Watch the latest episodes of the Innovation Journal Club series on Eyetube.

While considered the gold standard for targeting robust IOP reduction, risks and complications associated with trabeculectomy warrant careful consideration and may disqualify some patients from the procedure. Newer surgical techniques and approaches may be a viable alternative in select cases, at least as an interim step before incisional techniques are needed. In episode 4 of Innovation Journal Club, host I. Paul Singh, MD, sat down with Sahar Bedrood, MD, PhD, to discuss two studies that compare minimally invasive bleb-forming procedures with trabeculectomy.
GPS: Gel Stent Versus Trabeculectomy
When it was introduced, the Xen gel stent (Allergan, an AbbVie company) ushered in a new category of glaucoma surgeries: minimally invasive, device-based, bleb-forming procedures. Whether they qualify as MIGS is not fully established, nor is the nomenclature to describe them. Nevertheless, due to a similar mechanism as trabeculectomy—facilitate nonphysiologic drainage to the subconjunctival space via a bleb formed postoperatively—they are intended to offer similar IOP-lowering efficacy, albeit with a more favorable safety profile.
According to Dr. Bedrood, the Gold Standard Pathway (GPS) Study was designed to help answer questions pertaining to patient selection and the clinical utility of the gel stent in eyes requiring modest IOP reduction. The safety and efficacy of the two procedures was compared in a head-to-head fashion in a 12-month, open-label, prospective, randomized, multicenter study. in 159 eyes (139 treated; 95 Xen, 44 trabeculectomy) with “poorly controlled glaucoma” (defined as IOP of 15–44 mm Hg on ≥1 topical medication).
The topline takeaway from the study was that gel stent was noninferior to trabeculectomy. Although trabeculectomy achieved slightly greater IOP lowering (Figure 1), the safety outcomes favored the gel stent (Table 1).
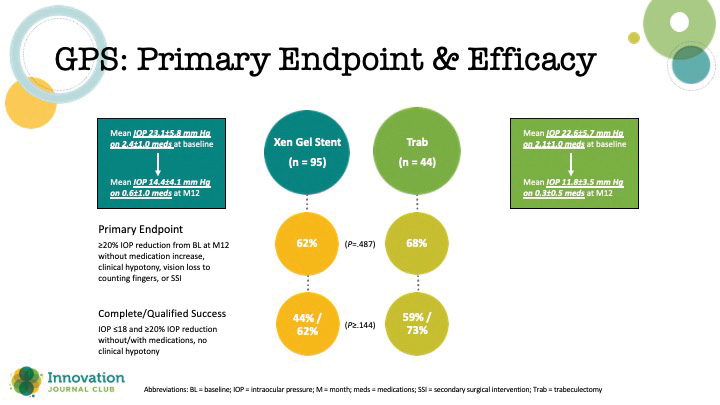
Figure 1. Primary endpoint outcomes in the GPS study.
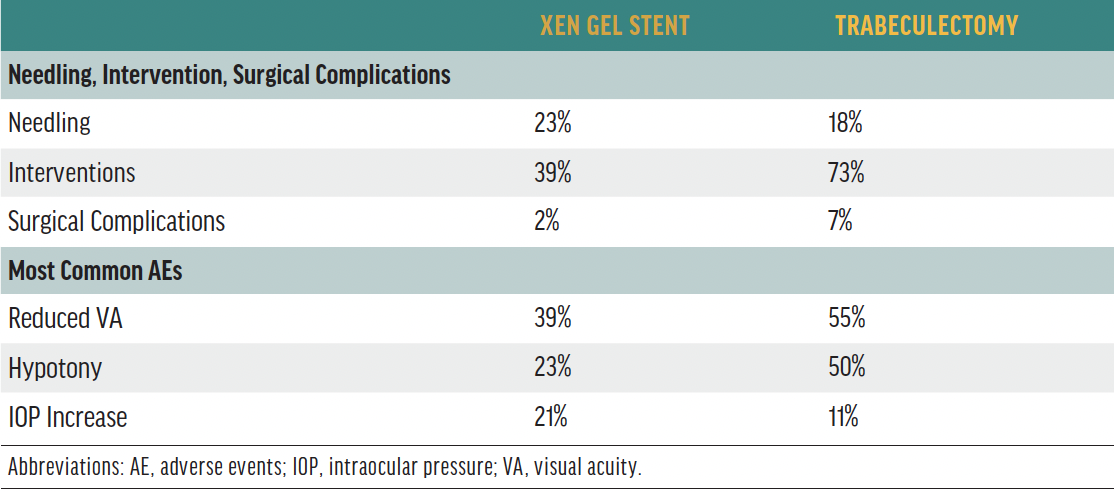
Table 1. Safety outcomes in the GPS study.
