are now using femtosecond lasers to create LASIK flaps, according to the 2016 ASCRS Clinical Survey, but that utilization rate represents a decade or more of adoption.3 Dr. Donaldson, do you foresee similar growth in the use of femtosecond lasers for cataract, such as the CATALYS System used for cataract surgery only and not LASIK? What are the barriers to adoption?
Dr. Donaldson: The main reason why surgeons have not adopted femtosecond technology for their cataract surgeries is the financial investment, according to the 2016 ASCRS Clinical Survey.4 This is understandable, because incorporating femtosecond technology into your surgeries is a commitment. In addition to acquiring the technology and devising a marketing plan, you must train your staff and educate your patients so that everyone is on board and believes in this technology.
The second barrier cited by some surgeons is that they are waiting for confirmation that the improvements in outcomes warrant the expense. They want to see the gain relative to the investment.
I think the comparatively rapid acceptance of the femtosecond laser for LASIK was related to complications associated with the microkeratome. There were clear differences with regard to safety. We are still accumulating safety data for cataract surgery.
Dr. Liang: I believe some physicians are somewhat tentative about adopting new technology because of how it changes things in the OR. To me, having a laser like the CATALYS, which, in my experience, is easy to dock and comfortable for patients, is a no-brainer.
Gary Wörtz, MD: I view the femtosecond laser as a tool, and as with any tool, you must use it in different ways until you learn how it works best in your hands. An advantage with the CATALYS is that you can customize it to your own needs (Figure 2).
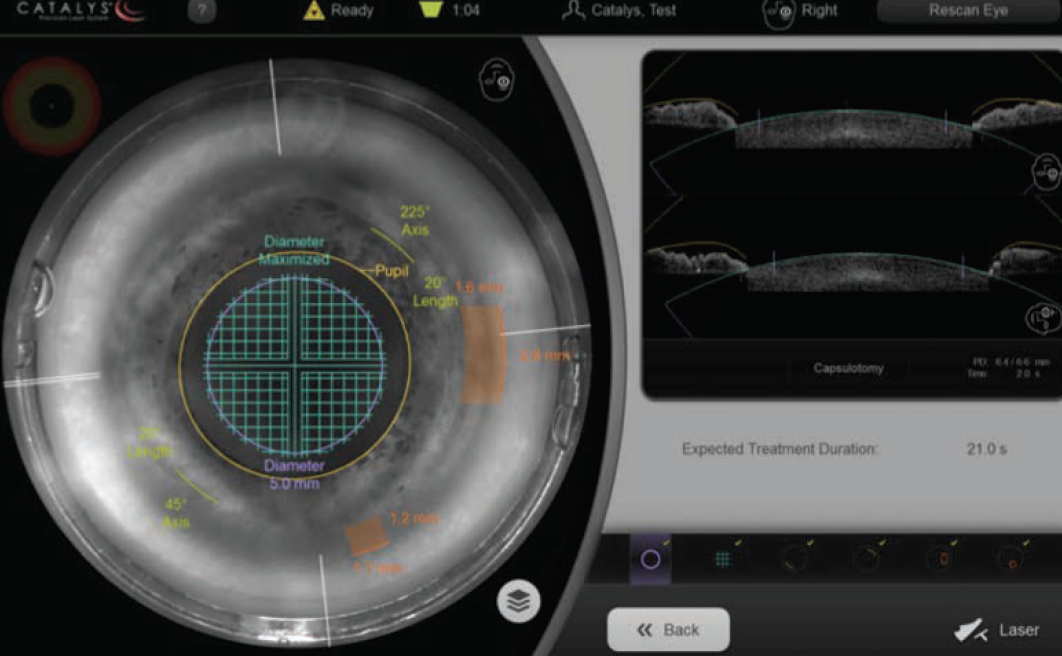
Figure 2. CATALYS allows surgeons to use the patient's unique anatomy to precisely place each incision.
Dr. Waring: The intuitive interface of the CATALYS system is one of its strong points. It is simple to navigate and offers a user-friendly experience.
Explaining FLACS to Patients
Dr. Waring: How has having the CATALYS laser influenced your conversations with patients? How do you introduce the concept of using a laser for cataract surgery to patients?
