Sponsored By

During the past several years, there has been a changing paradigm of refractive cataract surgery. Our patients are savvier, they have higher expectations, and they expect a refractive outcome. They are attracted to and seek out advanced technology, especially as they see friends, neighbors, and loved ones achieving greater independence from glasses and better visual outcomes than ever before. This roundtable was convened to address some of the ways in which we can achieve better outcomes and become better refractive cataract surgeons.
—Cathleen McCabe, MD, moderator

Cathleen McCabe, MD, moderator
LenSx user for 4 years
Cathleen McCabe, MD, is a cataract and refractive specialist practicing at The Eye Associates of Bradenton and Sarasota, Florida. She is a consultant to and speaker for Alcon. Dr. McCabe may be reached at (941) 792-2020; cmccabe13@hotmail.com.

Kendall Donaldson, MD, MS
LenSx user for 4 years
Kendall E. Donaldson, MD, MS, is an associate professor of ophthalmology, cornea/refractive surgery/external disease; medical director; and cornea fellowship codirector at Bascom Palmer Eye Institute in Plantation, Florida. She is a consultant to Alcon. Dr. Donaldson may be reached at (954) 465-2765; kdonaldson@med.miami.edu.

Preeya K. Gupta, MD
LenSx user for 6 months
Preeya K. Gupta, MD, is assistant professor of ophthalmology at Duke Eye Center in Durham, North Carolina. She is a consultant to Alcon. Dr. Gupta may be reached at (919) 660-5071; preeya.gupta@duke.edu.

Elizabeth Yeu, MD
LenSx user for 3.5 years
Elizabeth Yeu, MD, is in private practice at Virginia Eye Consultants and an assistant professor of ophthalmology at Eastern Virginia Medical School in Norfolk, Virginia. She is a consultant to Alcon. Dr. Yeu may be reached at (757) 622-2200; eyeu@vec2020.com.
FLACS and YOUR PRACTICE
Cathleen McCabe, MD: With numerous developments in ophthalmic surgery in the recent past, what feedback have you received from patients with regard to having more advanced technology in your practice, such as the femtosecond laser-assisted cataract surgery (FLACS)?
