This content is for U.S. healthcare professionals only.
The last decade has brought both a surge of patients that need glaucoma treatment and a renaissance of glaucoma treatment options that have taken glaucoma surgery from the exclusive domain of the glaucoma subspecialist and enlarged it to include almost every ophthalmology office. As these physicians are looking for ways to surgically treat their refractory glaucoma patients, they are looking for options that will effectively lower intraocular pressure (IOP) with reliability, predictability, fast recovery, and minimal tissue manipulation. Four comprehensive ophthalmologists shared why they decided to perform the XEN Gel Stent (Allergan/AbbVie) procedure, how they went about learning the new technique, and how they integrated it into their practices.
Onboarding XEN in a Comprehensive Ophthalmology Practice
Deborah Ristvedt, DO
As a third-generation comprehensive ophthalmologist, I returned to my hometown to carry on the family practice. Located several hours away from a major city, travel distance to subspecialists presents a hardship for many of our patients. Thus, addressing glaucoma patients and incorporating interventional glaucoma procedures in my practice is an important part of being able to fulfill the needs of our patient demographic. Following the pioneering example of my father and grandfather, I have tasked myself to continuously learn about the latest developments in glaucoma and develop the skill set necessary to perform surgical procedures that allow me to serve our patients locally.
XEN Benefits
The XEN Gel Stent was a natural extension of my existing armamentarium and has proven beneficial for my patients. Many of my glaucoma patients need something beyond topical medications. When traditional aqueous drainage pathways are no longer adequate, XEN bridges the gap between maximum tolerated medical therapies and more invasive procedures, many times producing outcomes similar to trabeculectomy.1 XEN can be used alone or in conjunction with cataract surgery. It has a lot of flexibility.
Why I Adopted the XEN® Gel Stent
Amin Ashrafzadeh, MD; David Goldman, MD; Ahad Mahootchi, MD; and Deborah Ristvedt, DO, share key reasons why they use the XEN® Gel Stent (Allergan/AbbVie), including its established safety profile, reliable IOP reduction, medication reduction, and recovery time.
Implanted via an injector as an outpatient procedure (Figure 1), the XEN stent provides me with an opportunity to intervene at an earlier disease stage. Limited tissue manipulation allows for recuperation or recovery and leaves open the possibility for surgical procedures down the road as the disease progresses.
Figure 1. The Xen Gel Stent (left) is implanted via an injector (right) as an outpatient procedure.
I find that XEN is an effective tool for patients who previously had limited options. Although a patient may have already undergone laser therapy, MIGS, or cataract surgery, some need more help to achieve IOP reduction. Often, these patients have reached maximum tolerated medical therapy but have not progressed to the point of requiring invasive “rescue” therapies. Knowing that we can try the XEN approach before proceeding to more invasive procedures offers relief to my patients.
Since incorporating XEN into my practice, new and existing patients enjoy the ease of the procedure. Looking at the overall picture of glaucoma being a long-term disease process, it is wonderful to offer another treatment option.
Take Advantage of Learning Resources
Adherence to training is critical to long-term success. As a lifelong learner and surgeon, I actively seek knowledge and continuously work at refining my surgical technique. Prior to implanting the XEN Gel Stent, or any new-to-you procedure, take time to practice the steps to develop mental and muscle memory. Participate in wet labs and skill transfer labs to get the technique down prior to going live.
As ophthalmologists, we have the unique opportunity to get together with one another and share pearls that have made us better. As I was getting started with the XEN Gel Stent, I remember being at a meeting, sharing my observations on technique with implantation, dosage of MMC, and needling with a mentor of mine. This sharing of ideas was energizing. I am so grateful to the leaders in the field, who I look up to, that have experience, and who take the time to encourage and instruct. My partners are also key mentors who motivate me to be excellent. We share cases and videos with one another. I am grateful to be in a group that cares so much for one another and our patients. Bleb management is one of the main reasons we may not adopt this procedure. There are wonderful resources that I have used from the company itself for needling technique and postoperative management.
When starting, choose your initial patients anatomically. Select patients with plenty of exposure and a healthy conjunctiva. Start conservatively for your first 10-15 cases, then, as you learn the nuances of the surgical technique (how to effectively rotate the eye, where to make your incisions, etc.) and develop skill in placing XEN, consider transitioning to patients with more challenging anatomy, such as tight lids, deep-set eyes, prominent brows, or prior trabeculectomy. Multiple potential surgical approaches provide flexibility to address a broad range of patients. As I have optimized my technique over time, my outcomes have improved and my target patient parameters expanded, resulting in increased productivity.