“I love a good Trab,” Dr. Bedrood explained. “I always say that when I talk about Xen because there is a point where [a trabeculectomy] is important to do when you want those super low pressures, when you have a patient who is progressing at 13, 14 [mm Hg], and you want to try to get them down to 8 or 9 [mm Hg]. It may be worth the risk of this to get them down. But if you have a patient that doesn’t need that super low pressure, then let’s do the thing that has a higher safety profile at the end.”
According to Dr. Singh, the safety profile of the gel stent has made him more comfortable performing surgery earlier than he would have with a tube or trabeculectomy. Unlike trabeculectomy, which involves several surgical variables that effect the outcome (ie, flap thickness, size, and placement; sure placement, etc.), drainage is facilitated by a patent microstent, thus making IOP response more reliable.
“The post-op period [with the gel stent], for me, has been much more controlled and predictable,” Dr. Singh said.
Interim Analysis of Pivotal Study
Although the pivotal study for the PreserFlo Microshunt (Santen/Glaukos)—another miniature implantable stent that affects drainage to the subconjunctival space via a conjunctival bleb—did not meet its primary endopoint, it nevertheless demonstrated clinically meaningful efficacy in secondary endpoints and was associated with more favorable safety (Figure 2).1
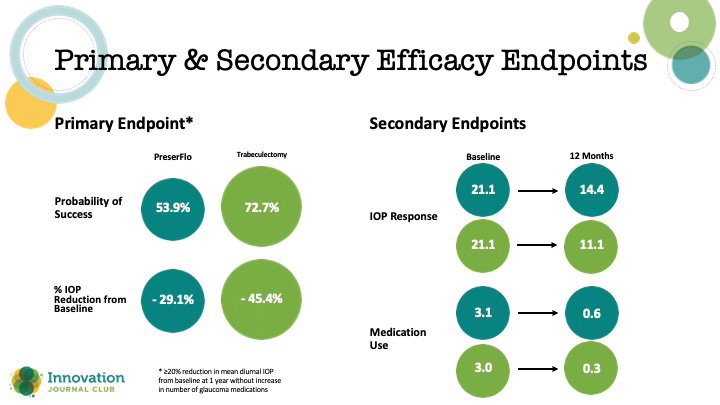
Figure 2. Primary and secondary endpoints in a study that compared PreserFlo to trabeculectomy.
According to Dr. Bedrood, the pivotal trial results should be viewed as only one piece of information about a promising device currently being reviewed by the FDA.
“I don’t see the fact that it didn’t meet that primary endpoint as being a game-over situation by any means. The standard was really high, and I think that there is definitely room to hopefully revisit this and reinvent it in a way that it’s applicable to our patients,” Dr. Bedrood said.
Dr. Singh added that interpreting outcomes from the study requires some context.
“It’s hard when you compare a new procedure to one that you’ve done for hundreds and hundreds of cases,” Dr. Singh said. “In this study, and the previous study we talked about earlier with GPS, trabeculectomies did better than historical data. So we’re getting better at trabeculectomy, it’s not that the, let’s say, PreserFlo didn’t work at all. In fact, it had significant reduction.”
What the blossoming category of minimally invasive, bleb-forming glaucoma surgeries ultimately offers, Dr. Bedrood said, is an answer to a current unmet need in clinical practice—the types of patients the ophthalmologist knows instinctually need a more aggressive approach to control IOP, but for whom the safety risks conjure a moment of pause. As well, she said, once a new device clears regulatory and enters the market, surgeons are likely to identify ideal patients, gain experience with the techniques, and thereby achieve better outcomes than witnessed in clinical trials.
1. Baker ND, Barnebey HS, Moster MR, et al; INN005 Study Group. Ab-externo microshunt versus trabeculectomy in primary open-angle glaucoma: one-year results from a 2-year randomized, multicenter study. Ophthalmology. 2021;128(12):1710-1721.