Dr. Donaldson: Patients hear about the femtosecond laser from me first. I tell every patient about all available options, and then explain what I feel is best for him or her. I always begin the conversation, and my surgical coordinator takes it to the next level.
In order for FLACS to be successful, the surgeon has to believe in it and attain a level of understanding through research and working with colleagues. When you understand and believe in the benefits for your patients, that belief is propagated to your staff and your patients.
Dr. Waring: Dr. Liang, what is the usual protocol in your practice?
Dr. Liang: Most of our patients are referred to us specifically for cataract surgery. They undergo testing, and they watch videos while their pupils are dilating, so they already have some basic information before they see the surgeon who discusses their options. Our surgical counselor finalizes the details with them.
Dr. Waring: We follow a similar routine in my practice. Our staff members educate patients throughout their consultation process. Patients watch videos that explain advanced technology while their pupils are dilating, after which we discuss the options and associated benefits and what procedure we feel is the best fit. Our staff members are trained to deliver consistent messaging throughout each patient’s experience, which is important.
Advanced Technology Options
Dr. Waring: How do you present the various options available with the femtosecond laser? Do you offer them as “premium” packages? Dr. Wörtz, what is your approach?
Dr. Wörtz: This is a key point. I describe the laser as a tool and explain that just as we use the latest technology in our preoperative testing, so do we use the laser during surgery to ensure predictable outcomes. I emphasize outcomes more than any specific tool, because everything has to work in concert to ensure a good outcome. I definitely feel the CATALYS laser plays a key role in that. We present the laser as part of a premium package.
Dr. Donaldson: At the Bascom Palmer Eye Institute, we have two levels of upgrade. First, I explain routine cataract surgery, and then I describe our refractive cataract surgery packages. One option is astigmatism correction, and it includes additional testing and the use of the laser as part of the overall procedure. The second option is our presbyopia package, which also includes the laser and all of the necessary testing. These packages, of course, include the implantation of a toric, multifocal, or extended-depth-of-focus IOL.
I keep the explanations as simple as possible, so patients do not become overwhelmed and confused. Many patients come in thinking they will have a cataract removed, and now they find they have to make some decisions. I emphasize that these are great decisions, and I encourage patients to embrace them. I tell them, “This is a major change in your life. This is a wonderful process that you are going through, because we are able to offer new options that were not available 10, 15, 20 years ago. You are very lucky.”
Dr. Liang: We use a “good, better, best” model to present cataract surgery options. I explain that the basic surgery, which includes a basic lens, is good surgery. Patients can opt for intraoperative aberrometry for a fee, even with the “good” package. “Better” is upgrading with either the method of surgery or the lens type, and “best” includes both. For us, it is a simple explanation.
Not All Femtosecond Lasers Are Created the Same
Dr. Wörtz: My first experience with a femtosecond laser was in 2012, when I was working in a different practice. It was an early version of another platform, and I quickly became dissatisfied with it and stopped using it. At that time, I was experiencing frustrations with docking and still having incomplete capsulotomies from time to time. We should recognize that all laser platforms have evolved since that time. However, I clearly had a false start with femtosecond technology.
After a few years, I joined a new practice that had a CATALYS laser system already up and running. This was a system that really worked. The laser was fantastic. It was easy to learn and the precision was higher.5 I adapted quickly to the CATALYS laser.
Over time, I have seen the platform become even more robust. For me, it has been fun experience. When we are excited about a technology and we see the precision and the results, it is easy to talk to patients about that. When they see that we are confident about a tool that we want to use, it is much easier for them to make that decision.
Dr. Donaldson: We have three different laser platforms at the Bascom Palmer Eye Institute. My technicians who run the lasers like the CATALYS system because it is intuitive and user friendly, and they appreciate the many safeguards built into the system. With all of the laser platforms, errors are possible, but our technicians love the CATALYS laser because it takes responsibility out of their hands by internalizing many safeguards and mechanisms for security throughout the procedure.
Dr. Liang: I introduced a femtosecond laser for cataract surgery into my practice when I opened in 2013. I started with a different platform, and I did not have the same sort of conviction when educating patients as I do now when discussing the CATALYS system. In my community, just a few of us were offering femtosecond technology, even back in 2013, but over the years more people have jumped on board.
