Corneal blood staining (CBS) is a complication of hyphema and increased intraocular pressure (IOP). Spontaneous clearing can take up to 3 years, starting at the periphery.1 Factors that increase the risk of CBS include total hyphema, rebleeding, and endothelial dysfunction.2 Management options for hyphema with increased IOP include trabeculectomy, anterior chamber washout, and pharmacotherapy with topical steroids and cycloplegics.3
CASE
A 22-year-old white man presented with right eye pain and vision loss. He had suffered a nail gun injury to the lower eyelid 5 days prior. On follow-up day 1, he woke up with decreased vision in the right eye. He had no significant past medical, ocular, or surgical history. His right eye exam indicated light perception vision, not visible pupils, no relative afferent pupillary defect, IOP of 27 mm Hg, 3+ conjunctival injection, 95% hyphema, and no retinal detachment or mass on B-scan ultrasonography. He was prescribed prednisolone 1% hourly to prevent rebleeding and atropine 1% twice a day for pain.4
One week later, the patient’s IOP had increased to 41 mm Hg, and CBS was first noted. An anterior chamber washout was performed, after which a blood clot was noted in the anterior chamber, as were many areas of iridodialysis. The paracentesis wound was enlarged to remove the clot, which was complicated by iris prolapse. The next day, vision was hand motion, IOP was 26 mm Hg, and there was a 7-mm area of CBS in the right eye. Timolol was added.
One month later, the patient’s vision was light perception, and the hyphema had resolved. However, there was still CBS present, and a mature cataract was noted (Figure 1). Surgery was delayed, and the patient was monitored monthly. His vision remained stable at hand motion at 1 foot, IOP remained below 20 mm Hg, and CBS continued to improve.
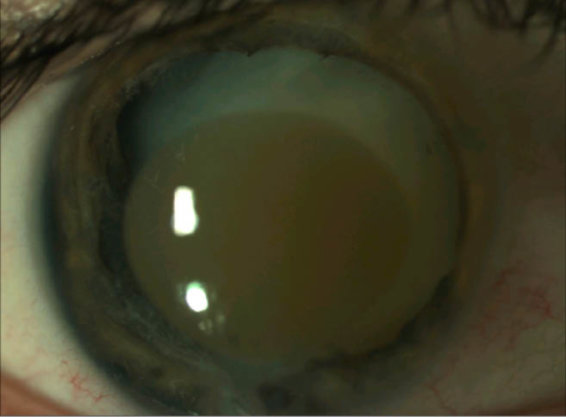
Figure 1 | Postoperative month 3 with corneal blood staining and mature cataract present.
After 2 years, the CBS improved significantly (Figure 2). Phacoemulsification with IOL implantation was performed. The next day, the patient’s uncorrected vision in the right eye was 20/70, and IOP was 17 mm Hg. A month later, his vision was 20/30-2 with -0.50 +0.75 X 45 refraction in the right eye. Optical coherence tomography showed normal foveal contour with no cystoid macular edema.
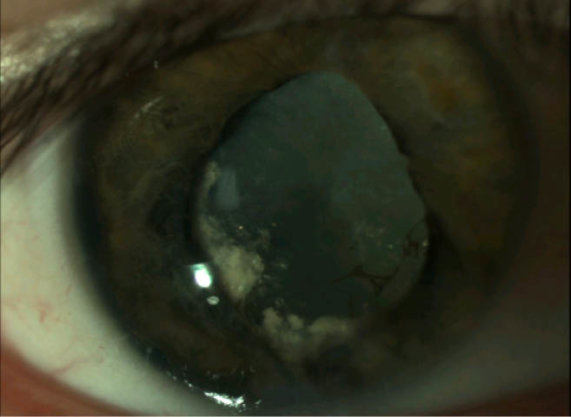
Figure 2 | Postoperative year 2 exhibiting improved corneal blood staining.
Video | Laser cataract surgery in a patient with previous CBS.
DISCUSSION
Etiology of endothelial damage, seen consistently in CBS, remains unclear. Messmer et al found extracellular hemoglobin concentrated in the posterior stroma, whereas intracellular hemosiderin predominated anteriorly. They suggest that hemoglobin in the anterior chamber crosses an intact Descemet membrane, and keratocytes in the posterior stroma phagocytize hemoglobin to produce hemosiderin. Once the amount of hemoglobin overwhelms the keratocytes’ capacity to metabolize it, they undergo necrosis.5
This observed cell death might be due to photosensitivity, as McDonnell et al found that hematoporphyrin derivatives accumulate in the cells, and when the blood-stained cornea is exposed to light, cytotoxic oxygen particles form. These are potent oxidizing agents that cross-link the plasma membrane, causing cell damage.6 Although more studies on prevention and management of CBS are needed, this and previous studies show that aggressive treatment of increased IOP, evacuation of hyphema, and limiting sun exposure may improve outcomes.
1. Brodrick JD. Corneal blood staining after hyphaema. Br J Ophthalmol. 1972;56:58.
2. Beyer TL, Hirst LW. Corneal blood staining at low pressures. Arch Ophthalmol. 1985;103:654-655.
3. Graul TA, Ruttum MS, Lloyd MA, at al. Trabeculectomy for traumatic hyphema with increased intraocular pressure. Am J Ophthalmol. 1994;117:155-159.
4. Walton W, Von Hagen S, Grigorian R, et al. Management of traumatic hyphema. Surv Ophthalmol. 2002;47(4):297.
5. Messmer EP, Gottsch J, Font RL. Blood staining of the cornea: a histopathologic analysis of 16 cases. Cornea. 1984;3:205-212.
6. McDonnell PJ, Gritz DC, McDonnell JM, et al. Fluorescence of Blood-Stained Cornea. Cornea. 1991;10(5):445-449.





