The interface between the air and tear film is the most important refractive interface in the visual system. It is therefore understandable that, when considering the origin of refractive astigmatism, surgeons often assume that the magnitude and axis of refractive astigmatism directly corresponds to keratometry. Although the anterior corneal astigmatism measured by keratometry contributes the majority of astigmatism measured on refraction, astigmatism arising from sources posterior to the anterior corneal surface is also clinically important.
Non-anterior corneal astigmatism is also called intraocular astigmatism or lenticular astigmatism, but it is effectively quantified by magnitude and axis as the vector value of ocular residual astigmatism (ORA). ORA may arise from any source posterior to the anterior corneal surface, including the posterior corneal surface, anterior surface of the crystalline lens, posterior surface of the crystalline lens, or vitreous. ORA may also be the result of the sum of higher-order aberrations, which result in low-order cylinder that is measurable with subjective refraction. In unusual cases, manifest refractive astigmatism may also arise from the visual cortex, in that patients may subjectively prefer cylinder in their refractions when, in fact, optically it is not present.
WHY IS THIS IMPORTANT?
In LASIK procedures, the refractive error is corrected on the anterior corneal surface, regardless of the source of the refractive error. For example, if a patient has 1.00 D of astigmatism arising from the crystalline lens, but 0.00 D of corneal astigmatism as measured by keratometry, the LASIK procedure will correct the 1.00 D of astigmatism on the surface of the eye. The formerly spherical cornea will now have 1.00 D of corneal astigmatism in a meridian opposite the lenticular astigmatism. This may be acceptable for small magnitudes of ORA, but for higher amounts it may result in unsatisfactory vision (Figures 1 and 2).
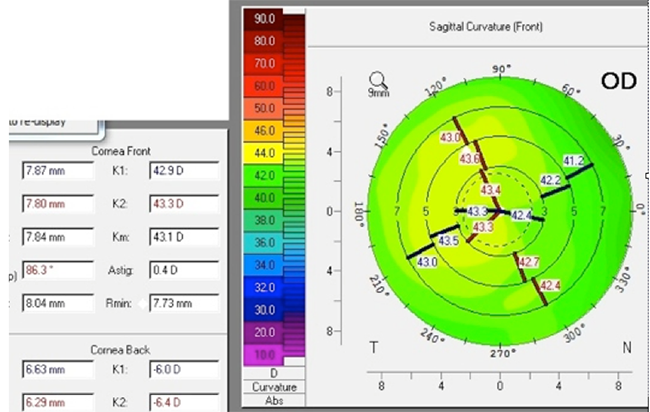
Figure 1. This patient had 0.40 D of corneal astigmatism prior to LASIK but a refraction of plano -1.50 x 095.
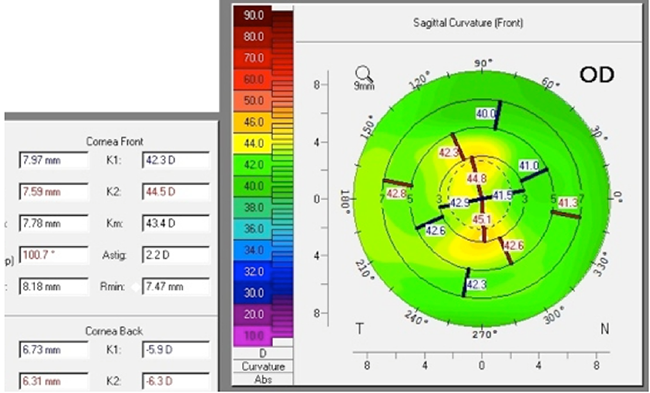
Figure 2. Postoperatively, the cornea has 2.20 D of astigmatism. The refraction is plano sphere, but the patient is not happy with visual quality and has night glare.
WHAT DO I NEED TO DO ABOUT THIS?
The key take-home point is that surgeons should be thinking about the source of astigmatism when considering a plan to treat it. If significant astigmatism is arising from an intraocular source, then correcting the problem on the corneal surface with LASIK may not be ideal. During the refractive surgery evaluation process, it is important to compare refractive astigmatism to topographic and keratometric values. If they do not align in axis or magnitude, then further investigation is warranted.