Conversion rates are different among the surgeons I know, and I have noticed that it often depends on the platforms they use. When you are confident with your technology, the message will be evident when you educate patients on their options. Having used three different lasers, I can say that not all lasers are created equal (Figure 3), and the CATALYS system is my favorite. It delivers higher precision and accuracy.5
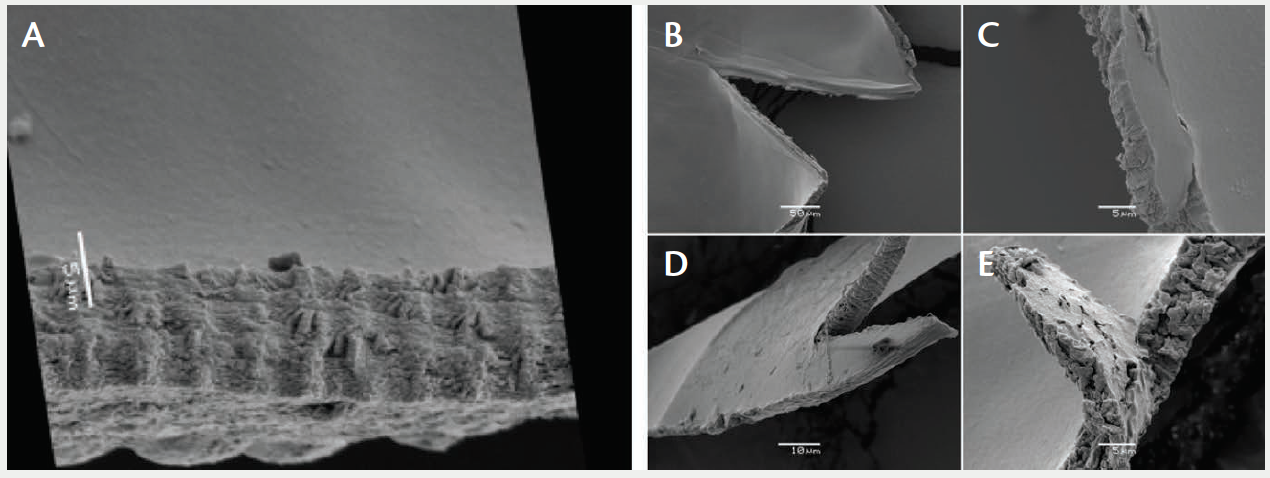
Figure 3. Example of a capsulotomy generated by the CATALYS (A) and other systems: LenSx System SoftFit Patient Interface (B,C), Victus System I (D), and Victus System II (E).6,7
Workflow Optimization
Dr. Waring: Efficiencies and flow are important considerations when introducing new technology into the OR. Earlier we touched on potential barriers to adopting laser technology, but we did not discuss efficiency. Inefficiency can be a barrier, not only in the clinic but, more importantly, in the OR.
Dr. Donaldson, what is your current operating procedure for femtosecond laser-assisted cataract surgeries?
Dr. Donaldson: I practice in an academic setting, which is a less efficient model than private practice. We have three femtosecond lasers: two, including our CATALYS laser, are located in the OR, and one is located outside the OR. We have found that we add 7 minutes to each case when the laser is in the OR. When the laser is outside the OR, we reduce our time by 5 minutes.
OR time does depend on the location of the lasers. I think most doctors in private practice place the laser outside the OR for some of these reasons.
Dr. Waring: Dr. Wörtz, what is your usual workflow? Have you made any changes since you began using the femtosecond laser?
Dr. Wörtz: Our femtosecond laser is set up in a separate room across from our ORs. We try to alternate standard or insurance-based surgery with a FLACS case, and ideally I rotate among three rooms. I operate on a standard case, a femtosecond case, and another standard case. By the time I return to the first room, a patient scheduled for FLACS is there.
I have changed the way I use the femtosecond laser. I do not use it for the primary and sideport incisions, only for the capsulotomy, lens chops, and arcuate corneal incisions. I have adjusted my settings so that I can do an efficient four-quadrant chop and not do any lens fragmentation.
Dr. Waring: Dr. Liang, how do you maintain efficiency? Have you changed anything since you began using the femtosecond laser?
Dr. Liang: Actually, my mindset has changed. When I first adopted FLACS, I was worried about adding additional steps, but at the end of the day, the patient is choosing a premium service, and I think it is perfectly reasonable for the surgery to take longer.