Kendall Donaldson, MD, MS: In my experience, the idea of having a laser is very appealing to patients, and part of this may stem from laser refractive surgery on the cornea. Lasers imply precision in the mind of patients, so they tell me that they feel very confident about their outcomes because their surgery is being done with a laser. I tell patients that this is a less traumatic way to perform surgery, as we can put less energy into the eye1,2 and be more precise with our astigmatism correction. Patients understand that, and it is very appealing to them.
FLACS OVERVIEW
Dr. McCabe: There are some data to back up that statement. Quite a few publications3,4 are now showing that femtosecond laser results in less damage than manual techniques and provides better endothelial cell protection for patients who are at risk for that. Let us discuss ways that femtosecond laser gives you extra confidence that what you are doing is supported by scientific evidence? What published data are there that describe these improved results?
Elizabeth Yeu, MD: It is wonderful that we have the ability to perform corneal incisions and utilize the lens softening platforms that femtosecond laser provides us. However, one of the biggest benefits is that it increases our predictability and our refractive reproducibility, as shown in the 2012 Filkorn study (Table 1).5 Laser refractive cataract surgery does seem to provide better predictability with your IOL power calculations. It is possible that the standardized, well-centered capsulorhexis created with FLACS provides more stability with IOL positioning and less tilt (Table 2).6
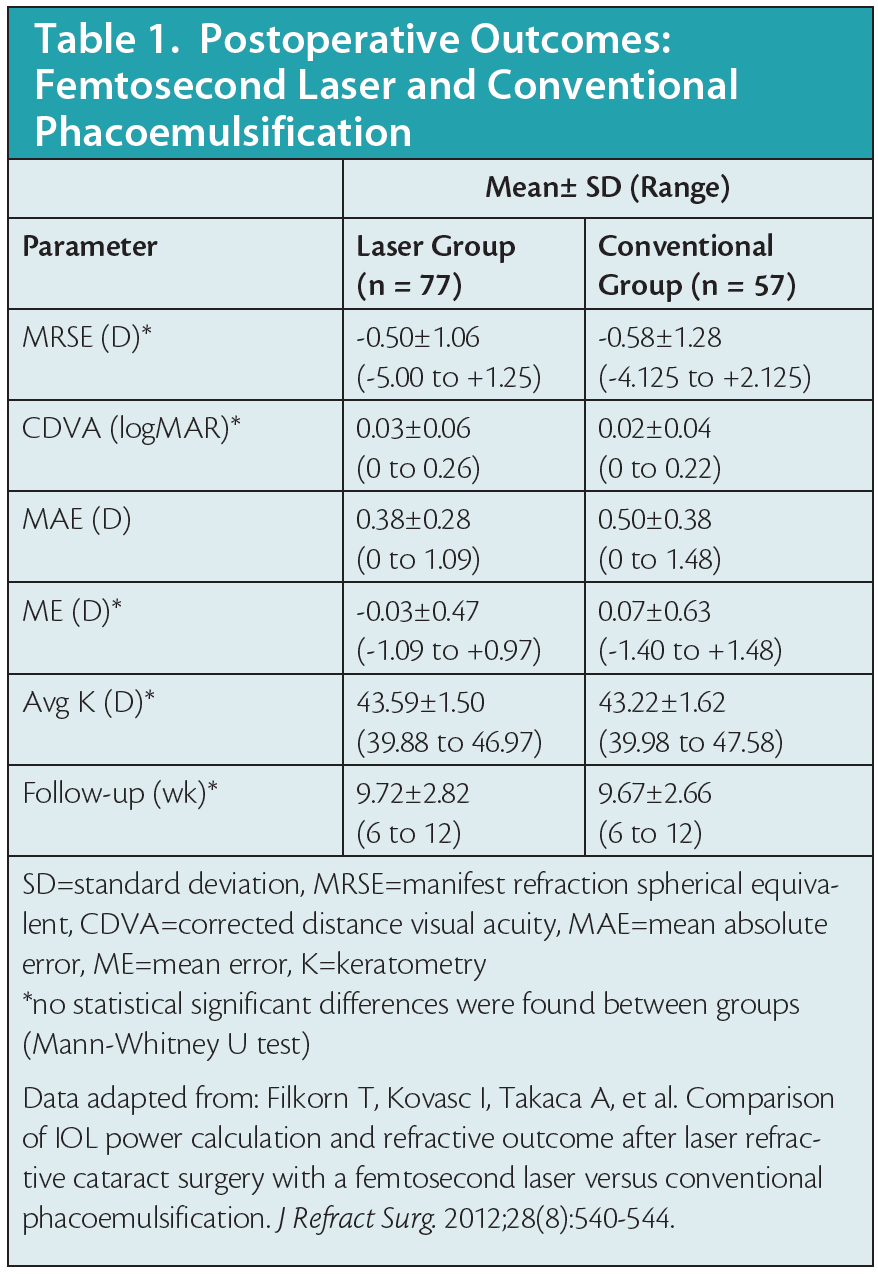
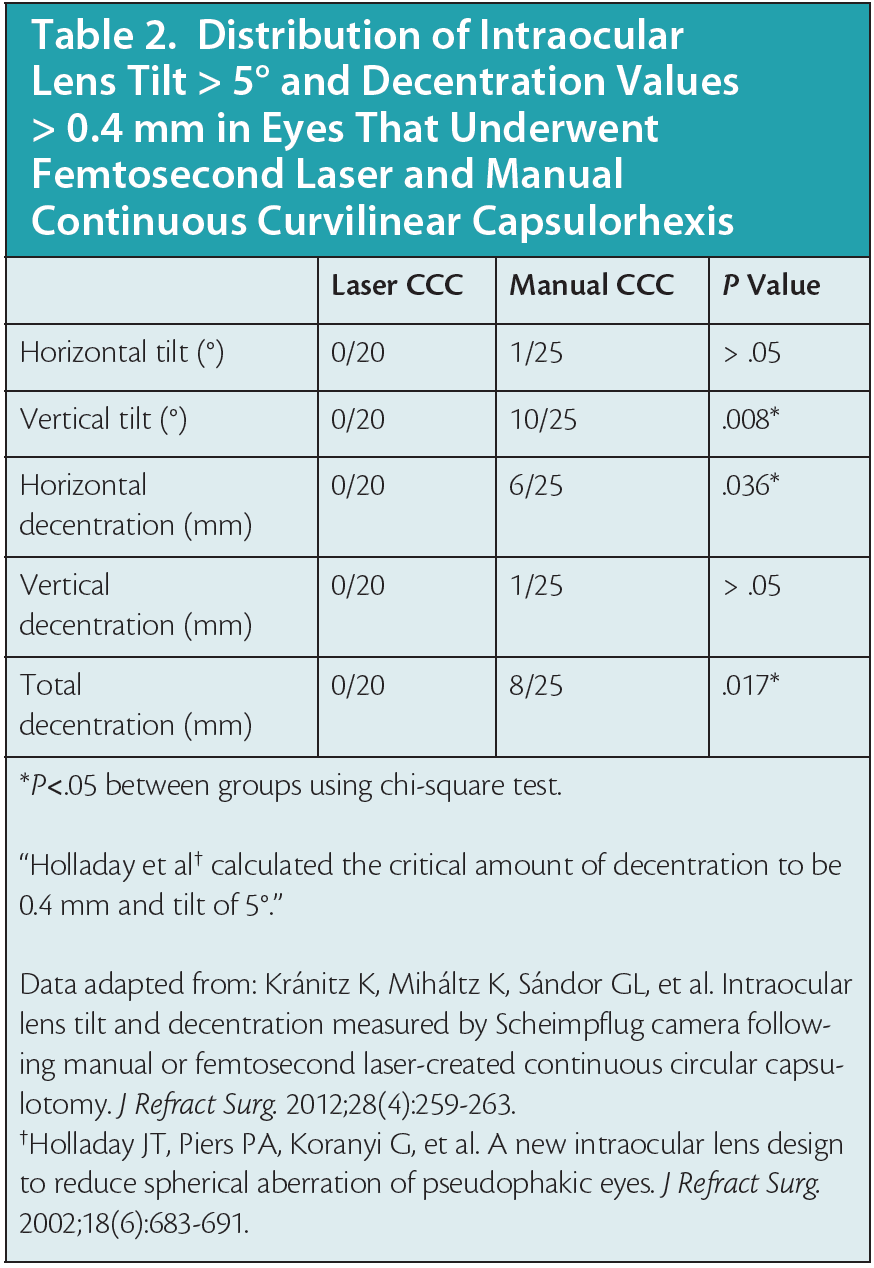
Dr. McCabe: That is important with the multifocal lenses, and we have seen success with our patients. You want to make sure that you are hitting that centration and that the lens is stable and not going to tilt (Figure 1).
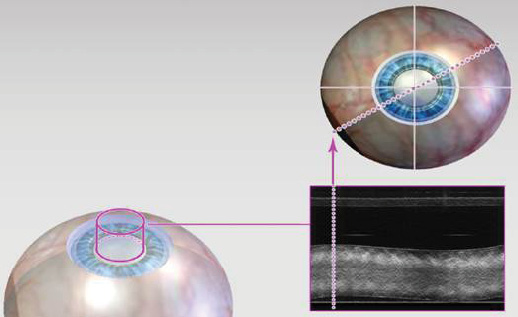
Figure 1. With the LenSx Laser, surgeons have a real-time OCT circle scan to ensure a complete capsulotomy.
