By now, most ophthalmologists are likely familiar with what is considered the typical dry eye patient. However, while postmenopausal women, contact lens wearers, and surgical candidates constitute the majority of individuals evaluated for dry eye disease (DED), developing trends suggest growing disease incidence among less obvious populations. This changing demographic profile is fueled in part by greater awareness and improved detection but also by shifts in patients’ visual demands.
The changing demographics of DED, coupled with an evolving understanding of its multifactorial nature, should challenge us to rethink our commonly held beliefs about this ocular surface condition. The classic patient profile will certainly still be relevant for the foreseeable future, but it may also be time to think outside the box and to look for signs and symptoms in so-called atypical populations that are becoming more normal.
A LOOK AT THE NUMBERS
Changing demographics in a disease state are usually due to multiple factors. The increased focus on DED over the past decade against a backdrop of improved diagnostics for understanding the signs and symptoms are certainly one reason why we are detecting more disease. We also have the ability to detect disease earlier, which can lead to swelling numbers. In addition, changing vision habits in our society have the potential to negatively affect the ocular surface; in particular, the use of digital devices is becoming much more prevalent, from tablets in the classroom, to GPS devices in cars, to computers, to smartphones, and to the explosion of video-gaming culture.
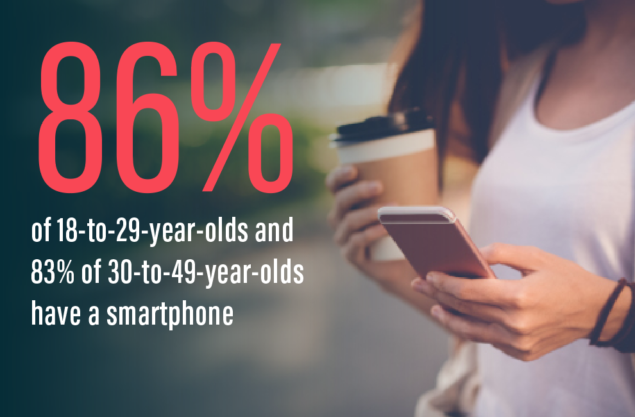
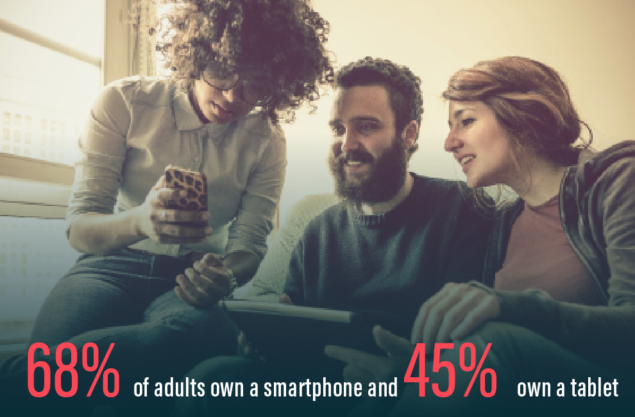
There are numbers to back these observations. The Pew Research Foundation noted that, while smartphone ownership has nearly reached saturation, 86% of 18-to-29-year-olds and 83% of 30-to-49-year-olds have a smartphone; overall, 68% of adults own a smartphone—an increase from 35% in 2011—and tablet ownership is about 45%.1 The explosion of video game playing has led some researchers to suggest the potential for pathologic video game addiction, with alarming statistics showing that 72% of households own gaming consoles and some players log more than 50 hours a week playing video games.2 Yet, gaming is not exclusively teenage behavior: The Entertainment Software Association, a self-described advocacy group for the $22 billion-a-year industry, boasts that the average gamer is 36-years-old, with 73% of gamers over age 18.3

Those statistics paint a picture where dry eye is much more likely to occur in patient types that do not fall into the so-called typical categories. Studies show that approximately 12% of men and 13% of women aged 21 to 34 years have signs and/or symptoms of DED.4 The rise in those age brackets coincides with a veritable explosion in the total number of cases: Dry eye affects about 29 million adults,4,5 or about 40% of the American population.6 It is now understood that an expanding number of risk factors can incite signs and symptoms of DED, including contact lens wear, ocular surgery, female gender, use of certain medications, occupation, presence of autoimmune diseases, use of digital devices, environment, diabetes, age, and diet.4,7-10
THE IMPORTANCE OF INFLAMMATION
The availability of advanced diagnostics for DED, including tear osmolarity testing (TearLab), and the ability to review the meibomian glands in close detail (TearScience) has helped practitioners understand the functional aspects of the dry eye entity. From these diagnostics, we have learned that the signs of the disease do not always correlate with the symptoms. Increased attention on the dry eye space over the past 5 to 10 years has significantly increased our knowledge of the disease process, which has been used to develop objective diagnostics. Those improved diagnostics showed the importance of inflammation as a common element underscoring the various etiologies; this, in turn, suggests the benefit of addressing the inflammatory component of DED to increase the ability of the eye to produce tears and restore the natural defense and compensatory mechanisms.