Initially, as we developed our routine and flow, we decided our most efficient approach would be to create what we call a femto sandwich. We do two or three basic cases first, while the pupils of patients who will receive FLACS are dilating. We alternate cases—femto, basic, femto, basic—until all femto cases are completed, and then we wrap up the day with basic cases.
Because some extra intraoperative steps are involved for the patients who choose the premium packages, those cases take longer. I just cannot avoid that. As for efficiency, I am doing a similar number of cases now compared to the number I did before I started using the laser. It might take me a little bit longer at the end of the day, but I think it is worth it for everyone involved.
Features That Make a Difference
Dr. Waring: The CATALYS laser offers multiple capabilities including: capsulotomy, lens fragmentation or prechopping, corneal arcuate incisions, primary and sideport incisions, Liquid Optics Interface, and image-guided surgery. What features of the CATALYS laser technology intrigued you the most and made you feel like you needed to offer this to your patients?
Dr. Liang: I was one of those people who thought, “I am a good surgeon. I do not need a laser,” until a friend encouraged me to try it. After the first case, I realized that incorporating the femtosecond laser into my practice was a no-brainer.
One of the best features of the CATALYS is that it locates the anatomical center of the lens and puts your capsulotomy there, which definitely helps with premium IOL centration. If I have a complicated case and need optic capture, I know exactly how big my capsulotomy is. In addition, the fragmentation is precise.
Before I tried the CATALYS laser, I thought it would not make much of a difference. Being in the driver’s seat and doing a case that has been prefragmented or treated with the femtosecond laser really does make a difference. The arcuate incisions are also precise and customizable.
Dr. Waring: Dr. Wörtz, what made you choose the CATALYS system?
Dr. Wörtz: Two words describe why I prefer the CATALYS laser: intuitive and precise. The platform is so intuitive, it seems like it was designed by surgeons with a surgeon’s mindset. Docking is easy. The interface locates anatomical surfaces consistently.
Dr. Donaldson: One of the main strengths of the CATALYS system is that it was designed specifically for intraocular surgery, not derived from systems designed for corneal surgery, as is the case with some of the other laser platforms being used for cataract surgery.
After working with several laser platforms, I can really see the differences, whether it is in the precision of the optical coherence tomography-guided imaging or the safeguards that are incorporated into the system. Those are some of the main features that distinguish the CATALYS laser from other laser platforms.
Advantages of a Femtosecond Capsulotomy
Dr. Waring: In your hands, is the CATALYS laser capsulotomy more sustainable in shape and size than a free-hand capsulotomy?
Dr. Wörtz: Whenever I have had a skip area or an area where the capsulorhexis was incomplete, it was always because of an opacification in the cornea (Figure 4). In one case, the cornea dried out somewhat, either while the patient was being prepped or while the pupil was dilating. When I noticed that the cornea was exhibiting some superficial punctate keratitis, I knew I needed to be aware of that area. Just like anything else in surgery, it is a dynamic situation.
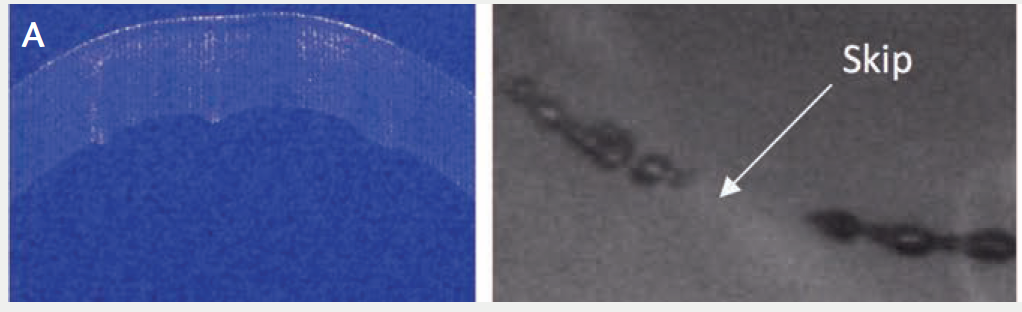
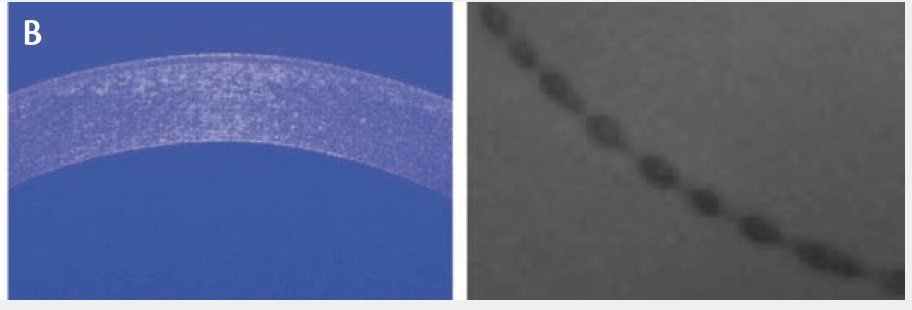
Figure 4. The true nonapplanating Liquid Optics Interface does not demonstrate corneal folds and therefore does not interfere with laser delivery.8 Images show a capsulotomy with corneal folds (A) and a complete capsulotomy (B).