Dr. Donaldson: As lens designs continue to advance through the years, it is going to be even more essential that we use a femtosecond laser to create just the perfect size capsulorhexis or capsulotomy (Figure 2), so we are better equipped to predict the lens position.6 It is becoming more important in my practice to have that degree of precision and centration.
Figure 2. Surgeons can program the LenSx Laser to create a precise circular capsulotomy.
Click here for Important Product Information
Experience with adopting the technology
Dr. McCabe: Let us talk about the first few months of using the LenSx Laser (Alcon). What things stand out most as you look back on that experience?
Preeya K. Gupta, MD: The ease of use stands out to me because I was not expecting it to be so easy to use. Before I started using the LenSx Laser, I was worried that it was going to be more complicated, or that it would push me too far outside of my comfort zone. But, I have been very pleasantly surprised that it is a very intuitive and easy technology to use. It takes you smoothly through all the planning steps. I learned it very quickly from the Alcon clinical application trainers.
I was also pleasantly surprised that Alcon took my comments to make improvements to the system. During my first 10 cases, I provided very honest feedback to a trainer from Alcon. Case by case, the trainer listened to what I said and helped me dial into my preferred nuclear disassembly technique, the type of incision that I wanted, and the feel of the incision that I wanted. I thought that was really impressive that the company customized the laser to mimic what I was used to doing and make it even better.
Dr. Donaldson: I have been extremely impressed with the patients’ experiences with the LenSx Laser. They tell me that they find it very comfortable. I explain that there is going to be a very mild pressure sensation, certainly not uncomfortable in any way, and I have never had anyone complain that it was uncomfortable to be under the LenSx Laser. In fact, many patients say it is a very positive, interesting experience for them.
I have also found it interesting how quickly things have advanced during the past few years. We acquired our lasers in 2012, but there have been amazing advancements and software upgrades, including the SoftFit Patient Interface (PI). Laser technology keeps getting better all the time. It seems we regularly get software updates that make the laser even better for our patients, surgeons, and staff.
FLACS, corneal incisions, and REFRACTIVE CATARACT SURGERY
Dr. McCabe: I was a little surprised by the incision-sealing ability. The incisions look pretty in the cornea. The quality of the corneal incisions is exceptional and the main incision seals very easily with little hydration (Figure 3). It was that quality of the corneal incision that we were looking for when considering future corneal applications. One of the things that we have added to how we use our LenSx Laser is the flap-making capability. In my practice, we are using the LenSx Laser to create flaps for LASIK as well.
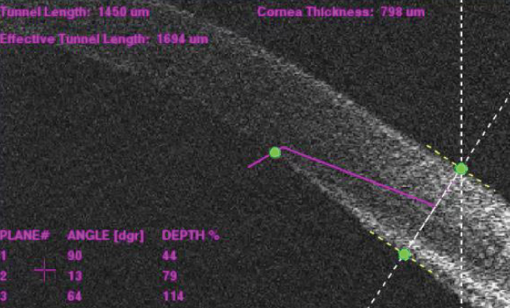
Figure 3. A three-plane corneal incision with the LenSx Laser.
Please describe some additional benefits of the LenSx Laser that you have seen in your practices, especially benefits that you were not expecting.
Dr. Yeu: Beyond the use of the LenSx Laser for creating corneal incisions, I specifically combine any cataract surgery involving premium IOLs or monovision goals with LACS. Specifically with the LenSx Laser, we have experienced a clinically significant improvement in our refractive predictability, and 92% of my LACS patients are within 0.50 D, as compared with the 83% refractive predictability seen in my 2015 manual cataract surgeries. This is my personal experience. Filkorn et al also demonstrated significant improvements in refractive predictability when using the LenSx Laser.5
Dr. Gupta: As a new user of the LenSx Laser, I have found that I have a higher percentage of patients who have an uncorrected distance vision of 20/20. Many patients that we see on a daily basis come in with under 1.00 D to 1.25 D of astigmatism, and I think that the femtosecond laser provides reliable and predictable corneal incisions to help manage low levels of astigmatism as part of cataract surgery. I have become more confident in describing the laser and in talking about astigmatism management with my patients. The number of patients in my practice who want laser for their surgery has increased over time. I feel this is because of my increased confidence that is related to improved visual outcomes.
Dr. McCabe: Let us discuss improving visual outcomes and what it means to be a refractive cataract surgeon today compared with 10 years or so ago.
Dr. Donaldson: I think it is an exciting time for us to be cataract surgeons. I think the field of cataract surgery and the evolution into refractive cataract surgery has been so exciting. Over the past 10 to 15 years, we have introduced a great deal of new technology for our patients, including laser cataract surgery and many new IOL options. Therefore, patients have really come to think of cataract surgery as one of the great opportunities of a lifetime. It is not just the opportunity to remove their cataract, but also an opportunity to correct their refractive error and to have more freedom from glasses. So, they have much higher expectations. These days, it seems every patient has a friend or family member who had cataract surgery and has raved about his or her experience and freedom from glasses. Many patients are expecting equal freedom from glasses and a high-level refractive outcome. Fortunately, we have the technology available now to help them achieve their goals.
Dr. Yeu: I completely agree with Dr. Donaldson. I think that corneal refractive surgery, as it has evolved, has really raised the bar. We have continued to try to emulate the similar high quality-of-vision outcomes with cataract surgery, and that is what the past 5 to 8 years have really provided us. We have been able to incorporate different technologies that can give us that better quality of vision and those outcomes.
