In clinical practice, surgeons tend to offer laser cataract surgery to their younger, healthier patients with the least challenging cataracts. However, I am often asked about whether this procedure can be performed in more complex eyes. This article presents three challenging cases where the femtosecond laser made a big difference in my ability to successfully perform phacoemulsification and implant IOLs that met my patients’ refractive goals.
Case 1: Traumatic Cataract
A 26-year-old man presented with counting fingers vision. He had a traumatic cataract with zonular dehiscence and lens subluxation of about 4 clock hours. There was no retinal detachment, and IOP was 17 mm Hg. Corneal topography showed 1.37 D of with-the-rule astigmatism at 75˚, indicating he could be a good candidate for limbal relaxing incisions (LRIs).
The capsulorhexis is a limiting factor in cases of traumatic cataracts with zonular dehiscence. Because the subluxed lens is decentered and has poor zonular support, it can be difficult to center the capsulotomy on the dislocated capsular bag. I planned a 5.1-mm-diameter capsulotomy using scanned-capsule centration on the Catalys laser (Johnson & Johnson Vision). Even in routine cases, the pupil center can change with dilation, so I prefer to use scanned capsule centration when possible.
Video 1 | The femtosecond laser setting adjustments and laser portion of the procedure in a complex traumatic cataract case.
This patient had a little bit of anterior subcapsular fibrosis, so I increased the pulse energy to 6 µJ. I chose quadrant segmentation and 800-µm grid spacing for the softening pattern. Tighter grid spacing can reduce the effective phaco time,1 but the tradeoff is that very small cubes, especially in denser nuclei, can hide under the iris and become retained lens fragments, so I usually opt for a 600- to 800-µm grid. Finally, I planned two anterior penetrating astigmatic keratotomy (AK) incisions at 75˚, 80% depth, and 9-mm optical zone to correct his astigmatism.