Good Candidates
Dr. Waring: How do you determine which patients are likely to be good candidates for FLACS?
Dr. Donaldson: Patients ask me this question every day. When patients have dense cataracts, I tell them, yes, you may benefit. I also feel that my arcuate incisions benefit patients (Figure 5). Everyone who chooses premium lenses in our practice, whether toric or presbyopia-correcting, is treated with the femtosecond laser, if they are a suitable patient.
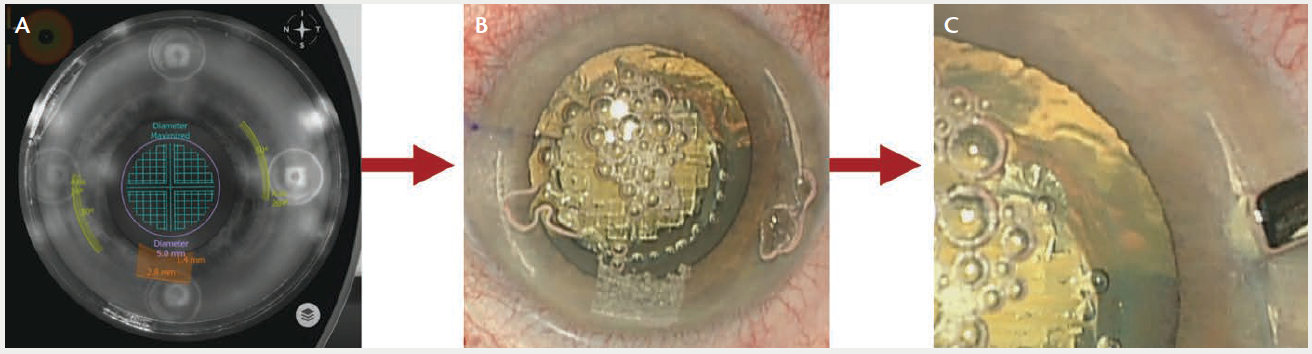
Figure 5. Arcuate incisions are clinically validated within: 0.83 ± 0.66% of intended optical zone, 0.22 ± 0.20° of intended axis, and 0.22 ± 0.29° of intended length.9 Images show the CATALYS treatment plan (A), OR view (B), and blunt dissection (C).
During the New Orleans Academy of Ophthalmology Symposium held in February, I asked the approximately 200 attendees, “If you were having cataract surgery today, would you choose the femtosecond laser or your traditional cataract surgery?”10 All but one person raised their hands in favor of the femtosecond laser. Many of them were not even performing femtosecond cataract surgery but indicated they would prefer it for themselves. To me that indicates that even surgeons who are not willing to invest in a femtosecond laser now believe it is the technology of the future. I believe the femtosecond laser will help us integrate specialized treatment programs so that each patient can have a custom cataract surgery.
Dr. Wörtz: Will implementing femtosecond laser technology help the general population of all cataract patients? I think the clear answer is yes. By making multiple steps of the surgery precise, we can deliver excellent outcomes for most of our patients.
Conclusion
Dr. Waring: I want to thank all of our panelists for sharing their pearls and experiences with FLACS with the CATALYS Precision Laser System. I think we all agree that performing cataract surgery with the assistance of a femtosecond laser is an exciting new chapter in our field. Having image guidance alone for the first time is a game-changer. Just imagine where we will be in 5 or 10 years. I personally believe that we will be using femtosecond laser technology for a majority of cases in cataract surgery and lens surgery in general.
