Watch a short introductory video from Dr. Whitley to learn more about this article.
Introduction and Objectives
Vitreous opacities (VO) are microscopic collagen fibers within the vitreous that tend to clump and cast shadows on the retina appearing as floaters to the patient. The most common cause of VO is posterior vitreous detachment (PVD), a separation of the posterior hyaloid face from the retina.1 VO are not usually visually threatening, but they may significantly affect visual function. In the absence of more serious underlying pathology, many patients may not experience significant persistent visual impairment from VO. For some patients, the symptomatic effects of VO may persist and become burdensome. These are referred to as symptomatic vitreous opacities (SVO) (Figures 1 and 2). Treatment options are available, and the most commonly reported option is vitrectomy.2
Figure 1. An artistic depiction of SVO illustrated by Marielle Mahan, MD, an ophthalmology resident at MedStar Georgetown University Hospital/Washington Hospital Center in Washington, D.C.
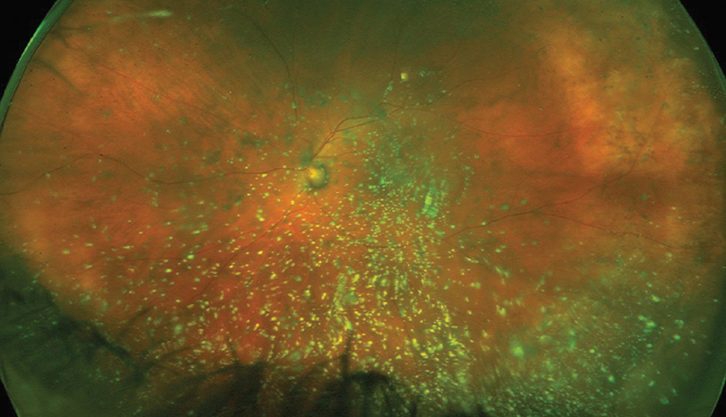
Figure 2. Ultrawide-field photograph taken on the Optos platform depicting asteroid hyalosis in a patient presenting with SVO.
Image courtesy of Maria H. Berrocal, MD, originally published in D’Amico D, Berrocal M, Ho A, et al. Vitreous opacities: current trends and treatment strategies. Retina Today. July/August 2021.
Vitrectomy for the management of severe VO is becoming increasingly accepted because of the tremendous relief of symptoms reported by patients. The risks of retinal tear and detachment remain a concern, particularly in patients who have an attached posterior hyaloid.3 However, small-gauge vitrectomy is a minimally invasive way of removing the VO. The peer-reviewed literature demonstrates vitrectomy is well tolerated and highly effective at improving vision, symptoms, contrast sensitivity, and quality of life.4 In the United States, patients with VO require a referral to a vitreoretinal surgeon to determine if vitrectomy is an appropriate option. However, the referral practices of eye care professionals are not well understood. An online survey was recently deployed and completed by 339 US-based eye care professionals to determine to what degree patient populations are impacted by VO and how often these patients are referred to retina specialists for further care. An expert panel was convened to provide a balanced review of these data and the implications from the optometrist, ophthalmologist, and retina specialist perspectives. The objectives for the workshop discussion included:
- Reviewing survey findings indicating that when patients present to eye care professionals with SVO, they are not typically referred to retina specialists
- Discussing the barriers to referral and potential tools to facilitate the process
- Providing consensus-based recommendations to bolster the referral of patients with SVO to help optimize their care
- Establishing that surgery may be an appropriate option for some patients with SVO
Survey Findings on Current Views of VO Among Eye Care Professionals and Referral of Patients to Retina Specialists in the United States
In June 2021, an online survey was sent to those in the Bryn Mawr Communications database to better understand the perceptions of VO. A subset of eye care professionals was analyzed to also assess the referral process for further care in the United States. Key findings are summarized in the infographic in Figure 3.