Gain an understanding of what the bevel should look like and learn how to rotate it into the subconjunctival space. When learning this ab interno technique, it can feel like you are going through the conjunctiva; it takes experience to get a feel for where to stop. Ask your colleagues about their experience with placement, angle, and how to enter the scleral wall. You can gain skills and knowledge from each other by being creative and working out techniques.
As surgeons, we are accustomed to optimizing patient outcomes through technique refinement. In the clinical trial, about 32% of cases require needling.1 Study eyes undergoing glaucoma-related secondary surgical intervention and/or removal of the XEN Gel Stent prior to the 12-month evaluation were considered to be nonresponders. Seven subjects in the study underwent needling procedures with mitomycin C; 4 of these subjects were considered responders. Bleb management can feel intimidating, but it is simply an opportunity to revise and optimize outflow, so do not let that stop you from learning the XEN technique. The need for needling also tends to decrease as surgeons hone their craft. Ask for advice from peers, and study publications to learn bleb morphology and needling technique.
Setting Patient Expectations
Set realistic expectations for patients. It is important to distinguish the difference between visual improvement versus vision preservation to avoid disappointment with the outcomes. I cite published data when making safety claims and discussing potential complications. Since many of my XEN candidates have had cataract surgery, it is easy to explain that they can expect a similar postoperative recovery period; however, they will need to use drops to prevent tissue scarring. This is also when I bring up the topic of needling by telling them that some eyes scar quickly and will need a little revision, but that we can perform it here in the office.
Educating patients on the long-term gain afforded by earlier surgical intervention also helps them to buy into the idea of an implant. They go into the procedure with the understanding that XEN will not improve visual acuity, but it can help lower IOP. Elevated IOP presents a major risk factor for glaucomatous field loss. The higher the level of IOP, the greater the likelihood of optic nerve damage and visual field loss.
Measure of Success
Stabilized and lower pressures are quantifiable measures of success, but success encompasses much more than an IOP number. It is the ability to personally take care of my patients and provide them with the therapies they need, like XEN, in a familiar, friendly setting. It is about potentially reducing their medication burden. Success is providing pressure relief now while preserving the conjunctiva and health of the eye for later. The long-term benefits, though not readily measured, are very real. When treating glaucoma, my treatment goal is vision preservation, which means extended independence and gaining time before undergoing more invasive procedures and the accompanying discomfort and complications. Finally, hearing and seeing my patients express relief because they have minimal discomfort and a lower IOP that is stable in the low to mid-teens makes the investment of my time to learn this technology all worth it.
1. XEN Directions for Use.
Implantation of the XEN Gel Stent in Comprehensive Ophthalmic Practice
David Goldman, MD
As a cornea-trained comprehensive ophthalmologist, my natural inclination was to steer clear of glaucoma surgery. However, as glaucoma procedures evolved and could be combined with cataract surgery, I realized that I was actually doing my patients a disservice by not taking the time to learn new techniques and offer them in my practice. I began offering MIGS procedures at the time of cataract surgery, and when the XEN Gel Stent became available to implant, I began offering it in conjunction with cataract surgery or as a standalone option to lower my patients’ IOP.
Not a Traditional Tube Shunt
Early on, I found my main concern was bleb management and needling. As my skills improved and my technique progressed, I found my rate of needling continued to decrease. Considering the invasive nature of traditional trabeculectomies and implantable tube shunts, the surgical learning curve with implantation and needling is less pronounced. Needling can be performed easily in the office or the operating room with sedation. Some surgeons will also pre-emptively needle the bleb at the end of the case if the implant is immobile or excessively curled. I have found most of the time patients do not need needling. If a surgeon is confident in device placement but continues to feel uncomfortable needling a bleb, the patient can always be placed back on topical medications or referred to a glaucoma specialist. Most will feel comfortable managing the patient and will be more than happy to take over at that point.
Overall, I have felt the procedure to be safe and low stress to implant. In a recent clinical trial, zero intraoperative complications were encountered.1 Clinical trials did not show chronic hypotony, despite some short-term postoperative hypotony with a formed anterior chamber. In these circumstances, patients are monitored closely and typically self-resolve.
