
Combining intrastromal corneal ring segments (ICRS; Intacs [Addition Technology]) with CXL maximizes the benefits of surgical intervention for patients with keratoconus. The goal of CXL is to strengthen the cornea and stop the progression of keratoconus. ICRS improve patients’ visual acuity. By reshaping the cornea and by supporting and improving the symmetry of the cone, ICRS correct myopic defocus, and they render the astigmatism more regular, which makes it easier to correct with glasses or contact lenses. The result is improved visual acuity.
Symmetric ICRS are used when the cone on the posterior float is located within the 3- to 5-mm optical zone and the spherical power is greater than the cylindrical power on the manifest refraction. Asymmetric ICRS or a single inferiorly placed segment is used when the cone is decentered and located outside the 3-mm optical zone and the cylindrical power is greater than the spherical power on the manifest refraction. Determining which thicknesses of ICRS to implant depends on the nomogram based on the patient’s preoperative manifest refraction spherical equivalent, the cone’s location, and the degree of asymmetric astigmatism.
At Storm Eye Medical University of South Carolina, my colleagues and I are studying the results of the combined procedure. We are evaluating its effect on keratometry, corneal topography, and corneal tomography with the Pentacam (Oculus Optikgeräte), and we are assessing epithelial remodeling using spectral-domain OCT. We see patients at 1 week, 1 month, 3 months, 6 months, and 12 months postoperatively. The results have been encouraging. Usually, we find stability at between 6 and 12 months. Thus far (approximately 20 eyes), we are finding that the epithelial thickness profile becomes more regular in treated eyes. I have been surprised to observe changes in keratometry readings of up to 5.00 D in some cases, a far greater effect than I had anticipated.
CASE EXAMPLE
A 27-year-old man presented with worsening vision in his right eye. Upon examination, the manifest refraction was -3.50 -6.00 @ 70º, and his CDVA measured 20/60. Corneal tomography showed inferior steepening, superior flattening, an increase in the inferior-superior ratio, and irregular astigmatism. The Kmax reading was 54.40 D, which, 6 months later, had increased to 58.70 D (Figure 1). The patient was unable to tolerate contact lenses.
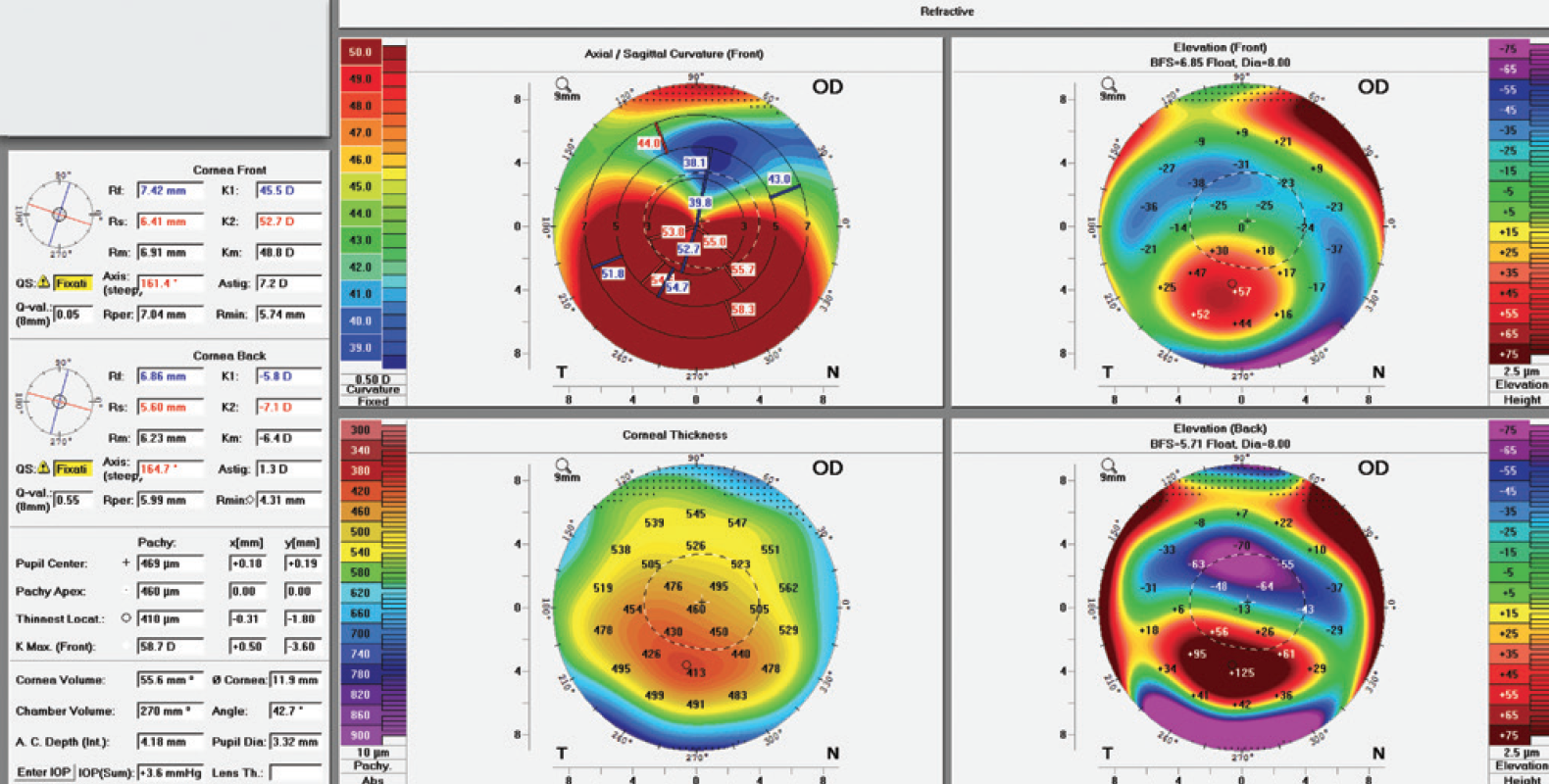
Figure 1. Corneal tomography. Kmax measured 54.40 D at presentation. It had increased to 58.70 D 6 months later (shown here).
Using the FS200 Femtosecond Laser (Alcon), I created the tunnel using a femtosecond laser and placed a 0.45-mm segment inferiorly. I positioned the thicker segment to correspond to the keratoconic cone (inferiorly) so as to lift it and produce the maximal flattening effect. After securing the incision, I performed