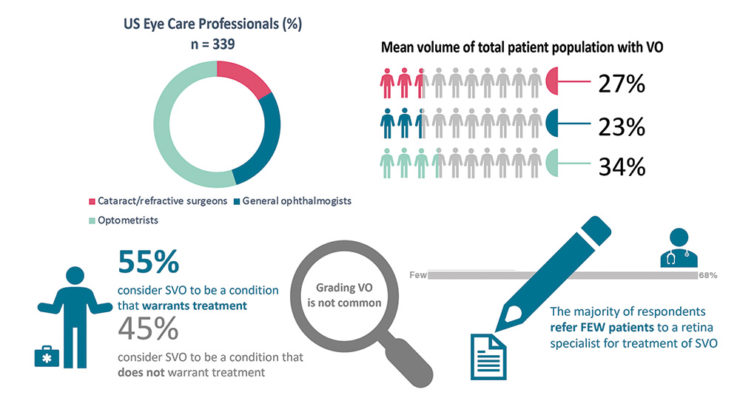
Figure 3. An infographic summary of key survey findings of US eye care professionals and their views on VO and referring practices.
There was an unprecedented response to the survey with 339 US respondents, of which 15% were cataract and refractive surgeons, 26% were general ophthalmologists, and 50% were optometrists. The volume of patients reported presenting with VO to the eye care professional respondents was substantial.
- Optometrists reported that approximately 34% of their total patient population is comprised of patients with VO, cataract surgeons reported approximately 27%, refractive surgeons reported approximately 26%, and ophthalmologists reported approximately 23%.
- Interestingly, when asked whether SVO are considered a condition that warrants treatment, across specialties respondents were basically split—55% answered ‘yes treatment is warranted’ and 45% answered ‘no’.
- Additionally, when assessing patients with VO, the majority of eye care professionals do not grade the severity of their patients’ opacities. However, 45% of the optometrist respondents and 31% of the cataract surgeons reported grading their patients’ VO (Figure 4).
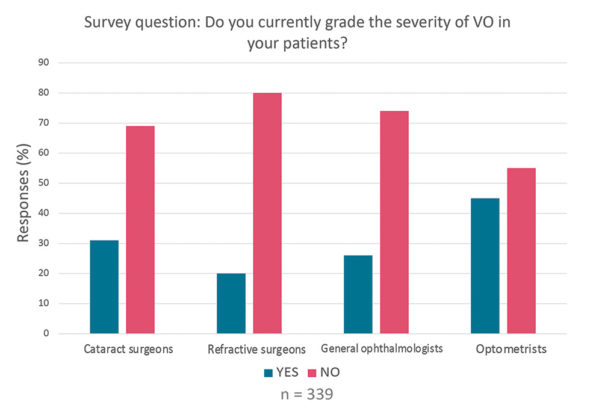
Figure 4. Survey findings of US eye care professionals on grading VO severity.
When asked about how many of their patients with VO are referred to a retina specialist, 68% responded that they refer ‘few’ patients, and 22% responded that they refer ‘some’ patients, while 8% reported that they refer ‘none’ of their patients (Figure 5).
An expert panel was convened to represent the eye care professionals who completed the survey. They took a closer look at the survey findings and discussed how to facilitate the referral of patients with SVO to a retina specialist for potential surgical intervention. Dr. Whitley moderated a discussion about the survey data.
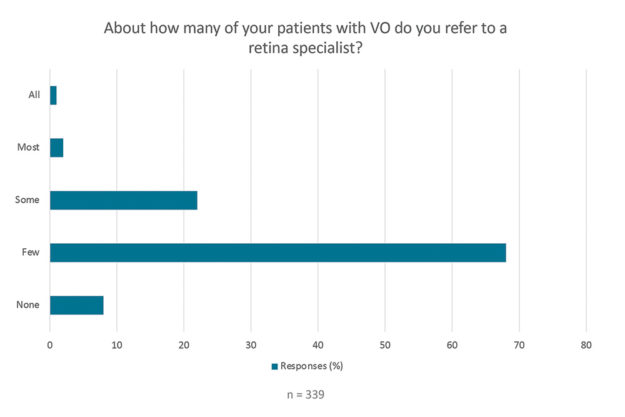
Figure 5. Survey findings show the majority of US eye care professional respondents refer FEW patients to a retina specialist for treatment of SVO.