Success with XEN
In the primary analysis at 12 months, 76.3% of subjects (n = 65) achieved ≥ 20% IOP reduction on the same or fewer number of medications versus baseline.1 In my practice, I consider XEN a success if I have stabilized a patient’s IOP and avoided a more invasive surgical option. I consider XEN a success if I have lowered IOP and reduced the number of topical medications required. Reminding patients that glaucoma is a chronic disease and requires constant management with various treatment strategies throughout a lifetime is helpful to discuss prior to surgery. XEN has met patient/clinical goals in my practice by lowering IOP or reducing drop burden leading to more stable glaucoma.
Defining Success with the XEN® Gel Stent
Refractory glaucoma is a chronic disease, so everyone measures success differently. Amin Ashrafzadeh, MD; David Goldman, MD; Ahad Mahootchi, MD; and Deborah Ristvedt, DO, share what success with the XEN® Gel Stent (Allergan/AbbVie) looks like for their patients and how it has evolved over time.
Expanding My Skills With XEN
There are many reasons a comprehensive ophthalmologist may choose to offer XEN, and for me it came down to patient care. With limited access to glaucoma specialists and issues with insurance carriers, I wanted to keep taking care of my patients when medications stopped working. Most of my patients didn’t require a trabeculectomy or strict IOP control into the single digits. I came to realize that glaucoma specialists are incredibly busy, and I could expand my skills to fill the gap in care. I found XEN to be another option to try prior to referring out for more invasive surgeries.
Versatility with Targeting & Approach
Initially, I had some reluctance to adopt glaucoma surgery when I remembered my days in residency managing trabeculectomies and tube shunt failures. Gradually I began performing some of the angle-based MIGS procedures on the market and found them enjoyable. The XEN was the first minimally invasive conjunctival device that formed a bleb, placing it in a separate category from the angle-based devices. As the first ab interno approach to create a new pathway for aqueous flow, the stent is about the size of an eyelash and becomes soft and flexible once implanted in the eye, similar in constitution to the surrounding tissue (Figure 2). The gel stent can be implanted at the time of cataract surgery or as a standalone procedure. Use of the stent is versatile in this manner as it doesn’t limit other surgeries that may be needed down the road. Once I watched how the surgery was performed and how straightforward it was to implant, I quickly warmed up to XEN.
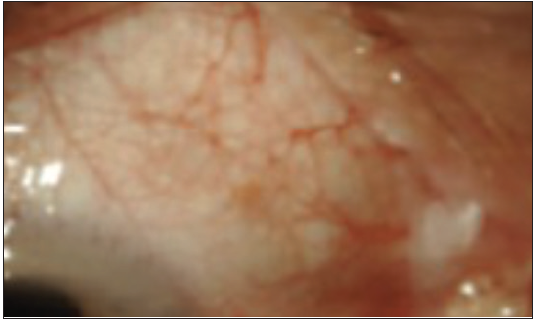
Figure 2. One-week postoperative.
Image courtesy of Vanessa Vera, MD.
Evolution of Technique and Optimizing Outcomes
My surgical technique continues to evolve for implantation. Surgeons who already perform intraocular surgery or conjunctival surgery have many of the skills necessary to begin implanting and managing XEN. The learning experience can occur during dedicated wet lab sessions with device representatives, online training, and other peer-to-peer programs, mentorships, and preceptorships. I think it takes about 10-12 cases in order to feel comfortable and proficient. With 10-20 more cases under your belt, you further hone your skills and optimize your outcomes.
Conclusion
The XEN Gel Stent is designed to deliver lower IOP in patients without sacrificing safety profiles. It bridges the gap between topical medications and invasive surgical approaches. The device accommodates both the needs of the patient and the surgeon while preserving conjunctival tissue for any future procedures, if needed. Comprehensive ophthalmologists can utilize it as they continue to grow their skill set to meet their patients’ needs.