TOOLS TO IMPROVE OUTCOMES
Dr. McCabe: Expectations are higher for everybody: for the patient, for the referring doctor, and for us as surgeons. What are some of the things that you have implemented in your practice? Specifically, what tools have you implemented that help improve outcomes?
Dr. Yeu: I think intraoperative technology tools, including the lens options and the actual femtosecond laser technology itself, have helped me become a more sophisticated refractive cataract surgeon. In my practice, which is a multispecialty group, we have a very strong referral network; 74% of the patients are referred from our optometry partners. This makes positive patient outcomes extremely important because our shared patients go back to their eye care providers for their primary eye care needs.
Dr. McCabe: Expectations are high—not just for the patient, but for the other doctors who share in the care of the patient.
Dr. Yeu: I absolutely agree. I think different technology pieces have helped us achieve a greater level of satisfaction, which also helps our referring doctors to have more trust that we can achieve those outcomes for their patients.
There are three parts to improving outcomes. We need to do what we can preoperatively on a naïve cornea to ensure that we understand the patient’s cornea surface. Next, we have the diagnostics. We strive to acquire the best measurements, in addition to fine-tuning ourselves as surgeons and optimizing our own outcomes. Third, I think we must prescribe the proper medications postoperatively to aid in healing. So, there are multiple components, and it really is a commitment.
Dr. Gupta: I am in an academic setting, and have a number of patients who are also comanaged with optometrists. Regardless of where my patients are coming from, they universally want to see better and, more often than not, want to see without glasses. Many patients come to me having either had LASIK surgery or have at least heard of refractive surgery and are familiar with the concept of laser technology.
For me, managing astigmatism has been a big part of providing refractive cataract surgery. The biggest advantage, in my experience, of the femtosecond laser and intraoperative aberrometry is a better ability to manage astigmatism. That has improved my success rate in terms of providing my patients with desired refractive outcomes. They are seeing great at distance, near, or both, depending on which intraocular lens I am using.
Dr. Donaldson: I agree with Dr. Gupta. I think that managing astigmatism is something we really have to embrace. If we do not manage astigmatism properly, through accurate preoperative assessment and implantation of the correct toric lens, then we cannot accurately apply a true refractive correction to the patient. Whether we are creating our corneal incisions with a blade or a laser, treatment begins with accurate preoperative measurements. In my hands, I really appreciate the laser as a tool to perform my most accurate astigmatism management.
In my experience, now that I can use the laser to help design and execute my surgical plan, I feel more confident that I am providing complete refractive correction. This is particularly important with our presbyopia-correcting lenses that demand minimal residual refractive error. Personally, I find myself correcting more patients’ astigmatism and doing it much more accurately than I did manually 5 to 10 years ago, thanks to the use of femtosecond laser technology.
Dr. Yeu mentioned the private practice thought process involved here, and it is similar in academic centers, where both Dr. Gupta and I practice. Patients are being referred to us by ophthalmologists and optometrists. They expect the highest degree of safety and accuracy with our refractive cataract surgery, and we have to achieve that.
I also agree with Dr. Yeu when it comes to analyzing our results. It is essential to analyze our data and continue refining our outcomes through our data collection. This is very important.
Dr. McCabe: I think these are all very important factors as we strive to be more precise in our outcomes. We want to know that we are correcting all of the refractive error, the patient’s sphere but also his or her cylinder. I am in private practice, and we do things similarly in my practice as well. One tool that has been helpful is the introduction of our femtosecond laser, which allows another level of precision to certain aspects of the treatment. I think you alluded to this, Dr. Donaldson, when you were saying that the laser is more precise in cutting corneal incisions to help us manage astigmatism during cataract surgery. We are happy to have that as an additional tool that may help in how we manage astigmatism.
Dr. Donaldson: Before the femtosecond laser, I was not performing many manual corneal incisions, and I did not feel as confident with my astigmatism management during cataract surgery. But now that we have the LenSx Laser, we have more confidence in what we are doing in creating and carrying out our surgical plan, especially with regards to managing astigmatism due to the reliability and precision of the LenSx Laser incisions with less tilt and decentration. I think if we look at the number of patients who are having astigmatism correction, it is very different now since femtosecond technology has come into play.
Dr. Yeu: I agree. If you looked at the 2015 Annual Survey for ASCRS,7 50% of the more than 2,000 respondents said they do not perform corneal incisions. I believe this hesitation to adopt manual corneal incisions is largely due to the lack of exposure to and inexperience with corneal-relaxing incisions during residency or fellowship. Unfortunately, you cannot jump into refractive cataract surgery without being able to understand how to perform corneal astigmatic keratotomies, because it is not uncommon to have some mild residual mixed astigmatism, postoperatively, even with the most experienced cataract surgeons. Multifocal IOLs are particularly affected by residual astigmatism. Every 0.25 diopter of residual astigmatism leads to a loss of a line on the Snellen eye chart. With that being said, being able to manage that astigmatism using femtosecond laser technology has provided more reproducible and accurate outcomes. When I need to manage residual astigmatism during cataract surgery, the precision of the femotosecond laser allows me to better standardize my corneal incisions at specific optical zones and tissue depth,3,8 which in turn allows me to more easily address lower levels of corneal astigmatism.
Click here for Important Product Information
SPECIAL CASES WHERE FEMTO LASER EXCELS
Dr. McCabe: That is terrific. Are there other cases or special circumstances where you find the femtosecond laser is essential to your practice? In my practice, I have found that the LenSx Laser is particularly effective on white or very dense cataracts.9 In fact, I will often use the laser for these patients even when they cannot, for financial reasons, elect to have advanced refractive results with femtosecond laser, because I believe there is an increased level of safety. Does anyone have similar experiences to share?