1. 2015 Market Scope. The Millennial Eye Poll Report for Bryn Mawr Communications.
2. 2016 Market Scope. Cataract Equipment Report.
3. ASCRS Clinical Survey 2016.
4. ASCRS Clinical Survey 2016.
5. O’Meara, Madeleine C, et al. “Laser Capsulotomy.” Textbook of Refractive Laser Assisted Cataract Surgery (ReLACS). Ed. RR. Krueger et al. Springer, New York: Springer Science+Business Media, LLC 2013. 79-99
6. Day AC, Gartry DS, et al. Efficacy of anterior capsulotomy creation in FLACS. J Cataract Refract Surg. 2014;40(12):2031-2034.
7. Bala C, Xia Y, et al. Electron microscopy of laser capsulotomy edge: interplatform comparison. J Cataract Refract Surg. 2014;40:1382-1389.
8. Talamo J. et al. Optical patient interface in femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2013;39(4):501-510.
9. Culbertson D. Why Use a Femtosecond Laser for Incisions? Presented at ESCRS; September 2012; Milan, Italy.
10. Academy of Ophthalmology Symposium. February 10-11, 2017; New Orleans, Louisiana.
INDICATIONS: The OptiMedica CATALYS Precision Laser System is indicated for use in patients undergoing cataract surgery for removal of the crystalline lens. Intended uses in cataract surgery include anterior capsulotomy, phacofragmentation, and the creation of single plane and multi-plane arc cuts/incisions in the cornea, each of which may be performed either individually or consecutively during the same procedure.
PRECAUTION: Patients must be able to lie flat and motionless in a supine position and able to tolerate local or topical anesthesia.
PRECAUTIONS: The CATALYS System has not been adequately evaluated in patients with a cataract greater than Grade 4 (via LOCS III); therefore no conclusions regarding either the safety or effectiveness are presently available.
INDICATIONS and IMPORTANT SAFETY INFORMATION for the CATALYS® Precision Laser System
ATTENTION: Reference the labeling for a complete listing of Indications and Important Safety Information.
INDICATIONS: The OptiMedica® CATALYS® Precision Laser System is indicated for use in patients undergoing cataract surgery for removal of the crystalline lens. Intended uses in cataract surgery include anterior capsulotomy, phacofragmentation, and the creation of single-plane and multi-plane arc cuts/incisions in the cornea, each of which may be performed either individually or consecutively during the same procedure.
CONTRAINDICATIONS: The CATALYS® System is contraindicated in patients with corneal ring and/or inlay implants, severe corneal opacities, corneal abnormalities, significant corneal edema or diminished aqueous clarity that obscures OCT imaging of the anterior lens capsule, patients younger than 22 years of age, descemetocele with impending corneal rupture, and any contraindications to cataract surgery.
WARNINGS: Prior to INTEGRAL GUIDANCE System imaging and laser treatment, the suction ring must be completely filled with sterile buffered saline solution. If any air bubbles and/or a meniscus appear on the video image before treatment, do not initiAte laser treatment. Before initiating laser treatment, inspect images created from the OCT data, surface fits, and overlaid pattern in both axial and sagittal views, and review the treatment parameters on the Final Review Screen for accuracy. Safety margins for all incisions are preserved only if Custom Fit Adjustments to ocular surface(s) are applied in accordance with the instructions for use. Purposeful misuse of the Custom Fit Adjustment to ocular surfaces can result in patient injury and complication(s), and therefore must be avoided. Standard continuous curvilinear capsulorrhexis (CCC) surgical technique must be used for surgical removal of the capsulotomy disc. The use of improper capsulotomy disc removal technique may potentially cause or contribute to anterior capsule tear and/or a noncircular, irregularly shaped capsulotomy. Verify that the suction ring is correctly connected to the disposable lens component of the LIQUID OPTICS Interface during the initial patient docking procedure.
