Have you seen it, too? Recently, I’ve noticed baby boomers using selfie sticks, and not only for their intended purpose. Turns out, a selfie stick functions nicely as an arm extender for presbyopia! Young boomers are all about having the latest technology, staying fit, traveling the world, performing in the boardroom, and having young eyes to match the youth they feel. Given that presbyopia is virtually ubiquitous after age 45, refractive surgery options to address the eye’s loss of zoom capability are now vital tools to meet the needs and demands of this emerging demographic.
One of the most common things I hear from patients goes something like this: “Doctor, it was one thing when I needed glasses to be able to see far, but now that I need help to see up close too, just fix it all.” Bifocals aren’t doing it for their self-image. For many top execs in the boardroom, a simple task like reading and interpreting small print on an important document immediately provides a level of top performance to which they’ve grown accustomed. It’s interesting that presbyopia reduces not only the magnitude of accommodation but also the speed of accommodation. Many of my patients report the need to preserve their ability to see fast and think fast in order to maintain their status in a professional environment.
Enter corneal inlays. With the FDA approval of the Kamra inlay (AcuFocus) last spring, refractive surgeons will need to become comfortable with patient selection, surgical implantation pearls, and, especially in this arena, the need for careful postoperative care. These are by no means “lunchtime LASIK” procedures; they need to be managed accordingly.
THE RAINDROP CORNEAL INLAY
I’ve been involved as a principal investigator with the Raindrop corneal inlay (ReVision Optics) for a little over 3 years. The Raindrop is a 2-mm–diameter, clear, hydrogel disk that is placed under the anterior one-third of the cornea to restore near vision in emmetropic presbyopes. The Raindrop’s mechanism of action is to produce what’s being called a profocal cornea. It essentially creates a reversible form of corneal multifocality, whereby the central cornea steepens for near, a paracentral transition zone provides a good level of intermediate vision, and the peripheral cornea is maintained for distance. The Raindrop is placed in the nondominant eye and, in clinical trials, has been shown to provide an immediate “wow” factor, often with J1 or even J1+ near acuity on day 1.

The Raindrop measure 2mm in diameter.
Given that the Raindrop and most other corneal inlays being studied are placed only in the nondominant eye, this is another version of what some call blended vision. Modern blended vision options are not your grandmother’s monovision, where one eye was corrected strictly for distance and the other eye distinctly for near. Rather, blended vision with corneal inlays restores near vision in the treated eye with minimal or no detriment in distance acuity in that eye. In my experience, people who never adapted to old-school monovision were fine with what it produced for near but never really liked what they gave up in distance acuity in the near eye to achieve it. That fact highlights one of the major advantages of this new class of presbyopia solutions. Below are a few highlights of Raindrop implantation.
• Patients often achieve J1 or J1+ near acuity on day 1.
• The procedure is reversible.
• The inlay is invisible to the patient and outside world; cyborgs need not apply.
• It is a corneal procedure that preserves the crystalline lens.
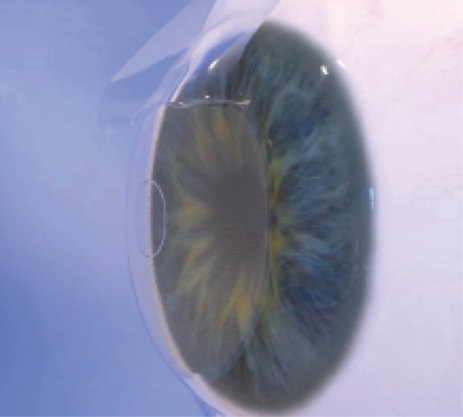
The Raindrop is implanted under a femtosecond laser flap.
At the 2015 ASCRS meeting in San Diego, I reported on 39 patients who were implanted with the Raindrop at my center in San Antonio as part of the multicenter prospective US IDE study.1 The patients we enrolled were presbyopic emmetropes (MRSE, -0.50 to +1.00 D) requiring at least +1.50 D to +2.50 reading add. The Raindrop inlay was implanted in the nondominant eye and centered over the light-constricted pupil. A femtosecond laser was used to create a flap one-third of the central corneal thickness deep.
At 12 months, we found that:
• 100% of patients achieved 20/25 binocular acuity at near, and 80% were
20/20 at near;
• 100% of patients maintained 20/20 binocularly at distance;
• 97% of patients achieved 20/32 binocular acuity at intermediate; and
• 100% of patients achieved at least 20/25 binocular acuity for both distance and near.
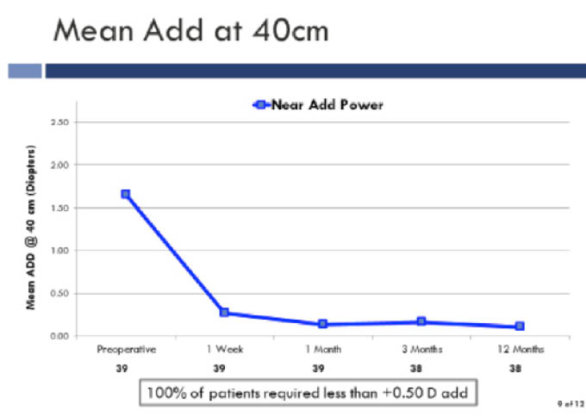
After implantation of the Raindrop 100% of patients required less than +0.5 D reading add.
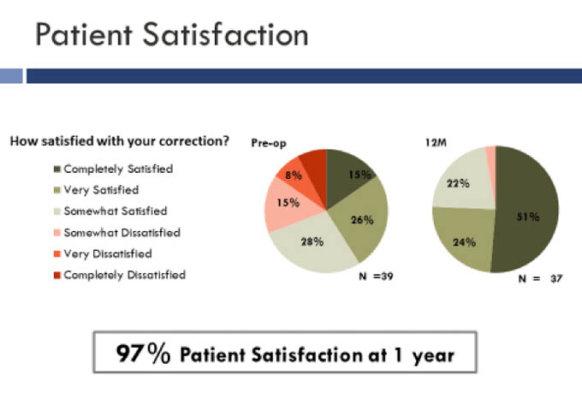
Patient satisfaction with the Raindrop inlay.
Overall, 97% of patients reported being satisfied with these results. The Raindrop inlay improved near vision by nearly 6 lines of acuity and intermediate vision by 3.5 lines.
CONCLUSION
The full range of vision and high patient satisfaction support the Raindrop inlay as a valid tool to treat presbyopia. As baby boomers continue to seek a level of vision that is compatible with their active lifestyles, corneal inlays will be an important addition to our surgical toolset. Let’s put the selfie sticks away already.