epithelium-off (epi-off) CXL with the KXL System (Avedro). At the conclusion of the case, I instilled one drop of moxifloxacin hydrochloride ophthalmic solution 0.5% (Vigamox; Alcon) and placed a bandage contact lens.
Immediately after surgery, I advise patients to start administering moxifloxacin and prednisolone acetate 1% four times daily and to use preservative-free artificial tears frequently. Typically, I see them 1 day after surgery, and then, within 5 to 7 days postoperatively, I remove the bandage contact lens.
Three months postoperatively, the Kmax was 54.50 D (Figure 2). The manifest refraction was -2.50 -4.00 @ 65º, and the CDVA measured 20/30+1 OD. Corneal tomography demonstrated more regular astigmatism that could now be corrected with glasses and contact lenses.
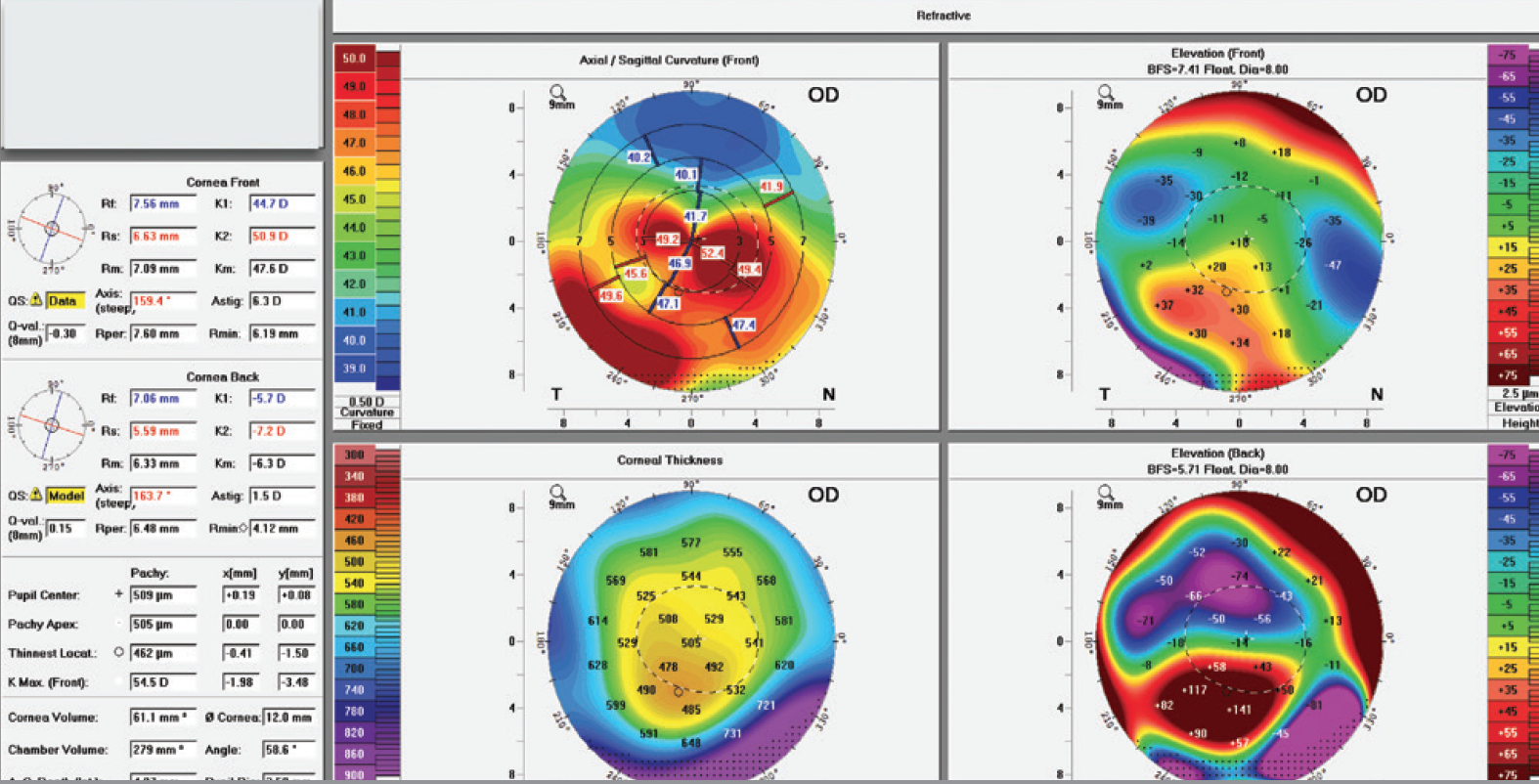
Figure 2. Three months after combined ICRS and CXL, the Kmax was 54.50 D, and the astigmatism was more regular.
Significant regional variability in epithelial thickness is observed in keratoconic eyes (Figure 3A). Epithelial remodeling occurs in abnormally curved corneas in such a way as to minimize topographic irregularities. Thus, the corneal epithelium tends to thin over the corneal apex in eyes with keratoconus and to thicken over adjacent areas. Three months postoperatively, analysis of epithelial remodeling with spectral-domain OCT revealed a more regular thickness profile in all meridians (Figure 3B).