1. Data on file, Allergan, 2016; Clinical Study Report R-020.
Long-term Patient Relationships Require Meeting Multiple Clinical Needs
Ahad Mahootchi, MD
Like a lot of ophthalmologists, I am a cataract surgeon with a refractive mindset. Over the last two decades, I have performed many procedures and made a lot of people happy with LASIK surgery and presbyopia-correcting lenses. I have continued to serve my patients by offering blepharoplasty, ptosis repair, and other procedures that keep my patients loyal to our office. But ultimately, a percentage of those patients are going to develop glaucoma, and I decided I wanted to be able to continue to treat those patients and do it in a cornea-friendly way.
The XEN Gel Stent works well in a broad range of patients. I can offer this to pseudophakic patients, patients that previously underwent MIGS, or patients that are uncontrolled on topical drops.1 We use it in patients who are not getting sufficient IOP lowering with drops or need additional lowering following MIGS. As I have gained experience, I find that I am able to achieve pressures in the low-to-mid-teens from a wide variety of baseline pressures, and it accomplishes this with a favorable risk-benefit profile. Adding XEN to my list of tools allows me to continue to treat my previous LASIK and cataract patients who also have glaucoma, providing a quick recovery while lowering their IOP.1
Sticking with It
When I decided to implement the XEN Gel Stent into my practice, I had a lot of built-up demand for an effective procedure with a benign postoperative course, and I hoped to really over-deliver and get my patients off all of their topical drops. My initial XEN implantations did exactly that 60% of the time. But 40% of the time I was performing more revisions than I wanted, and that propelled me to keep refining my technique.
In the clinical investigation, a topical steroid was started 5-7 days prior to surgery at the discretion of the surgeon, and continued through a 12-week taper, also at the discretion of the surgeon. However, I do it slightly differently. One change I made was to focus on a postoperative steroid that is strong enough to keep the body from closing off the tube, but not so strong that it induces a steroid response. In addition, I found a lot of my patients were running out of the topical steroid I prescribe postoperatively prior to completing the days indicated. Thus, I now inject a small amount of Kenalog-10 right at the tip of the bleb before they leave the operating table, and then I prescribe the patient loteprednol for 6 weeks following the procedure.
Acing the XEN® Gel Stent Learning Curve
With training, careful patient selection, and a multitude of peer resources, the learning curve with the XEN® Gel Stent (Allergan/AbbVie) is very manageable, according to Amin Ashrafzadeh, MD; David Goldman, MD; Ahad Mahootchi, MD; and Deborah Ristvedt, DO. Allergan offers wet labs and skills transfer labs to help physicians practice the technique, as well as representatives to answer questions during the first few surgeries.
In my opinion, performing digital ocular massage the first few days following XEN implantation aids in creating a large, diffuse bleb that is less likely to form adhesions around the stent. To enforce this, we have created an instructional video showing both the right and wrong way to perform digital ocular massage and posted it online for patients to review prior to coming in. The massage pressure is directed to the globe on the opposite side of XEN. When they do come into the clinic, we have them demonstrate the massage technique so that we can redirect them if needed.
I continued to look for published papers on the XEN technique. With these and the robust offering of online videos through Allergan’s training portal and instructions from colleagues, I have made multiple adjustments to my technique. My personal definition of success is low pressure with minimal revisions. The rate of postoperative needling in the clinical trial was 32%. When I started, my rates were even higher. Over time, I have made improvements to my surgical technique and now my personal needling rates are lower than 32%. The ideal outcome is a significant reduction in topical medications, and I can achieve that for most of my patients.
Serving My Patients
While I had to work hard to reduce the number of postoperative revisions with XEN, the safety profile has been satisfactory from the beginning. Consistent with the clinical trials, I have not had intraoperative complications or had any patients with hypotony maculopathy following stent placement. There are patients whose visual goals I have spent years trying to optimize, and I would not want to perform a procedure with a high risk of serious complications or refractive change.
I have not found another procedure to lower IOP that meets so many of the needs of my patients and my practice. Like many of my cataract colleagues, I have implemented a dropless cataract surgery regimen to enhance the experience of my patients. When I meet colleagues who are also using a dropless technique, I tell them that the next thing they need to do to enhance patient care is offer XEN.
1. Xen Directions for Use.
Improving Outcomes with Treatment
Amin Ashrafzadeh, MD
Many years ago, I would have patients come into my office crippled and in wheelchairs due to rheumatoid arthritis (RA). The prevailing treatment paradigm at the time was to manage pain with medications, but otherwise inform the patient they would eventually lose mobility. Then, better interventions were discovered and rheumatologists were able to be more proactive with treatment. Now, I virtually never see RA patients in wheelchairs in my office.