PRECAUTIONS: The CATALYS® System has not been adequately evaluated in patients with a cataract greater than Grade 4 (via LOCS III); therefore no conclusions regarding either the safety or effectiveness are presently available. Cataract surgery may be more difficult in patients with an axial length less than 22 mm or greater than 26 mm, and/or an anterior chamber depth less than 2.5 mm due to anatomical restrictions. Use caution when treating patients who may be taking medications such as alpha blockers (e.g. Flomax®) as these medications may be related to Intraoperative Floppy Iris Syndrome (IFIS); this condition may include poor preoperative dilation, iris billowing and prolapse, and progress intraoperative miosis. These conditions may require modification of surgical technique such as the utilization of iris hooks, iris dilator rings, or viscoelastic substances. Surgical removal of the cataract more than 30 minutes after the laser capsulotomy and laser lens fragmentation has not been clinically evaluated. The clinical effects of delaying surgical removal more than 30 minutes after laser anterior capsulotomy and laser lens fragmentation are unknown. The LIQUID OPTICS Interface is intended for single patient use only. Full-thickness corneal cuts or incisions should be performed with instruments and supplies on standby, to seal the eye in case of anterior chamber collapse or fluid leakage. Patients who will undergo full-thickness corneal incisions with the CATALYS® System should be given the same standard surgical preparation as used for patients undergoing cataract surgery for the removal of the crystalline lens. During intraocular surgery on patients who have undergone full-thickness corneal incisions with the CATALYS® System, care should be taken if an eyelid speculum is used, in order to limit pressure from the speculum onto the open eye.
Patients who will be transported between the creation of a full-thickness corneal incision and the completion of intraocular surgery should have their eye covered with a sterile rigid eye shield, in order to avoid inadvertent eye injury during transport. Patients must be able to lie flat and motionless in a supine position and able to tolerate local or topical anesthesia.
ADVERSE EFFECTS: Complications associated with the CATALYS® System include mild Petechiae and subconjunctival hemorrhage due to vacuum pressure of the LIQUID OPTICS Interface Suction ring. Potential complications and adverse events generally associated with the performance of capsulotomy and lens fragmentation, or creation of a partial-thickness or full-thickness cut or incision of the cornea, include: Acute corneal clouding, age-related macular degeneration, amaurosis, anterior and/or posterior capsule tear/rupture, astigmatism, capsulorrhexis notch during phacoemulsification, capsulotomy/lens fragmentation or cut/incision decentration, cells in anterior chamber, choroidal effusion or hemorrhage, conjunctival hyperemia/injection/erythema/chemosis, conjunctivitis (allergic/viral), corneal abrasion/depithelization/epithelial defect, corneal edema, cystoid macula edema, Descemet’s detachment, decentered or dislocated intraocular lens implant, diplopia, dropped or retained lens, dry eye/superficial punctate keratitis, edema, elevated intraocular pressure, endothelial decompensation, floaters, glaucoma, halo, inflammation, incomplete capsulotomy, intraoperative floppy iris syndrome, iris atrophy/extrusion, light flashes, meibomitis, ocular discomfort (e.g., pain, irritation, scratchiness, itching, foreign body sensation), ocular trauma, petechiae, photophobia, pigment changes/pigment in corneal endothelium/foveal region, pingueculitis, posterior capsule opacification, posterior capsule rupture, posterior vitreous detachment, posteriorly dislocated lens material, pupillary contraction, red blood cells in the anterior chamber (not hyphema), residual cortex, retained lens fragments, retinal detachment or hemorrhage, scar in Descemet’s membrane, shallowing or collapsing of the anterior chamber, scoring of the posterior corneal surface, snail track on endothelium, steroid rebound effect, striae in Descemet’s, subconjunctival hemorrhage, thermal injury to adjacent eye tissues, toxic anterior shock syndrome, vitreous in the anterior chamber, vitreous band or loss, wound dehiscence, wound or incision leak, zonular dehiscence. CAUTION: Federal law (USA) restricts this device to sale by or on the order of a physician. The system should be used only by qualified physicians who have extensive knowledge of the use of this device and have been trained and certified.
CAUTION: Federal law (USA) restricts this device to sale by or on the order of a physician. The system should be used only by qualified physicians who have extensive knowledge of the use of this device and have been trained and certified.
CATALYS, OPTIMEDICA, and LIQUID OPTICS are trademarks owned by or licensed to Abbott Medical Optics, its subsidiaries or affiliates.
All other trademarks are the intellectual property of their respective owners.
© 2017 Abbott Medical Optics Inc.
PP2017CT1312