Dr. Gupta: I am a cornea specialist by training, and I see many patients at the academic center who have complicated corneas. A special population in which I have noticed particular benefit of the femtosecond laser are my patients with early Fuchs dystrophy—there is often less corneal edema because of the lower amount of energy used with the femtosecond laser.8 There are studies4,10 that show pachymetry tends to be lower early on in patients who have femtosecond LACS compared with manual surgery. I think that is especially true in the Fuchs patients who have a tenuous cornea, and you are trying to preserve endothelial cells. I think this is a great use of the femtosecond laser.
Dr. Donaldson: I agree with Dr. Gupta. I enjoy using the femtosecond laser with my patients with Fuchs dystrophy. Just like the dense cataracts that Dr. McCabe mentioned, the situation is similar with patients with loose zonules because you do not want to over manipulate the nuclear material. I find that presoftening the lens helps to have less nuclear manipulation, which helps facilitate cataract removal (Figure 4). In patients with small anterior chambers, having the lens presoftened allows me to put less energy into the eye, which is important since there is less working space.4 That is another situation where I particularly enjoy using the femtosecond laser.
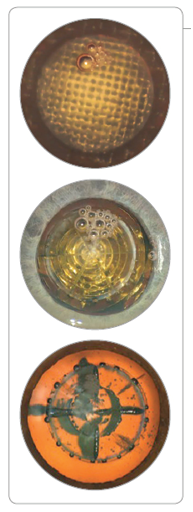
Figure 4. Pretreating the lens may help to have less nuclear manipulation, which helps facilitate cataract removal.
Dr. Yeu: In my opinion, femtosecond laser makes my cataract surgeries easier. Period. I actually feel more relaxed when I am operating on several cases in a row that are laser-assisted. It improves my day because I feel like the femtosecond laser adds a level of security and helps me get through my cases more readily and quickly. Beyond just refractive cataract surgery, the laser also provides a therapeutic benefit when used on more complex cataract surgery patients. Dense lenses, very soft lenses, and dislocated crystalline lens cases can be tackled with greater ease with FLACS.9
DISPELLING MYTHS and addressing barriers to adoption of flacs
Dr. McCabe: You have described several benefits in improving outcomes, in increasing surgery-day efficiency, in lowering the stress level for the surgeon, and in simplifying complicated cases. What do you think is holding back our other colleagues from adopting this technology? What are some of the negative comments you may have heard when talking with colleagues who have not yet adopted femtosecond laser for cataract surgery?
Dr. Gupta: My delay in using the laser was because I wondered, like many surgeons, about the value of femtosecond laser and if it was truly better than manual surgery. I think many surgeons are fearful of the technology, and they fall into the trap of not trying it for themselves prior to forming an opinion on the technology.
Whether you are an excellent surgeon or not, I believe that almost every group will find some benefit to the femtosecond laser technology. I would implore everyone to try it because it is easy to use and integrate into your own workflow, makes the surgery more streamlined, and it offers you the opportunity to manage residual astigmatism beyond the toric for a full cataract refractive outcome. Not to mention, additionally aid in treatment of the difficult case types that we have talked about. I felt the LenSx Laser was easy to use from my first surgery. I was also very well supported throughout the entire process by Alcon’s training staff and service group. I felt like it was an easy transition, and I am happy that I did not shy away from the process because of general fear of the technology.
Dr. Yeu: I believe there are two primary reasons why some ophthalmic surgeons have not embraced femtosecond laser surgery. The first is that phacoemulsification is just so good. When we jumped from extracapsular to phacoemulsification cataract surgery, it became a very refined procedure. Those who have performed cataract surgery with this technology for the past 10 years often wonder what can be improved or added to it. Second, people get comfortable. With laser cataract surgery, or any kind of technology of this magnitude, the learning curve can be daunting.
One thing I want to highlight is how much I like using the SoftFit PI (Figure 5) of the LenSx Laser. We have two different laser systems, one being the LenSx Laser, and the other is a laser with a two-piece, liquid interface docking system. I find that the capsule integrity with the LenSx Laser is superior. Studies support that the LenSx Laser provides less capsular tear.11
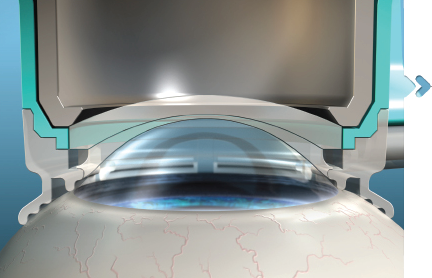
Figure 5. The LenSx Laser’s SoftFit Patient Interface.
It is very rare—maybe one in 150 cases—that I do not have a capsulotomy that is free floating. Then at the same time, because of the design of the patient interface, I also have excellent incisions. I believe these benefits, beyond everything else we discussed, can dispel any fears of the potential safety concerns of jumping into laser cataract surgery. My experience is also widely supported in the literature.9,12
Dr. Donaldson: I think that learning any new technology, or transitioning to something new in life, is difficult and can be stressful. Thank goodness Alcon is very supportive and sends supportive staff, especially when you are learning to use the LenSx Laser. The Alcon training staff help you through that initial period, and stay with you until you feel comfortable; they are with you every step of the way. There are also opportunities to bring in the laser once a month to try it, allowing surgeons to become more comfortable with the technology before purchasing the laser.
I think the concerns about expense and efficiency are two of the major things that prevent surgeons from purchasing the laser. They worry about the additional expense to their practice, and if they will have enough cases to support the investment. But, you really do not need that many cases, especially if you are in a surgery center where you have multiple providers.
