Pseudophakic monovision is the most commonly used strategy to provide increased depth of focus after bilateral cataract surgery,1 but the optimal degree of anisometropia has long been debated. Some argue that a difference of 2.00 to 3.00 D between the distance eye and near eye is required for adequate distance and reading vision. Others point out that this interocular difference can be too much for patients to tolerate, risking binocular inhibition, reduced contrast sensitivity, and a loss of stereopsis. So-called modest monovision, which aims for emmetropia in the distance eye and approximately -1.25 D in the near eye, has been shown to offer the best of both worlds, with a good level of spectacle freedom for most tasks and a minimal risk of anisometropic symptoms.2
Whichever approach is taken, an accurate refractive outcome for each eye is essential. This may appear to be as simple as using standard IOL calculation formulas and selecting an IOL that targets the required myopic outcome. IOL calculation methods, however, were designed and validated to achieve emmetropia. It has not previously been determined whether they work as effectively with nonemmetropic targets. This also has relevance for myopic patients who wish to remain bilaterally myopic postoperatively.
After concerns about the validity of IOL calculation methods for nonemmetropic targets were raised in an ASCRS EyeConnect forum discussion, we decided to investigate this matter. This article describes our findings.
METHODOLOGY
In a retrospective paired-eye study,3 we identified consecutive patients who had undergone bilateral, sequential cataract surgery performed by one of us (G.D.B.) with a plan of modest monovision. In our practices (A.M.J.T. and G.D.B.), patients with good binocular visual potential who desire greater spectacle independence are routinely offered modest monovision. For the purposes of this study, only patients who underwent bilateral in-the-bag implantation of an AcrySof IQ Toric IOL (model SN6ATx, Alcon) were included to avoid confounding from different IOL platforms. Patients with vision-limiting pathology were excluded, as were those with a history of refractive surgery.
A total of 88 patients (176 paired eyes) were included. Using optimized IOL constants to reduce the mean error of the data set to zero, the predicted postoperative refractions of six IOL calculation methods (Barrett Universal II, Hill-RBF version 2.0, Haigis, SRK/T, Holladay I, and Hoffer Q) were derived, with a target of approximately emmetropia in the distance eyes and -1.25 D in the near eyes. These refractions were compared with the subjective spherical equivalent 4 weeks after surgery, as measured by a single optometrist using a 6-meter refracting lane. Prediction error, mean error, median absolute error, standard deviation, and percentage within ±0.50, ±0.75, and ±1.00 D of target for each method were then calculated in the usual manner.
RESULTS
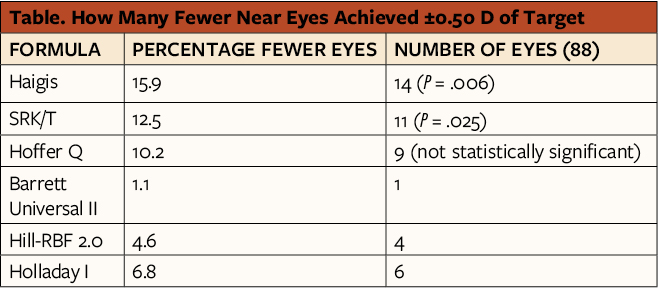
Overall, outcomes in the near-eye subgroup were less accurate than those in the distance-eye subgroup for each formula investigated (Figure 1). The formulas most affected were the Haigis and SRK/T, with 15.9% (14/88; P = .006) and 12.5% (11/88; P = .025) fewer near eyes, respectively, achieving within ±0.50 D of target. Using the Hoffer Q formula, 10.2% (9/88) fewer near eyes achieved the refractive target, but this difference was not statistically significant. The methods least affected were the Barrett Universal II, Hill-RBF 2.0, and Holladay I, with 1.1% (1/88), 4.6% (4/88), and 6.8% (6/88) fewer near eyes, respectively, achieving the refractive target; these differences were not statistically significant. Mean error, median absolute error, and standard deviation were consistently worse for the near eyes across all methods investigated (Table).