Positive Feedback Loop for SVO
Dr. Gerson commented that the only data that surprised him were the volume of patients with VO (27%) presenting to cataract surgeons. He expected this number to be higher given the potential for patient confusion between cataract and VO symptoms. Dr. Kitchens was not surprised that the volume of patients presenting to optometrists was the highest. He noted that as a retina specialist, he often has patients with VO referred to him by local optometrists. In his experience, optometrists have long-standing relationships with their patients and have important conversations to determine if their patients are bothered by VO. Dr. Kitchens also noted that there is a positive feedback loop so that when patients with SVO are referred and he performs vitrectomy, the patients eventually return to their optometrists and convey that they are thrilled with the results. Dr. Early agreed, noting that there is a positive feedback loop with referrals involving cataract patients and SVO.
Dr. Gerson said that as an optometrist, he often hears about symptoms such as VO from his patients. But he noted that he is not aware of retina specialists in his area routinely treating SVO with vitrectomy. If he was aware of this treatment option being available, he would be more likely to mention it to his patients and refer them. Dr. Gerson also noted that he is aware of laser vitreolysis as an option for his patients with SVO. Dr. Weng agreed that retina specialists may not “market” vitrectomy for the treatment of SVO. She noted that eye care professionals have been conditioned overall to not consider vitrectomy but that the experience and evidence base has grown in recent years due to surgical technology improvements underscoring the need to revisit the benefits and safety of surgery for SVO. Dr. Whitley asked Dr. Haynes if she thought grading VO severity would facilitate the referral of patients with SVO to a retina specialist. She noted that, given the volume of patients with VO presenting to optometrists, if the complaint is not taken seriously and graded with consideration of the impact on the patient’s quality of life (QoL), those who are really bothered and could benefit from referral and treatment can be missed.
Establishing a VO Severity Grading System
In previous panel discussions, definitions were proposed to help encourage and guide grading the severity of VO.
- A patient with asymptomatic VO has no visual disturbances. The VO are rarely noticeable and can be picked up in clinical exam, but the patient may not be aware of them.
- Mild severity refers to VO that are noticeable to the patient, but they are just slightly bothersome and do not interfere with vision or functions of daily living such as working or driving.
- Moderate severity refers to VO that are bothersome enough to impact vision and interfere somewhat with functions of daily living such as working or driving.
- Severe VO are extremely bothersome and highly impact QoL by significantly interfering with functions of daily living such as working or driving.
The majority of survey respondents agreed that these definitions were appropriate to facilitate grading VO severity. The definitions were vetted by a retina specialist working group who concluded that only patients with moderate or severe SVO should be referred to a retina specialist.
