A 37-year-old man was referred to our clinic for progressive corneal neovascularization and scarring in his left eye with symptomatic monocular diplopia. The patient history includes total left facial nerve palsy resulting in paralytic lagophthalmos and complaints of worsening vision, eye redness, and double vision due to exposure keratoconjunctivitis.
The left facial nerve palsy was secondary to a complicated acoustic neuroma excision performed 3 years prior. No pain was noted due to lack of sensation on the left side of the patient’s face. The patient had tried conservative therapy including tarsorrhaphy, gold weight implantation, aggressive corneal lubrication with preservative-free artificial tears and ointment, and a moisture chamber at bedtime without significant improvement.
The patient’s BCVA was 20/150. Slit-lamp examination of the left eye revealed conjunctival injection, central corneal scar, temporal neovascularization, and 2+ punctate keratitis. A Zenlens scleral lens (Bausch + Lomb) was fitted to tangentially align the sclera and provide 250 µm of clearance over the cornea and limbus. The area of clearance was filled with preservative-free saline solution (Figures 1 and 2), and the patient was instructed to wear the lens for 4 hours with gradual build-up to waking hours while continuing with the bacitracin ointment and moisture chamber at bedtime.

Figure 1 | Areas of hyperreflectivity over the scleral contact lens are indicative of contact lens desiccation. However, the underlying cornea remained hydrated by a chamber with preservative-free saline.
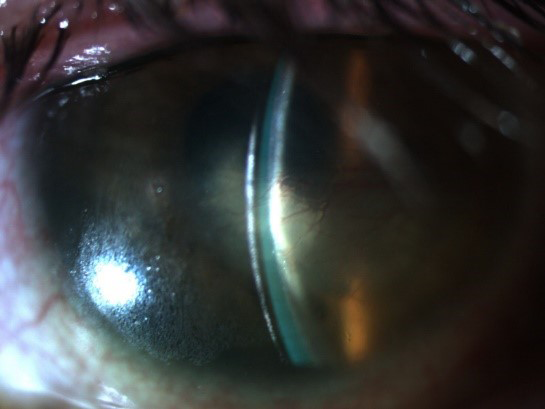
Figure 2 | After approximately two doses of tocilizumab, central foveal thickness was 283 µm.
At the patient’s 8-week follow-up visit, he reported an improvement in ocular hyperemia and vision. The patient increased his lens wear time to waking hours while continuing to use the moisture chamber and antibiotic ointment at night. Slit-lamp examination revealed stable 3-o’clock stromal vessels and 3-o’clock stromal scar, and his punctate keratitis had resolved. Visual acuity improved to 20/60 with complete resolution of monocular diplopia. The patient was to continue with the current lens modality and was instructed to follow up in 4 months for further corneal evaluation.
DISCUSSION
Ocular surface disease is a multifactorial disease, and the addition of cranial nerve palsies requires the practitioner to become innovative with nontraditional approaches. In recent years, with the advent of more gas-permeable contact lens materials, scleral shells have become a mainstay in managing this subset of patients who present with severe ocular surface disease.1
In the past, traditional therapy of aggressive lubrication, tarsorrhaphy, gold weight implantation, punctal plugs, amniotic membrane, and bandage contact lenses tended to fail.2 Traditional PMMA scleral shells were unreliable due to their poor oxygen transmissibility resulting in corneal edema.3 Additionally, with exposure keratitis, evaporation makes many lenses unwearable due to loss of hydration.
With the addition of silicone acrylate into contact lenses, the effects of contact lens–induced hypoxia can be better controlled. Theoretical spreadsheet models have been utilized to recommend fitting patients in materials with the highest oxygen transmissibility value (Dk) while minimizing lens thickness.4
The gas-permeable material of the contact lens used in this case is from a class of fluorosilicone acrylate lenses known as Hexafocon B. The Dk for Hexafocon B, non-edge corrected, is high at 161.5 Upon achieving optimal alignment on the sclera, the oxygen permeability of the lens allows the carefully measured saline reservoir to remain oxygenated throughout the day. Additionally, fitting the lens to allow for tangential scleral landing zones provides the cornea with adequate tear exchange for daily wear, improving oxygenation.
The incidence of microbial keratitis with scleral contact lenses is low, but it greatly increases with overnight lens wear. Scleral contact lens wear is limited to waking hours in this patient while nightly moisture chamber and antibiotic ointment is maintained. Additionally, the scleral contact lens can still provide the refractive benefits of a traditional hard contact lens to correct irregular astigmatism in addition to its moisturizing chamber properties.6 Both the improved corneal health and regular optical surface yielded this patient’s 20/60 BCVA.
Although not perfect, scleral contact lenses may provide an effective one-step solution to an otherwise challenging two-step problem.
1. Rosenthal P, Croteau A. Fluid-ventilated, gas-permeable scleral contact lens is an effective option for managing severe ocular surface disease and many corneal disorders that would otherwise require penetrating keratoplasty. Eye Cont Lens. 2005;31(3):130-134.
2. Williams ZR, Aquavella JV. Management of exposure keratopathy associated with severe craniofacial trauma. J Cataract Refract Surg. 2007;33(9):1647-1650.
3. Walker MK, Bergmanson JP, Miller WL, Marsack JD, Johnson LA. Complications and fitting challenges associated with scleral contact lenses: a review. Cont Lens Anterior Eye. 2016;39(2):88-96.
4. Michaud L, van der Worp E, Brazeau D, Warde R, Giasson CJ. Predicting estimates of oxygen transmissibility for scleral lenses. Cont Lens Anterior Eye. 2002;35(6):266-271.
5. Bausch & Lomb Boston XO2 gas permeable lens material gains FDA clearance for daily wear. Science Letter. October 2, 2007. bit.ly/2LXFBbY. Accessed April 12, 2018.
6. Severinsky B, Behrman S, Frucht-Pery J, Solomon A. Scleral contact lenses for visual rehabilitation after penetrating keratoplasty: long term outcomes. Cont Lens Anterior Eye. 2014;37(3):196-202.