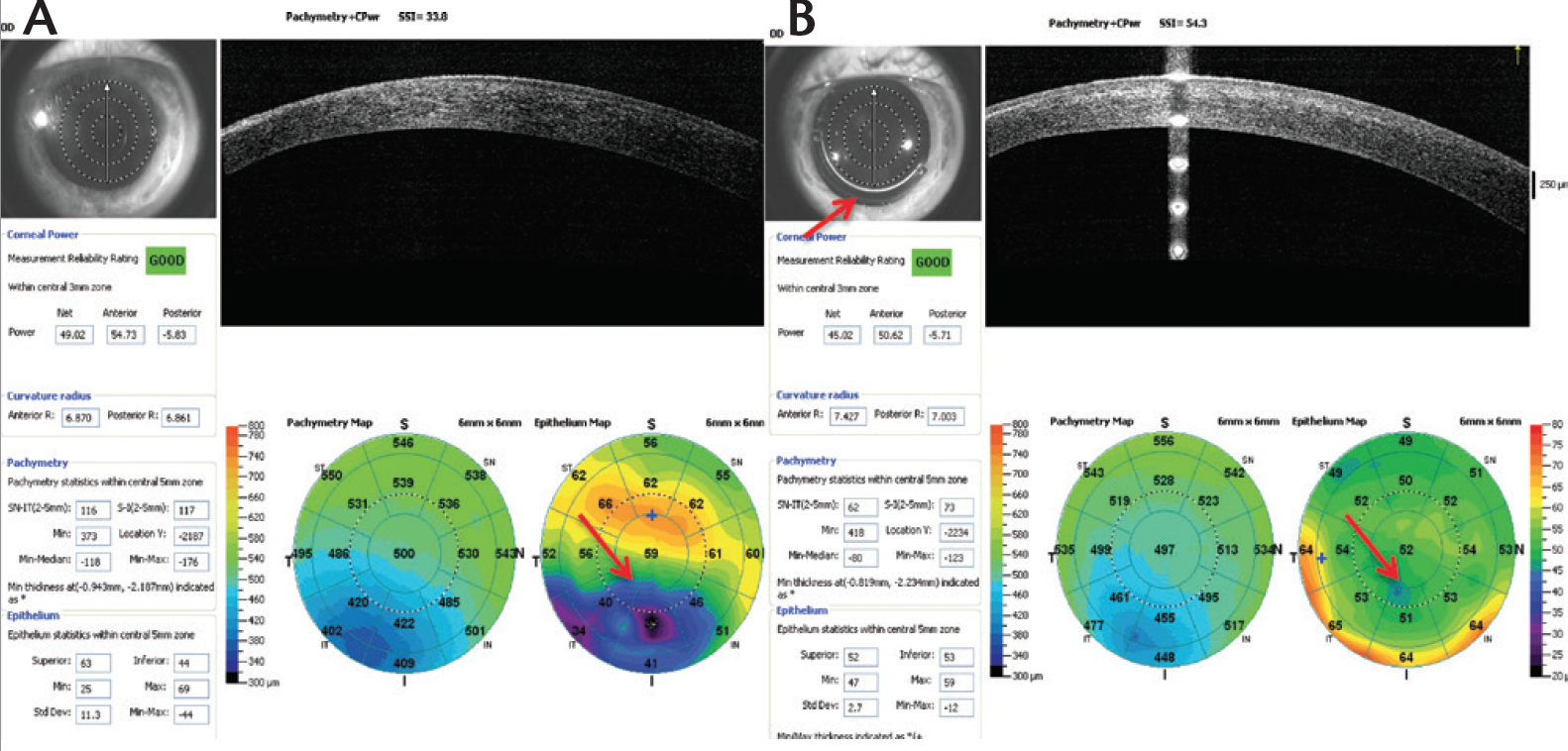
Figure 3. Corneal epithelial remodeling preoperatively (A) versus postoperatively (B).
TAKE-HOME POINTS
- For patients with mild keratoconus, low astigmatism, and a visual acuity better than 20/30, CXL alone is probably the best option. More severe forms of the disease will induce high amounts of asymmetric irregular astigmatism. In patients with moderate keratoconus, combining ICRS and CXL can improve their visual acuity, while strengthening the cornea and halting disease progression. This approach will not help patients with severe keratoconus or hydrops, however; in these cases, a corneal transplant is indicated.
- ICRS are contraindicated in eyes with corneas thinner than 450 µm at the incision site, and epi-off CXL is contraindicated in eyes with corneas thinner than 400 µm. There is no Kmax cutoff per the ICRS guidelines, but as stated earlier, eyes with clinically severe keratoconus may not benefit from the combined procedure and instead require a corneal transplant.
- It is important to maintain corneal hydration during surgery.
- The incision depth for ICRS should be at least 66%. Sutures are maintained for 2 months. Overly tight sutures induce astigmatism.
- Contact lens fitting may start as early as 6 weeks postoperatively with the understanding that the patient’s vision may fluctuate for up to 6 months before stabilizing. Visual acuity will continue to improve over time after the combined procedure.
- Complications with the combined procedure have been rare. Should epithelial healing be delayed, use of a bandage contact lens can be extended to a few weeks. Amniotic grafts, autologous serum, or other therapies to assist epithelial healing may be considered.
- Combining ICRS and CXL is off-label. At present, only epi-off CXL is approved in the United States. A direction for future research is the combination of epithelium-on CXL with the placement of ICRS. This option could broaden the pool of candidates and reduce the pain and risk of complications associated with epithelial removal such as infection and scarring.