I think if you are going to embrace this technology, you need to take the time to teach your staff about femtosecond technology, educate your patients, and provide them with that information early in the process. The surgeons and the staff have to believe in what they are doing and clearly understand the benefits. Once you get the staff on board, it can be a group effort. That excitement and confidence is passed on from the surgeon to the staff to the patients. In my experience, this approach has been very effective in many practices.
Dr. McCabe: One of the things that I have often heard is that surgeons are worried about how using a laser can impact the flow through the surgery center—that it may disrupt how efficient they are in their day. We did a small time study [unpublished data] in my facility and found that, on average, we spent about 2 minutes in the femtosecond laser room once we were familiar with the technology. It does not disrupt the day, and now I find that there are some efficiencies in the operating room that are related to the laser.
Dr. Yeu: I could not agree more with you, Dr. McCabe. Operating in two rooms requires the leadership of someone directing patients and having a point person or two within the operating room staff. Where I practice, we have two rooms and sometimes I will even do two lasers back to back. Once I perform laser surgery, I go back into the room where a prior patient has already been prepped and by the time I go into the second room, the patient who just had laser surgery is already prepped and ready to go. It may add an extra few minutes because I am in the laser room, but I am also oftentimes shedding 1 or 2 minutes off of my surgery. In the end, it seems to be a zero-sum game regarding time (Figure 6).
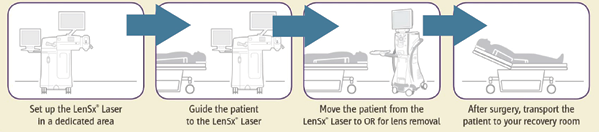
Figure 6. The LenSx Laser has no fixed bed, allowing the patient to stay on one bed throughout the entire cataract procedure.
Dr. Donaldson: A good way to begin your experience with the LenSx Laser is to observe surgeons who have experience with the laser. I learned a lot by observing the choreography of the day, just seeing how another surgeon had optimized the flow. I am coming from a university setting, which is generally not known for efficiency. We have our lasers inside the operating room, which is certainly not the most efficient way to set up a surgery center. But as Dr. Yeu was describing, having the laser in a separate room only adds 2 minutes. It can improve your efficiency and keep your day running smoothly.
Dr. Gupta: Where I practice, at Duke University, we now have three LenSx Lasers. As Dr. Donaldson mentioned earlier, one of the barriers to purchasing a femtosecond laser can be skepticism about return on investment if only one or two surgeons are using it. However, in our facilities, we had one or two physician champions for each of the lasers because they knew they would use the technology. As the other surgeons have become more familiar and comfortable with the laser, we needed to expand and increase the number of LenSx Lasers in our practice. We now have one at each of our major operating sites. I think that is an example of how you can use the laser and acclimate to the technology in a low-risk way.
Click here for Important Product Information
WHY the LENSX laser?
Dr. McCabe: We talked a lot about why adding femtosecond laser has been beneficial in your practice, but why did you choose the LenSx Laser? Are there some particular characteristics about the LenSx Laser specifically that influenced your choice?
Dr. Yeu: Without a doubt, for Virginia Eye Consultants where I practice, purchasing this laser has certainly been the best decision for our practice, because it really augments and adds to our refractive cataract surgery profile and offerings. Kudos to Alcon for all the advancements and upgrades to the system, including the SoftFit PI, which has been phenomenal.
At this point, we own different femtosecond laser platforms. While all systems have their unique qualities, a few attributes of the LenSx Laser really stands out. Firstly, the efficiency and the speed at which I can perform each patient treatment are exceptional, and I am generally able to be in and out of the LenSx Laser room for a treatment between 2 and 3 minutes. It takes me just 17 to 23 seconds to do the incision, capsulotomy, and fragmentation. The size of the PI also fits almost all eyes, which is also unique to the LenSx Laser. The SoftFit PI provides the “best of all worlds,” in my opinion, as the corneal and lens treatments are phenomenal. My peripheral corneal incisions open readily unless there is arcus or another opacity within the area of the incision. My capsulotomies rarely have any evidence of “misfires” with reduplicated tags or incomplete capsulotomies.10
Dr. Donaldson: I agree with Dr. Yeu. Also, Alcon’s service arrangements are wonderful. I was in the operating room this morning and we had a question about the LenSx Laser. We called our Alcon staff member on his cell phone. Not only did he answer our question, but within 15 minutes he stopped by and stayed with us for a couple of cases, until our concern was resolved. That is the level of service that they provide. It is really impressive. This one example is representative of my general experience with Alcon service being outstanding.
I also love the nonfixed bed with the LenSx Laser. Not having to transfer patients makes the process a bit quicker. Some laser platforms are associated with a fixed bed and require transfer of the patient from a gurney to the laser bed and back to the gurney for transport to and from the operating room suite. This can add additional time to the procedure, especially if the laser is in the operating room, as is true in our operating rooms at Bascom Palmer Eye Institute. I also like not having any portion of the laser over the patient’s body. Larger patients do not always fit under some laser platforms, but they can easily be treated with the LenSx Laser. That is a nice feature of the LenSx Laser.
Dr. McCabe: We really like the customizable platform of the LenSx Laser, especially the incision profiles. There are certain profiles I use for different things. You can utilize the benefits of that variability to more effectively treat your patients. Does anybody have any specific pearls about how they customize or use those features with their laser?