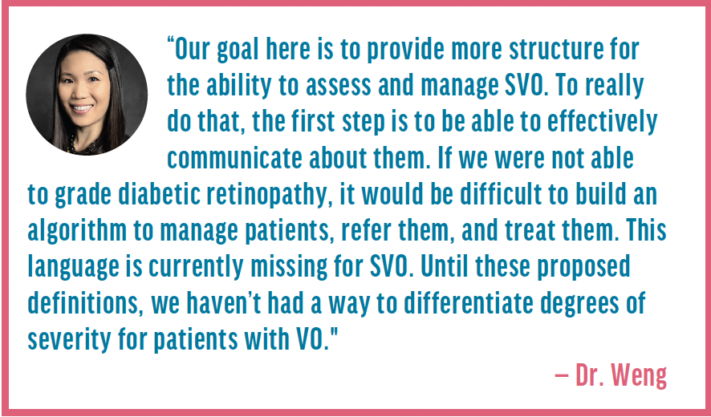
Dr. Weng asked the panel if they agreed with the proposed definitions, and there was consensus. Dr. Early noted that defining the severity of VO is less straight-forward than assessing anterior chamber cell, for example, which has a discrete, stepwise, incremental grading scale. But with VO, the subjective aspect is a very important part of severity. She stated that grading a cataract is more of a hybrid approach, where appearance is graded as well as the activities of daily life, and both help in the decision to propose cataract surgery. VO are different because of the significance of the subjective complaint since what is seen upon exam does not always correlate with the impact of the VO on the patients and their QoL. Dr. Weng noted that the definitions help to provide simple necessary language to quickly understand the severity scale of VO in the absence of a specific objective component. They may evolve over time or be somewhat customized by the eye care professionals who use them. She expects that with time and peer-to-peer education, they will be refined. She also emphasized they do not take into account the duration of symptoms, which is important and should also be considered when determining if a referral is warranted. Dr. Kitchens agreed about the importance of duration since a patient could present with severe SVO after a PVD or cataract surgery, and these postoperative SVO can improve over time. He added that there is not a diagnostic test for VO, so it involves asking patients a lot of questions and is a more subjective process. Dr. Haynes stated that the proposed grading scale addresses the functions of daily living and using that information in the context of what is observed in the clinical exam makes it a helpful tool to identify patients with SVO whom should be referred and potentially treated.
SVO Referral Form
The panel worked on a one-page SVO referral form (see Symptomatic Vitreous Opacity Referral Form) suitable for use by ODs and MDs for their patients that will capture key information by the patient and the referring eye care professional to facilitate subsequent evaluation by the retina specialist. Dr. Early commented on the importance of making the referral form as simple to complete as possible and including only pertinent details. She suggested including the definitions of VO severity and allowing the referring eye care professional to circle the patient’s grade. Dr. Kitchens and Dr. Haynes agreed with this approach and suggested including boxes that the referring eye care professional could easily check to convey the affected eye(s) and relevant patient history (e.g., acute PVD, dry eye, use of eye drops, etc.). Dr. Kitchens clarified that checking the box on the form indicating a history of dry eye, for example, is providing the retina specialist with useful information and context; it is not exclusion criteria for SVO treatment. Dr. Weng discussed the importance of capturing the duration of symptoms on the form. She said it was important to include when the patient first noticed the VO in a continuous timeframe (e.g., less than 3 months ago, 3-6 months ago, etc.), so it is easier for the patient to gauge. Ultimately, the duration of symptoms is often a key factor in the retina specialist’s decision about whether a patient with SVO is a surgical candidate. Dr. Gerson agreed and said that eye care professionals may be surprised to find that many patients may indicate they have been experiencing symptoms for more than 1 year. Dr. Weng and Dr. Early stated that it would be helpful for the referring eye care professional to fill in key relevant exam findings and that other details will already be captured in the patient’s chart that would accompany the referral form.
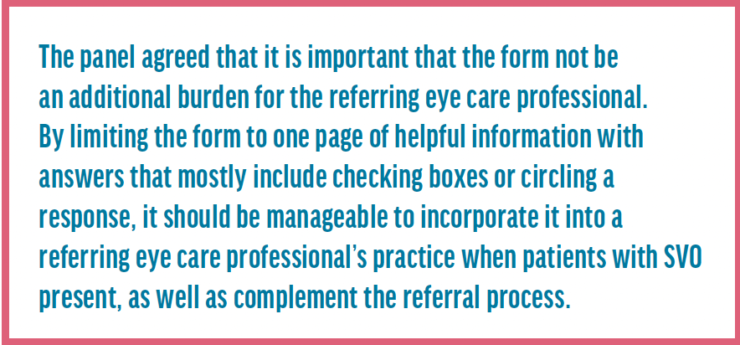
The referral form is customizable by eye care professionals' practices upon download. In terms of the practical use of the form, Dr. Haynes explained that the patient would complete the top of the form through question 6. Then the referring eye care professional would complete the remainder of the form, which would be faxed to the retina specialist with a copy of the patient’s chart. Dr. Haynes said that if the form is completed by the referring eye care professional, it is educational, providing guidance on VO, and creates a more meaningful referral for SVO. Dr. Early agreed that the form helps ensure the use of the same terminology and education, opening that communication channel between eye care professionals. Dr. Kitchens and Dr. Gerson noted that a technician or staff member in the referring eye care professional’s office could also complete the form and add it to the patient’s chart to create the referral. Dr. Early noted that ideally the form could be leveraged within a facility’s electronic medical record system. Dr. Whitley said that this form would help streamline the referral process in his practice. Figure 6 depicts a hypothetical example of how the form could be used.