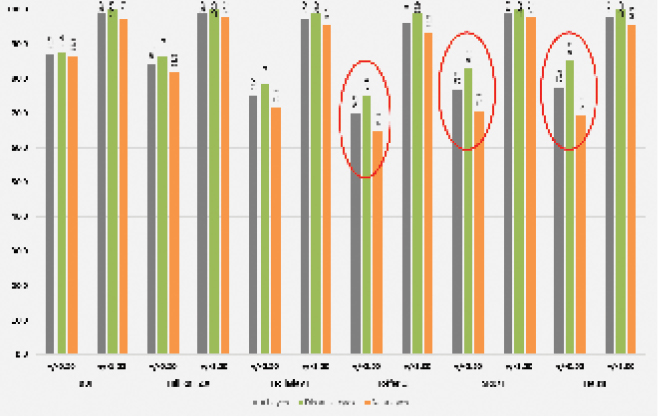
Figure 1 | Percentage of eyes within ±0.50 and ±1.00 D of target, comparing the whole data set with the distance- and near-eye subgroups. Red circles indicate those formulas where there was a clinically important difference in refractive accuracy between the distance and near eyes.
DISCUSSION
When surgeons plan for pseudophakic monovision, they need accurate IOL power calculation methods that can be applied to the distance eye and the near eye. Confirming suspicions raised by earlier studies,4-6 our study showed that reduced refractive accuracy can be anticipated with low myopic targets.
The precise reason for this is unclear. One possible explanation is that a higher-powered IOL is usually required in the near eye (Figure 2). If the effective lens position prediction in each pair of eyes is assumed to be the same due to interocular symmetry, the same effective lens position error will have a proportionally greater impact on a higher-powered IOL. Alternatively, there may be a fundamental difference in the DNA of IOL calculation methods when outcomes other than emmetropia are targeted.
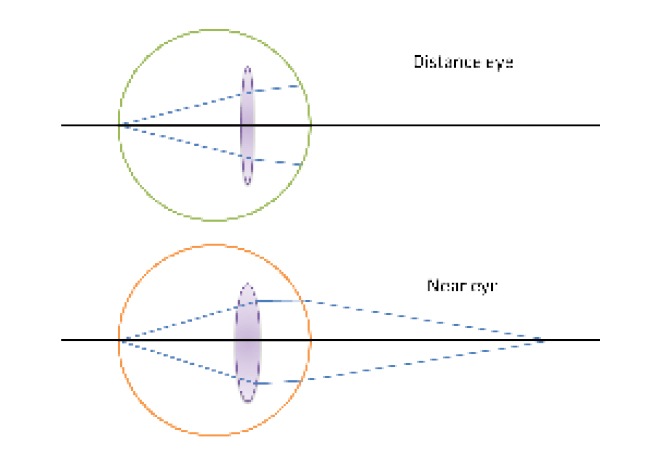
Figure 2 | Schematic demonstrating the difference in IOL power required for distance and near eyes when monovision is targeted in symmetrical eyes.
Although we investigated only modest monovision of -1.25 D in the near eye, it may be that these findings can be extrapolated and that the differences worsen progressively with higher myopic targets. The Barrett Universal II, Hill-RBF 2.0, and Holladay I formulas were the least affected by this phenomenon, but the Holladay I was less accurate overall for both distance and near eyes.
Based on these findings, when planning a myopic outcome, cataract surgeons should use the Haigis, SRK/T, and Hoffer Q formulas with caution regardless of whether this is in the context of monovision. With almost equivalent accuracy for distance and near eyes, the Barrett Universal II and Hill-RBF 2.0 offer reliable options for a patient desiring a refractive outcome of either monovision or bilateral myopia.
1. Balgos MJTD, Vargas V, Alió JL. Correction of presbyopia: an integrated update for the practical surgeon. Taiwan J Ophthalmol. 2018;8(3):121-140.
2. Naeser K, Hjortdal JØ, Harris WF. Pseudophakic monovision: optimal distribution of refractions. Acta Ophthalmol. 2014;92(3):270-275.
3. Turnbull AMJ, Hill WE, Barrett GD. Accuracy of intraocular lens power calculation methods when targeting low myopia in monovision. J Cataract Refract Surg. 2020;46(6):862-866.
4. Geggel HS. Comparison of formulas and methods for high myopia patients requiring intraocular lens powers less than six diopters. Int Ophthalmol. 2018;38(4):1497-1504.
5. Dalto RF, Ferreira MA, Queiroz W, Coelho RP, Paula JS, Messias A. Haigis and SRKT formulae accuracy for intentional myopic overcorrection. Int Ophthalmol. 2018;38(4):1459-1463.
6. Ple-Plakon PA, Wang L, Koch DD. Refractive outcomes in monovision: comparison of IOL calculations with distance, intermediate and near targets. Paper presented at: ASCRS Annual Meeting; April 20, 2015; San Diego.