Dr. Yeu: I customize my platform by patient age based on birth year. For patients younger than 55 years who are having cataract surgery or a refractive lens exchange, I use a simple quad fragmentation. For those who are aged 55 to 70 years, I use a cubed fragmentation pattern using a larger cube size of 500 microns (Figure 7A). For patients older than 70 years, I automatically use fragmentation patterns with a 250 or 300 micron, the smaller cube size, because they are typically the most appropriate to match the density (Figure 7B).
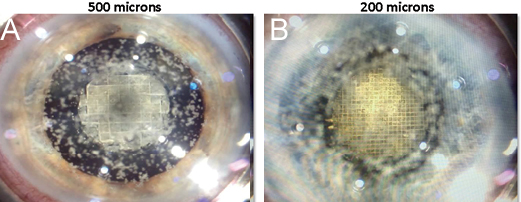
Figure 7. For patients who are 55 to 70 years, Dr. Yeu says the 500-microns cube size may be used (A). For patients older than 70 years, the 200-microns cube size may be used (B).
Dr. Gupta: I like to divide the nucleus into four quadrants and then the central cylinder. To me that was an easy way to start out using the LenSx Laser. As I have gotten more comfortable with using the laser, I am more confident and able to play around with the different settings. It is especially notable in patients who have a denser lens, the softening effect of the laser is a great addition. The software interface is very intuitive and navigates you through all the necessary screens. Docking is very easy with the SoftFit PI, and once docked it only takes a few seconds for scanning and image acquisition versus 25 to 45 seconds found on other systems (Figure 8).10,11
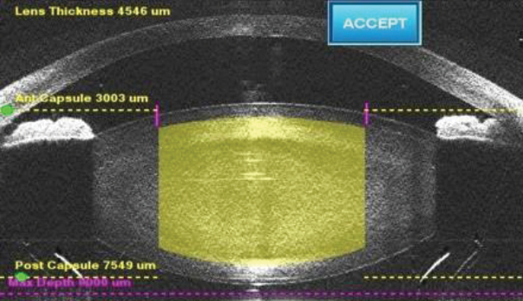
Figure 8. In her practice, Dr. Yeu says the LenSx Laser takes only a few seconds for scanning and image acquisition.
Dr. Donaldson: I like doing three cuts and three cylinders for several reasons. First, if you are a chopping surgeon, it is very easy to separate those segments. Then, I can have six smaller segments very easily that are already basically precut for me. With the cylinders and cuts, you can still easily visualize your capsulotomy, which I like. For most of my patients, I like the three cylinders, the three cuts. I find that very versatile.
Dr. McCabe: I use a fragmentation pattern with the chop extensions because I found that the gas bubbles tend to follow the chop extension and create quadrants in the peripheral portion of the lens.
I think the important point is that there are many different ways of using the software to customize treatment to the best effect for each surgeon and patient. We are all doing something a little bit different, which shows the laser’s versatility.
Dr. Donaldson: It is interesting that everyone finds what they like and uses the laser in different ways. Trying out all the different patterns and options allows you to fall into a pattern that you like best and feel most comfortable with. It is nice that we have all these options available to us.
WHAT I PERSONALLY VALUE MOST ABOUT FLACS
Dr. McCabe: We have all had an experience that has allowed us to value our LenSx Laser as a tool that assists us in delivering positive refractive cataract surgery outcomes that assist us in delivering better results to our patients.
If today I took away your LenSx Laser, what would miss the most? How would it impact your care of patients?
Dr. Gupta: For me, astigmatism management is what I would miss most with not having my LenSx Laser, especially for those patients with low levels of astigmatism. While manual corneal incisions can be effective, I feel in my hands, the laser incisions are much more reproducible.
Dr. Donaldson: I agree with Dr. Gupta. Without the LenSx Laser, I would not have the same level of confidence in making manual corneal incisions like I have with the laser-based corneal incisions. This is especially true for multifocal patients. We have to make sure we are right on target with our overall refractive correction.
In my opinion, the corneal incisions are a beautiful feature of the femtosecond laser that can maximize outcomes with our premium IOL technology. They go hand in hand.
Dr. Yeu: Based on my own experiences, I would have less confidence that I am going to hit the refractive target. Also, as a surgeon, my day would be a little more challenging because I believe the LenSx Laser makes my cataract surgeries easier and lead to a more enjoyable surgery day.
Dr. McCabe: I agree with all of you. I would also say that complicated cases with my LenSx Laser have become much more routine.10 Dense cataracts and white cataracts are no longer the heart-pounding experience they could be before I had my LenSx Laser.
Dr. Donaldson: In a teaching institution like Bascom Palmer Eye Institute, where I practice, we train a lot of residents and fellows in various techniques and technologies. But I have to say, teaching them to use the femtosecond laser is actually a relaxing experience. Whereas, teaching them other things without the laser can be a little anxiety-provoking at times.
I always reflect on the study by Jose De La Cruz13 in which the residents in training were learning to use the femtosecond laser before they learned how to do traditional phacoemulsification. He showed high levels of safety in the hands of brand-new surgeons. The LenSx Laser is a great tool, and teaching our residents and fellows to use it has been a pleasure.
Dr. Gupta: I agree completely with Dr. Donaldson. I think using the LenSx Laser is a great way to teach residents and fellows in a step-by-step manner how to perform manual surgery at an earlier stage in their careers. It also exposes the residents to the fundamental concepts in astigmatism management, corneal-incision creation (manual or laser), or refractive cataract surgery, in general, during their training. Teaching these concepts at an earlier stage will help to make refractive cataract surgery more mainstream.
Dr. McCabe: I think we are in agreement that this is excellent technology. It has allowed us to elevate our cataract surgery outcomes closer to the level of refractive corneal-based surgery. We benefit and our patients benefit, and I think that is a wonderful thing. I know we can all look forward to many improvements and new ways of using this technology to help our patients in the future.