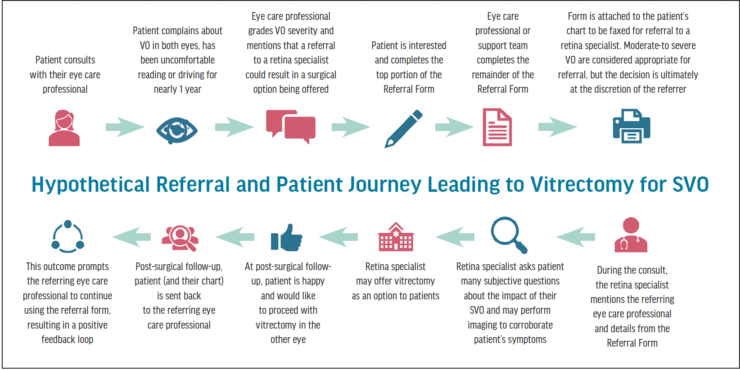
Figure 6. Hypothetical example of how the form could be used to facilitate referrals to a retina specialist.
Dr. Weng said that the form has additional benefits.
- It helps patients with SVO feel like their symptoms are being validated, which is important since historically VO have been dismissed as a part of aging.
- It streamlines the communication between the two physicians, strengthening the collaborative bond between retina specialists and their colleagues, and gives patients additional confidence in their care.
Dr. Weng acknowledged that not all retina specialists perform vitrectomy for SVO and that we are in the midst of a culture shift where some eye care professionals may still be resistant to the idea of surgery for SVO. She said that more discussion about VO with the necessary context of the severity scale will help spread awareness of a surgical option for SVO to ensure that the referral has the potential to really help the patient. Dr. Kitchens agreed. He also noted that not all the retina specialists in each practice may offer vitrectomy for SVO. So, if a referral of a patient with SVO is received, it should be routed to the specialist who offers that option and not kicked back to the referring eye care professional. Dr. Early also agreed and noted that patient education is also key. Patients are increasingly health literate and internet savvy. They will want to know about the outcomes associated with vitrectomy for SVO and that it is a low-risk option. She also noted that even young ophthalmologists recently out of training in the past few years may not be familiar with vitrectomy as an option for SVO, so education for both patients and eye care professionals is needed.
