In the past 5 to 10 years, corneal collagen crosslinking (CXL) via ultraviolet (UV) light and riboflavin administration has been shown domestically—and even more so internationally—to be an effective treatment option to halt and flatten the steepening effects of corneal ectasias (ie, keratoconus, post-LASIK/PRK ectasia). Several European studies have demonstrated its efficacy with the “standard treatment” (epithelium off, topical riboflavin 0.1% for 30 minutes followed by exposure to UV light at 3 mW for 30 minutes), and its continual flattening effects can even be seen beyond 3 years after one treatment.1
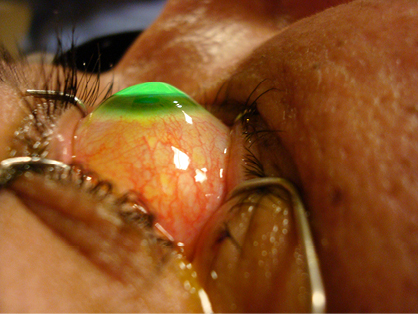
Slit-lamp image of standard, epithelium-off CXL of a patient showing Munson sign keratoconus. Notice the autoflourescence of the riboflavin-saturated corneal stroma. (Photo courtesy of Steven Dell, MD.)
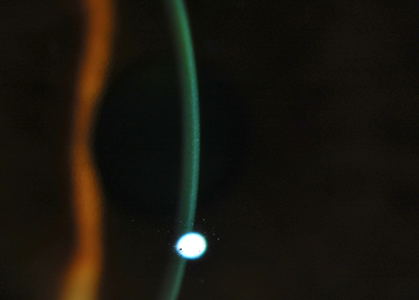
Slit-lamp image of a transepithelial riboflavin treatment. The cornea is well loaded using a proprietary technology. (Photo courtesy of Roy Rubinfeld, MD.)

Slit-lamp image of UVA application during transepithelial CXL. (Photo courtesy of Roy Rubinfeld, MD.)
RAPIDLY EVOLVING THERAPY
CXL is evolving fairly rapidly in treatment regimens, advancements over the standard protocol, and in its applications. Since the main goal of crosslinking the cornea is to increase the corneal rigidity and halt progression, it would seem logical to combine this treatment modality with others that seek to flatten the inferiorly steep keratometry or K values, thus improving corneal irregularity and overall visual acuity. You name a combination of treatment strategies and its being tried, with varied levels of success but all promising modalities nonetheless. A few noteworthy innovative treatment combinations include:
• CXL with topography-guided PRK2,3
• prophylactic CXL with LASIK4
• CXL with ring segments and the riboflavin injected into the intrastromal ring channels5
• Ring segments, followed by CXL with PRK6
Improvements with the actual treatment protocol are also being made, mainly with epithelium-on options and shorter treatment times. Although various trials are evaluating the aforementioned variables, with treatment times as short as 3 minutes, little has been published regarding the results of such trials. Koppen et al demonstrated that benzalkonium chloride-assisted transepithelial CXL was not as effective as the standard protocol at halting the topographic progression of keratoconus in 53 eyes of 38 patients over an 18-month follow-up period.7 Transepithelial CXL appears to be a very viable option with demonstrated efficacy. The positive difference may be a result of how well the riboflavin penetrates into the corneal stroma, and preparations with greater penetration are on the horizon.8 Another option may be a delivery system that drives the riboflavin into the corneal stroma, such as iontophoresis, and we will await such advances.
OTHER APPLICATIONS
Beyond its applications in corneal ectasia therapies, CXL appears to be a rather useful option in other corneal disease management, namely as an adjunctive therapy in infectious keratitis and as a means to treat symptomatic corneal edema. An in vitro study by Martins et al revealed that both riboflavin and UV exposure alone were adequate in killing Staphylococcus aureus, methicillin-resistant S aureus, and Pseudomonas aeruginosa.9 More recently, several studies have demonstrated the ability of photo-activated riboflavin therapy to help cure refractory corneal bacterial ulcers as well as halt ominous corneal thinning from such virulent ulcers, as evidenced by Panda and associates in their case series of seven eyes.10
Lastly, a known side of effect of CXL is that it causes compaction of corneal stromal tissue, and this effect appears to be another treatment direction for CXL. In three patients with Fuchs dystrophy, Hafezi et al demonstrated improved visual acuity, decreased central corneal thickness, and improved diurnal variation of the corneal thickness after CXL.11 As such, CXL may be just the right treatment option for a patient with bullous keratopathy who is either a poor candidate for corneal transplant surgery or is looking for a modality before going to the OR, as Ghanem et al showed that vision, corneal clarity, and ocular pain improved after CXL.12
CONCLUSION
The key message is that CXL is here to stay and will likely continue to sprout more beneficent wings in the near future. Take a gander, as I believe that riboflavin phototherapy will have greater reach in the treatment of various corneal diseases and help prevent—or the very least delay—the need for corneal transplantation for corneal ectasias, ulcers, and edema.
Abstract 1, Abstract 2, Abstract 3, Abstract 4, Abstract 5, Abstract 6, Abstract 7, Abstract 8, Abstract 9, Abstract 10, Abstract 11, Abstract 12