The laser portion of the case proceeded mostly uneventfully, although, due to a very irregularly dilated pupil, the laser imaging was not able to locate the iris, so I had to manually identify the iris surfaces (Video 1).
My initial plan was to use Ahmed capsular tension segments (FCI Ophthalmics) to stabilize the area of zonular dehiscence during phacoemulsification. Although these segments are highly effective, they must be sutured to the sclera. In this case, it turned out that I was able to use a standard capsular tension ring because the laser capsulotomy was so well centered (Figure 1, Video 2). I implanted an aspheric monofocal IOL, and the patient achieved 20/20 uncorrected vision after surgery.
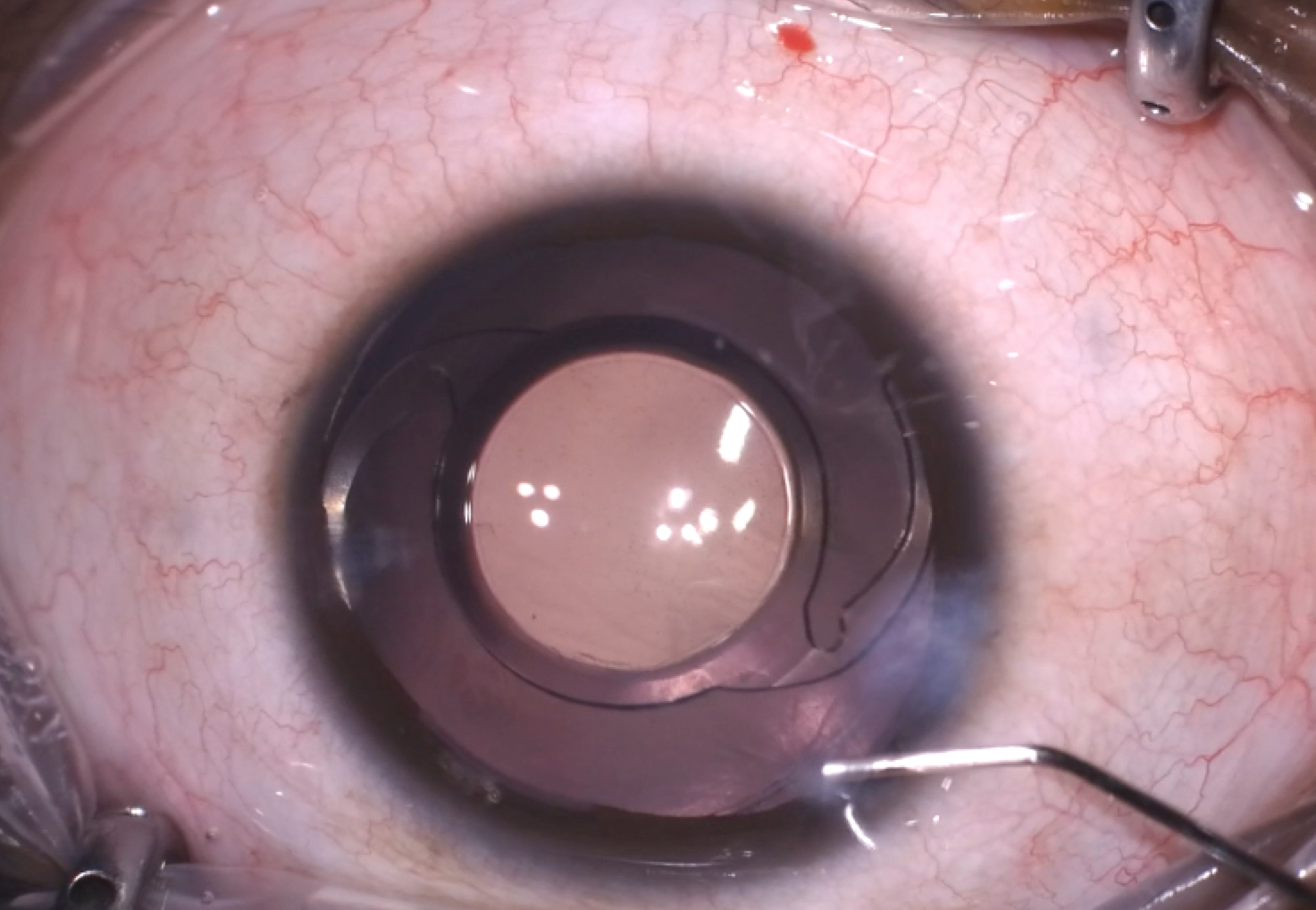
Figure 1 | A well-centered capsulotomy in this traumatic cataract case allowed for stable positioning of the lens despite zonular dehiscence and lens subluxation.
Video 2 | The phaco and IOL portion of the procedure.
Case 2: Prior RK
A 57-year-old woman presented for cataract surgery. She had previously undergone radial keratotomy (RK) and had 12 old RK incisions (Figure 2) and four additional AK incisions. She had significant astigmatism of 2.35 D. Despite the number of incisions, topography showed that her astigmatism was fairly regular within the visual axis, so I decided to implant a toric IOL. Perfect centration of toric lenses is key to their effectiveness, and we know that a well-centered capsulotomy can help to maintain the lens in the correct position. Thus, my preference in this case was to perform laser cataract surgery.