Symptomatic Vitreous Opacity Referral Form. To see a customizable and downloadable version, go to: eyetube.net/editorial-feature/vitreous-opacities
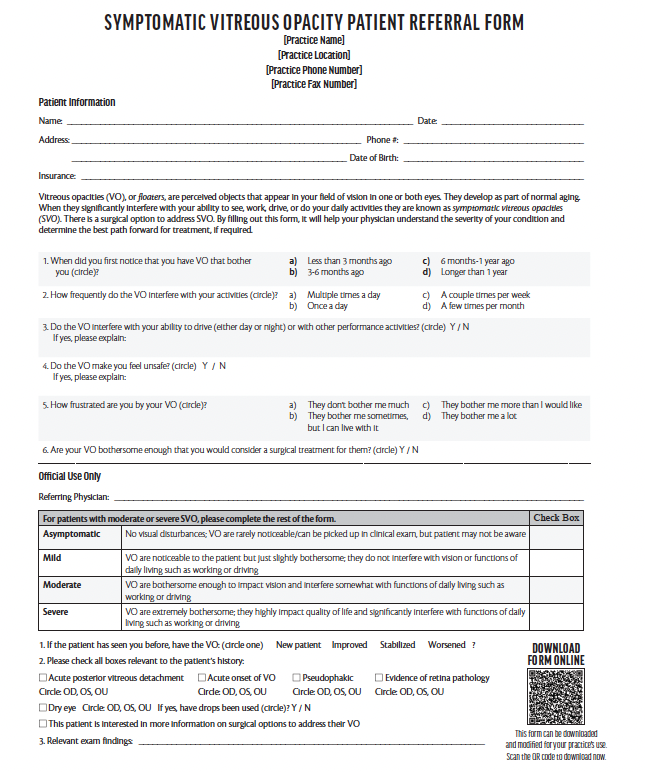
Interpreting the SVO Referral Form
The panel discussed a hypothetical completed referral form and what would stand out as criteria for consideration of vitrectomy for SVO. Dr. Weng said that for her, timing is important, and if a patient is bothered by symptoms for more than 6 months, that vitrectomy could be a great option. Of course, she takes many factors into consideration, but generally a severity of moderate-to-severe for at least 6 months makes a patient with SVO a potential vitrectomy candidate.
Potential Red Flags for Retinal Detachment
Dr. Early and Dr. Haynes discussed that the referral form should not be used to refer patients experiencing acute symptoms or new onset of VO. Dr. Kitchens agreed that if the form indicates that a patient has acute symptomatic PVD and flashes/opacities of acute onset or concern for retinal detachment, that they are red flags that warrant immediate attention. Recipients of the faxed referral form at the retina specialist office should be trained that if those boxes are marked on the referral form, that the patient should be seen within a few days. Dr. Weng and Dr. Kitchens agreed that when the referral form is received by them, it would prompt the patient being scheduled for a consult, even if the form is not completely populated. It would signal to them that a colleague thinks a patient needs further care, so they would assess the patient accordingly.
Vitrectomy for SVO: Images From a Recent Case
Dr. Kitchens shared imaging from a recent patient with SVO who was referred to him. In his clinic, new patients with VO must receive Optos imaging and OCT. Optos imaging provides views of the peripheral retina and allows him to identify VO, which are shown to the patient. Some of the VO in the left eye are visible in Figure 7; there were VO more overlying the patient’s macula.

Figure 7. Optos imaging of some of the SVO that were bothering Dr. Kitchens' patient’s left eye.
Dr. Kitchens also found a peripheral horseshoe tear in this patient that was lasered, and he proceeded with vitrectomy to remove the SVO. Dr. Weng said that the tear would have made her pause and very carefully consider whether to proceed with vitrectomy. She would be concerned about creating a retinal break or detachment intraoperatively. She noted she would not rule out vitrectomy, but she would carefully assess and discuss the risks thoroughly with the patient to arrive at a decision in this type of case. Dr. Kitchens emphasized how helpful Optos imaging is in assessing about 90% of the retina and that its use began in the optometrist’s office. The eye care professionals on the panel guessed that across the United States, between 10% and 30% of optometrists’ offices probably have Optos imaging. For those with this tool, it could help corroborate patients’ SVO symptoms and aid in the decision to refer the patient to a retina specialist.
Watch it Now
A Path Forward: Comanaging Patients With SVO
OCT helps Dr. Kitchens to rule out macular pathology. He has found that asymptomatic epiretinal membrane is not a contraindication for vitrectomy for SVO, but he wants to know if it is there and discusses the potential implications with his patients. In his experience, about 10% of asymptomatic epiretinal membranes will progress and need to be removed after removing SVO. He also prefers to confirm if the patient has a vitreous separation—sometimes there’s vitreous insertion at the nerve. In this patient’s left eye, the SVO are visible on the OCT of the reference scan in Figure 8.