Glaucoma’s not so different. Once someone loses vision due to glaucoma, it is not coming back. Our job is to take the interventions currently available and attempt to slow or prevent further vision loss by lowering IOP. With safe, effective treatments like the XEN Gel Stent,1 I don’t hesitate to provide another option to my patients.
A Great Treatment Option for My Patients
About 5 years ago I started running into difficulty referring patients to the glaucoma specialists that I trusted, and the other options were a significant drive away. It became absolutely impractical for a large enough population within my practice to get to a specialist. I felt I needed to start offering glaucoma care myself.
When XEN was cleared by the US Food and Drug Administration in 2016,2 I felt the good safety profile and high efficacy would benefit many of my patients.1,2 I have refractory glaucoma patients that were well-controlled on topical medications but then were no longer able to continue administering their own drops. I have patients that have significant reactions to the preservatives in topical medications that need another option. There is a large group of patients that are currently uncontrolled on multiple drops that we probably should look at and see if there is another option that will better serve those patients. XEN offers a great option to my refractory glaucoma patients still uncontrolled on topical medications by delivering powerful efficacy without sacrificing safety, and by providing controlled IOP and medication reduction for the majority of these patients.
The XEN® Gel Stent Gets Patients the Treatment They Need
Amin Ashrafzadeh, MD; David Goldman, MD; Ahad Mahootchi, MD; and Deborah Ristvedt, DO, discuss how offering the XEN® Gel Stent (Allergan/AbbVie) allows physicians to maintain control of their patients' long-term care.
Learning the Procedure
Implantation of the XEN Gel Stent requires surgeon comfort in the anterior chamber, and I think that covers most cataract surgeons. My initial training regimen included videos and then working with the support of an Allergan representative for the first 10 cases. My very first case took quite a bit of time as I carefully ensured the stent was in the correct place, the distal end was free and mobile, and the outflow was satisfactory. By the fourth or fifth case, I was getting more proficient. By the tenth case, I was feeling more confident and comfortable. Lining up 10 XEN cases in a short interval may seem ambitious, but the repetition greatly eases the learning curve. As I continued to place more XEN stents, I further honed both my intraoperative and postoperative skills with the stent.
Understanding the ideal location for the stent within the eye is essential to optimizing the procedure (Figure 3). The goal is to place the stent between the conjunctiva and Tenon’s capsule, with approximately 1 mm of the stent visible in the anterior chamber and 2-3 mm of the stent visible in the subconjunctival space, with the tip free and mobile.3 At this point, I find that 80% of my patients that receive XEN have a significant benefit from the procedure without any postoperative needling. That is a huge number in the world of glaucoma procedures.
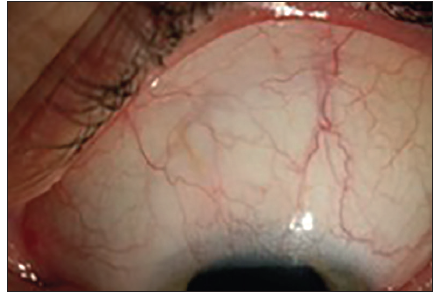
Figure 3. IOP is 13 mmHg on three medications OS.
Image courtesy of Ingeborg Stalmans, MD.
Comprehensive ophthalmologists worry about procedures with postoperative management. When dealing with postoperative complications, it’s important to say that persistent hypotony did not occur in the clinical trials.1 Other postoperative complications are generally easier to manage.1
I’ve gotten a positive response from many of my patients who have undergone the XEN procedure.
1. XEN Directions for Use.
2. US Department of Health and Human Services. https://www.accessdata.fda.gov/cdrh_docs/pdf16/K161457.pdf. Published November 16, 2016. Accessed September 12, 2020.
3. Vera V, Gagne S, Myers JS, et al. Surgical approaches for implanting XEN gel stent without conjunctival dissection. Clin Ophthalmol. 2020;14:2361-2371.
INDICATIONS
The XEN® Glaucoma Treatment System (XEN® 45 Gel Stent preloaded into a XEN® Injector) is indicated for the management of refractory glaucomas, including cases where previous surgical treatment has failed, cases of primary open-angle glaucoma, and pseudoexfoliative or pigmentary glaucoma with open angles that are unresponsive to maximum tolerated medical therapy.