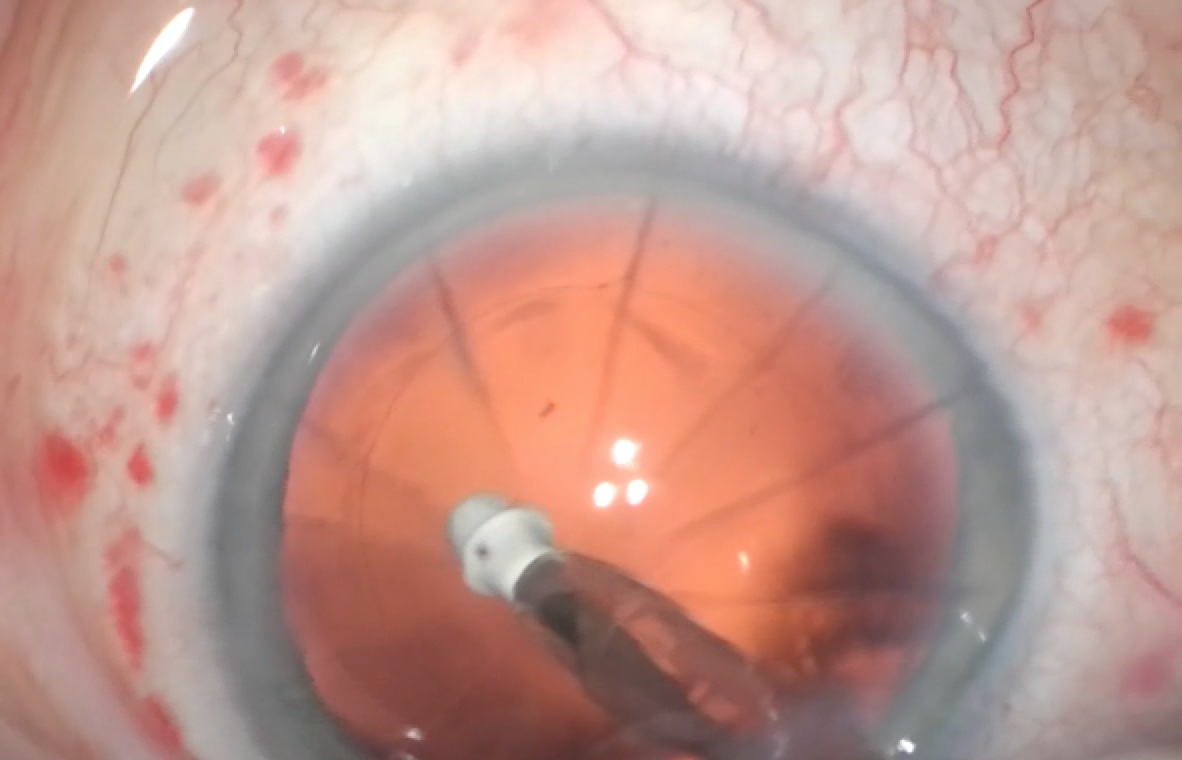
Figure 2 | Cataract surgery in an eye with 12 RK incisions and four AK incisions, shown here during cortical cleanup.
The biggest concern with using the femtosecond laser in a case like this (or, for that matter, in any eye with corneal scars and opacity) is that the hypertrophic RK and AK incisions can block the laser; thus, the laser settings must be adjusted accordingly. I increased the pulse energy to 8 µJ from the typical 4 µJ to ensure that the laser could cut through the scars and achieve a free-floating capsulotomy. This patient ended up with 20/25 uncorrected vision—an excellent outcome in an eye with 16 incisions.
Case 3: Hypermature Cataract
A patient presented with a total mature cataract and only light perception vision. He was interested in spectacle independence. I counseled him that I might need to use an extracapsular technique: Because the lens was so dense, I was not sure it could be removed with phacoemulsification, particularly because he had small pupils and floppy iris syndrome from tamsulosin use. Nevertheless, I decided to see if the laser could help me soften this lens.
Imaging can be difficult in such dense nuclei, but I was able to obtain good quality imaging and surface fits with the laser. I used the sextant pattern for lens segmentation and reduced the grid spacing to 450 µm. I then performed three repetitions of the laser segmentation pass. Despite the patient’s small pupil, I was able to create a 4.6-mm capsulotomy.
In the end, I was able to proceed with phaco—in fact, the softening was so effective that the phaco portion was relatively easy—and implanted a toric extended depth of focus IOL.
CONCLUSION
The key benefits of laser cataract surgery—scanned capsule centration, a perfect capsulotomy, and the ability to precisely correct astigmatism at the time of surgery—can be applied to complex cases if care is taken to adjust laser settings accordingly.
1. Conrad-Hengerer I, Hengerer FH, Schultz T, Dick HB. Effect of femtosecond laser fragmentation of the nucleus with different softening grid sizes on effective phaco time in cataract surgery. J Cataract Refract Surg. 2012;38(11):1888-1894.



