As ophthalmologists work to integrate the femtosecond laser into surgical practice, we are faced with a multitude of challenges, including logistics, cost, space, and surgical technique. The integration of the femtosecond laser into cataract surgery requires the surgeon to be prepared for an entirely different procedure, similar to the shift that occurred with the advent of phacoemulsification. Below is an outline of what to expect.
If nuclear rotation is poor, either a cross-chop or a reverse-chop technique can be employed to initiate nuclear disassembly.
Capsulorhexis
The capsulorhexis is performed first and takes 1.5 to 18 seconds to complete. Studies have shown that the femtosecond laser does this with greater accuracy, precision, and reproducibility than a manual continuous curvilinear capsulorhexis. Studies have also shown that the laser results in more stable refraction due to minimized IOL tilt and lens decentration.1-2
Once the patient is under the operating microscope, the paracentesis and main incision can be opened. After an ophthalmic viscosurgical device is injected into the eye, the surgeon can readily assess for any incomplete areas or tags and can remove the laser-created rhexis flap.
Corneal Incisions
Femtosecond lasers also have the ability to produce very accurate corneal relaxing incisions. The use of the laser to create these incisions may provide a more stable and accurate result over the use of toric IOLs, the effect of which can be limited by IOL rotation after implantation.3
These lasers can create complex and precise corneal incisions. Some surgeons feel that the advantage of using the laser is that it can be difficult to achieve consistent incision length and architecture manually. There may be difficulty adjusting to the changes in wound architecture, and some report that there is a learning curve for localizing the wound or paracentesis and entering the eye through these new incisions.
Cortical removal can be more challenging because of the lack of fimbriated ends, as the cortex is sharply dilineated by the laser. This can induce greater stretch and edema to the primary wound.
Hydrodissection
This step has the potential to create the most angst because of the possible air bubbles that can occupy space between the lens and the posterior capsule. There is little in the published literature regarding the rate of posterior capsular rupture from hydrodissection with laser cataract surgery. It goes without saying, though, that one should proceed with caution and gentle finesse during this step, decompressing the nucleus after each pass of fluid. Sometimes, the air can actually assist in “pneumodissection” and cleave the desired space if one begins hydrodissection 180° away from the location of the trapped air. The fluid can push the air anteriorly around and over the lens equator to propagate the cleaved plane between the nucleus and cortex.
Nucleus Removal
After the superficial cortex is removed, either a divide-and-conquer or chopping technique may be used. The grooves made by the laser are extremely narrow, and therefore adjustments must subsequently be made with regard to technique and the second instrument used.4
A few published studies report reduced ultrasonic energy utilization after laser lens fragmentation. Other studies report that laser cataract surgery causes less corneal swelling in the early postoperative period, which may be related to trauma to the endothelial cells during the procedure.5
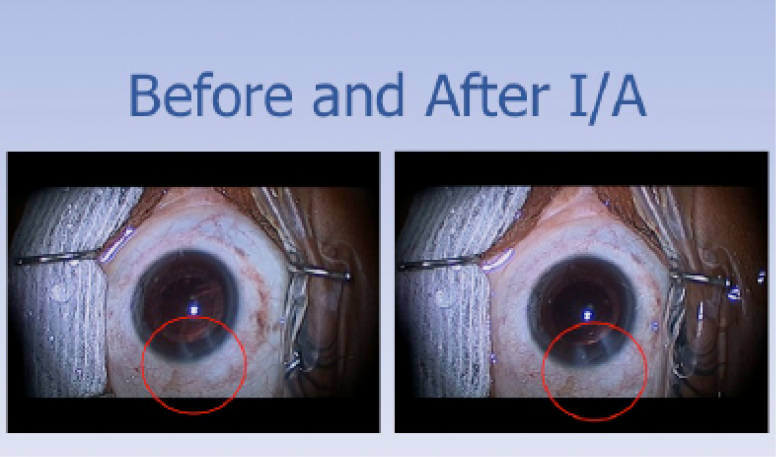
Before and after I/A of cortical fibers. Notice the temporal wound edema from the greater manipulation within the wound to perform cortical removal.
Cortical Removal
Cortical removal can be more challenging than with traditional phacoemulsification. This is likely multifactorial and is, in part, due to the sharp cutoff of the cortex where the rhexis is created by the laser, resulting in a lack of fimbriated cortical fibers to aspirate, particularly when the single handpiece is used.4 Visualization can also be more challenging because of the whitening that occurs from the laser. Poor hydrodissection can also lead to greater difficulties with cortical cleanup.
Conclusion
Laser cataract surgery seems to be safe, efficient, and reproducible. An awareness of the idiosyncrasies of the laser and the procedure is key in making a smooth transition to this new technique.
1. Friedman NJ, Palanker DV, Schuele G, et al. Femtosecond laser capsulotomy. J Cataract Refract Surg. 2011;37:1189-1198.
2. Kranitz K, Mihaltz K, Sandor GL, Takacs A, Knorz MC, Nagy ZZ. Intraocular lens tilt and decentration measured by Scheimpflug camera following manual or femtosecond laser- created continuous circular capsulotomy. J Refract Surg. 2012;28:259-263.
3. Hoffart L, Proust H, Matonti F, et al. Correction of postkeratoplasty astigmatism by femtosecond laser compared with mechanized astigmatic keratotomy. Am J Ophthalmol. 2009;147:779-787.
4. Donaldson KE, Braga-Mele R, Cabot F, et al. Femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2013;39:1753-1763.
5. Nagy Z, Takacs A, Filkorn T, Sarayba M. Initial clinical evaluation of an intraocular femtosecond laser in cataract surgery. J Refract Surg. 2009;25:1053-1060.