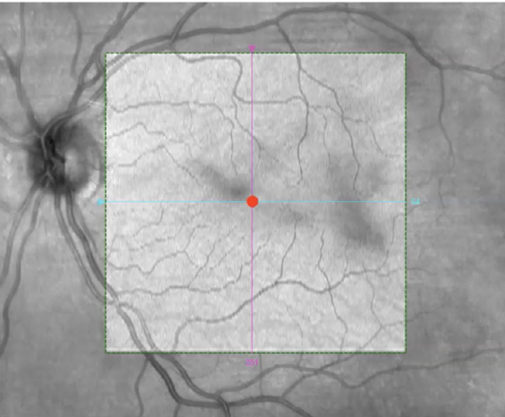
Figure 8. OCT of some of the SVO that were bothering Dr. Kitchens' patient’s left eye.
Dr. Kitchens noted that following SVO removal, he depresses peripherally under wide-field viewing before removing instruments to find any retinal breaks or tears. Antibiotic ointment twice a day for 1 week is then prescribed. He stated that when not working with the iris or anterior segment, the rates of cystoid macular edema are very low with vitrectomy. A patch, shield, and limited activities are also recommended for about 1 week. Dr. Kitchens is very quick to return patients back to their referring eye care professionals after a 1-week postoperative follow-up. The second eye may be done within 2-3 weeks of their first eye.
Dr. Early asked if Dr. Kitchens received any feedback from referring eye care professionals indicating a change in refractive outcomes in patients with premium IOLs following vitrectomy. He noted that he has not received such feedback. Dr. Weng said that in her experience, a small fraction of her patients experienced refractive shift. However, those few patients were still very satisfied following vitrectomy for SVO because it is a very minor shift (usually a quarter to a half diopter).
Conclusions
- Overall, the panel of eye care professionals agreed that the US survey data signaled a gap in the monitoring of VO severity as well as a tendency to not refer patients with SVO to a retina specialist, despite a high volume of patients presenting with these symptoms.
- The VO Severity Grading System will help introduce a working lexicon around VO and identify patients that may benefit from a referral to a retina specialist and potential vitrectomy to remove the SVO.
- Further, the SVO referral form will facilitate the referral process as an easy-to-use tool that can be populated quickly to accompany patients’ charts highlighting why patients may be appropriate candidates for surgery.
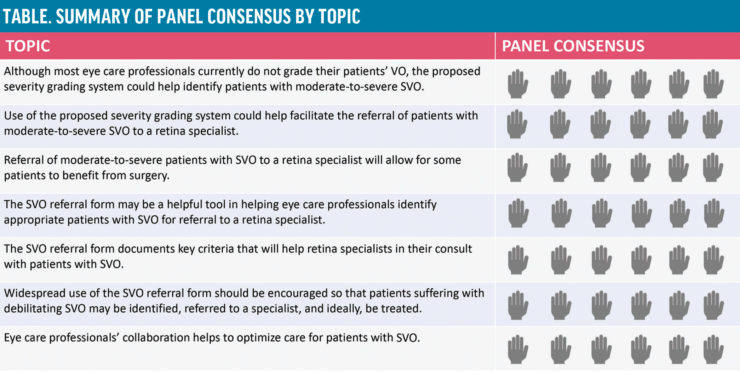
- The panel came to consensus on some key topics addressed during the discussion demonstrating how collaboration and communication can help benefit patient care for SVO. The Table summarizes the panel’s views by topic.
Acknowledgements
Medical writing and editorial support by Susan Cuozzo, CMPP, and A2E Communications Group.
1. Bergstrom R, Czyz CN. Vitreous floaters. 2022. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. 2022. PMID:29262091.
2. Broadhead GK, Hong T, Chang AA. To treat or not to treat: management options for symptomatic vitreous floaters. Asia Pac J Ophthalmol (Phila). 2020;9(2):96-103.
3. Ryan EH. Current treatment strategies for symptomatic vitreous opacities. Curr Opin Ophthalmol. 2021;32(3):198-202.
4. Sommerville DN. Vitrectomy for vitreous floaters: analysis of the benefits and risks. Curr Opin Ophthalmol. 2015;26(3):173-176.