© 2017 Novartis 8/17 US-LSX-17-E-0338a
1. Reddy KP, Kandulla J, Auffarth GU. Effectiveness and safety of femtosecond laser-assisted lens fragmentation and anterior capsulotomy versus the manual technique in cataract surgery. J Cataract Refract Surg. 2013;39:1297-1306.
2. Takacs AI, Kovacs I, Mihaltz K, et al. Central corneal volume and endothelial cell count following femtosecond laser-assisted refractive cataract surgery compared to conventional phacoemulsification. J Refract Surg. 2012;28:387-391.
3. Chen X, Chen K, He J, Yao K. Comparing the curative effects between femtosecond laser-assisted cataract surgery and conventional phacoemulsification surgery: A meta-analysis. PLoS ONE. 2016;11(3): e0152088.
4. Lawless M, Bala C. Femtosecond laser-assisted cataract surgery. US Ophthal Rev. 2014;7(2):82-88.
5. Filkorn T, Kovasc I, Takaca A, et al. Comparison of IOL power calculation and refractive outcome after laser refractive cataract surgery with a femtosecond laser versus conventional phacoemulsification. J Refract Surg. 2012;28(8):540-544.
6. Kranitz K, Mihaltz K, Sandor GL, et al. Intraocular lens tilt and decentration measured by Scheimpflug camera following manual or femtosecond laser-created continuous circular capsulotomy. J Refract Surg. 2012;28(4):259-263.
7. ASCRS 2015 Clinical Survey. Eyeworld.org. http://eyeworld.org/supplements/ASCRS-Clinical-Survey-2015.pdf. Accessed September 8, 2016.
8. Mastropasqua L, Toto L, Mastropasqua A, et al. Femtosecond laser versus manual clear corneal incision in cataract surgery. J Refract Surg. 2014;30(1):27-33.
9. Mayer WJ, Klaproth OK, Hengerer FH, Kohnen T. Impact of crystalline lens opacification on effective phacoemulsification time in femtosecond laser-assisted cataract surgery. Am J Ophthalmol. 2014;157(2):426-432.
10. Davidson J. The LenSx Laser-A review of current literature on its use in cataract surgery. US Ophthal Rev. 2016;9(1):16-20.
11. Bala C, Xia Y, Meades K. Electron microscopy of laser capsulotomy edge: Interplatform comparison. J Cataract Refract Surg. 2014;40:1382-1389.
12. Nagy ZZ, Dunai A, Kranitz K, et al. Evaluation of femtosecond laser-assisted and manual clear corneal incisions and their effect on surgically induced astigmatism and higher-order aberrations. J Refract Surg. 2014;30(8):522-525.
13. Hou JH, Prickett AL, Cortina AS, et al. Safety of femtosecond laser- assisted cataract surgery performed by surgeons in training. Letter to Editor. J Refract Surg. 2015;31(1):69-70.
Important Product Information for the LenSx™ Laser
Caution
United States Federal Law restricts this device to sale and use by or on the order of a physician or licensed eye care practitioner.
Indication
The LenSx® Laser is indicated for use in patients undergoing cataract surgery for removal of the crystalline lens. Intended uses in cataract surgery include anterior capsulotomy, phacofragmentation, and the creation of single plane and multi-plane arc cuts/incisions in the cornea, each of which may be performed either individually or consecutively during the same procedure.
Restrictions
- Patients must be able to lie flat and motionless in a supine position.
- Patient must be able to understand and give an informed consent.
- Patients must be able to tolerate local or topical anesthesia.
- Patients with elevated IOP should use topical steroids only under close medical supervision.
Contraindications
- Corneal disease that precludes applanation of the cornea or transmission of laser light at 1030 nm wavelength
- Descemetocele with impending corneal rupture
- Presence of blood or other material in the anterior chamber
- Poorly dilating pupil, such that the iris is not peripheral to the intended diameter for the capsulotomy
- Conditions which would cause inadequate clearance between the intended capsulotomy depth and the endothelium (applicable to capsulotomy only)
- Previous corneal incisions that might provide a potential space into which the gas produced by the procedure can escape
- Corneal thickness requirements that are beyond the range of the system
- Corneal opacity that would interfere with the laser beam
- Hypotony or the presence of a corneal implant
- Residual, recurrent, active ocular or eyelid disease, including any corneal abnormality (for example, recurrent corneal erosion, severe basement membrane disease)
- History of lens or zonular instability
- Any contraindication to cataract or keratoplasty
- This device is not intended for use in pediatric surgery.
Warnings
The LenSx® Laser System should only be operated by a physician trained in its use.
The LenSx® Laser delivery system employs one sterile disposable LenSx® Laser Patient Interface consisting of an applanation lens and suction ring. The Patient Interface is intended for single use only. The disposables used in conjunction with ALCON® instrument products constitute a complete surgical system. Use of disposables other than those manufactured by Alcon may affect system performance and create potential hazards.
The physician should base patient selection criteria on professional experience, published literature, and educational courses. Adult patients should be scheduled to undergo cataract extraction.
Precautions
- Do not use cell phones or pagers of any kind in the same room as the LenSx® Laser.
- Discard used Patient Interfaces as medical waste.
AEs/Complications
- Capsulotomy, phacofragmentation, or cut or incision decentration
- Incomplete or interrupted capsulotomy, fragmentation, or corneal incision procedure
- Capsular tear
- Corneal abrasion or defect
- Pain
- Infection
- Bleeding
- Damage to intraocular structures
- Anterior chamber fluid leakage, anterior chamber collapse
- Elevated pressure to the eye
- Attention
- Refer to the LenSx® Laser Operator’s Manual for a complete listing of indications, warnings and precautions.