IMPORTANT SAFETY INFORMATION
CONTRAINDICATIONS
XEN® Gel Stent is contraindicated in angle-closure glaucoma where angle has not been surgically opened, previous glaucoma shunt/valve or conjunctival scarring/pathologies in the target quadrant, active inflammation, active iris neovascularization, anterior chamber intraocular lens, intraocular silicone oil, and vitreous in the anterior chamber.
WARNINGS
XEN® Gel Stent complications may include choroidal effusion, hyphema, hypotony, implant migration, implant exposure, wound leak, need for secondary surgical intervention, and intraocular surgery complications. Safety and effectiveness in neovascular, congenital, and infantile glaucoma has not been established. Avoid digital pressure following implantation of the XEN® Gel Stent to avoid the potential for implant damage.
PRECAUTIONS
Examine the XEN® Gel Stent and XEN® Injector in the operating room prior to use. Monitor intraocular pressure (IOP) postoperatively and if not adequately maintained, manage appropriately. Stop the procedure immediately if increased resistance is observed during implantation and use a new XEN® system. Safety and effectiveness of more than a single implanted XEN® Gel Stent has not been studied.
ADVERSE EVENTS
The most common postoperative adverse events included best-corrected visual acuity loss of ≥ 2 lines (≤ 30 days 15.4%; > 30 days 10.8%; 12 months 6.2%), hypotony IOP < 6 mm Hg at any time (24.6%; no clinically significant consequences were associated, no cases of persistent hypotony, and no surgical intervention was required), IOP increase ≥ 10 mm Hg from baseline (21.5%), and needling procedure (32.3%).
Caution: Federal law restricts this device to sale by or on the order of a licensed physician. Please click here for the full Directions for Use. Please call 1-800-433-8871 to report an adverse event.
©2021 AbbVie. All rights reserved. XEN® is a registered trademark of AqueSys, Inc., an AbbVie company. XenGelStent.com. XEN149082 09/21
XEN® Gel Stent Important Safety Information for Healthcare Professionals
Collapse -
INDICATIONS
The XEN® Glaucoma Treatment System (XEN® 45 Gel Stent preloaded into a XEN® Injector) is indicated for the management of refractory glaucomas, including cases where previous surgical treatment has failed, cases of primary open-angle glaucoma, and pseudoexfoliative or pigmentary glaucoma with open angles that are unresponsive to maximum tolerated medical therapy.
IMPORTANT SAFETY INFORMATION
CONTRAINDICATIONS
XEN® Gel Stent is contraindicated in angle-closure glaucoma where angle has not been surgically opened, previous glaucoma shunt/valve or conjunctival scarring/pathologies in the target quadrant, active inflammation, active iris neovascularization, anterior chamber intraocular lens, intraocular silicone oil, and vitreous in the anterior chamber.
WARNINGS
XEN® Gel Stent complications may include choroidal effusion, hyphema, hypotony, implant migration, implant exposure, wound leak, need for secondary surgical intervention, and intraocular surgery complications. Safety and effectiveness in neovascular, congenital, and infantile glaucoma has not been established. Avoid digital pressure following implantation of the XEN® Gel Stent to avoid the potential for implant damage.
PRECAUTIONS
Examine the XEN® Gel Stent and XEN® Injector in the operating room prior to use. Monitor intraocular pressure (IOP) postoperatively and if not adequately maintained, manage appropriately. Stop the procedure immediately if increased resistance is observed during implantation and use a new XEN® system. Safety and effectiveness of more than a single implanted XEN® Gel Stent has not been studied.
ADVERSE EVENTS
The most common postoperative adverse events included best-corrected visual acuity loss of ≥ 2 lines (≤ 30 days 15.4%; > 30 days 10.8%; 12 months 6.2%), hypotony IOP < 6 mm Hg at any time (24.6%; no clinically significant consequences were associated, no cases of persistent hypotony, and no surgical intervention was required), IOP increase ≥ 10 mm Hg from baseline (21.5%), and needling procedure (32.3%).
Caution: Federal law restricts this device to sale by or on the order of a licensed physician. Please click here for the full Directions for Use. Please call 1-800-433-8871 to report an adverse event.