The implications for tear film dysfunction as a consequence of DED and, specifically, the inflammatory cascade that is a cause and trigger may help explain why increased digital device use can lead to a growing incidence of disease in new populations. It seems entirely plausible that prolonged use of smartphones, tablets, and the like could have several implications for DED, including that these devices may emit low level thermal energy that dries the ocular surface. In addition, their use may alter blink rates, causing a decrease in both quantity and quality of the blink response. As a result of decreased blinking, meibum is not expressed and is instead impacted within the gland, likely triggering a negative feedback loop that stops meibum production; because meibum is not expressed, the occluded gland leads to pressure atrophy and scars, yielding the inflammatory cascade that has implications for causing and/or triggering ocular surface disease.
WHAT DOES IT ALL MEAN?
Thinking about the changing demographics of DED should be more than an academic exercise, especially if the trends suggest a different approach to diagnosis and treatment. As diagnostics get more sophisticated, they will allow us to adopt a treatment schema that is more specific to the underlying cause. The traditional means for assessing DED, such as Schirmer testing, yield little actionable information. On the other hand, tests like InflammaDry (RPS) tell us pretty definitively whether inflammation is present, and, if it is, there are well-established therapeutic treatment options (cyclosporine ophthalmic emulsion 0.05% [Restasis, Allergan]; lifitegrast 5% [Xiidra, Shire]) to address that. In other instances, analysis of the meibomian glands reveals whether occlusion is playing a role in inciting inflammation in a self-perpetuating cycle.
In truth, blaming the changing demographics on digital devices would be to vastly simplify dry eye, an ocular surface disease we have come to learn is multifactorial and extraordinarily complex. In thinking about the future of DED, however, there are promising trends in drug and device development that may simplify treatment even further. In some ways, the movement in the dry eye space is indicative of larger trends in eye care, where research that is unveiling the nuances of pathophysiology is also yielding high technology that advances our ability to detect chronic disease earlier in its natural history, enhancing our ability to treat patients, save their vision, and improve quality of life.
1. Technology Device Ownership: 2015. Pew Research Center. https://www.pewinternet.org/2015/10/29/technology-device-ownership-2015. Accessed November 14, 2016.
2. Gentile DA, Choo H, Liau A, et al. Pathological video game use among youths: a two-year longitudinal study. Pediatrics. 2011;127(2):e319-e329.
3. Industry Facts. Entertainment Software Association. https://www.theesa.com/about-esa/industry-facts. Accessed November 14, 2016.
4. Paulsen AJ, Cruickshanks KJ, Fischer ME, et al. Dry eye in the beaver dam offspring study: prevalence, risk factors, and health-related quality of life. Am J Ophthalmol. 2014;157(4):799-806.
5. Schaumberg DA, Sullivan DA, Buring JE, Dana MR. Prevalence of dry eye syndrome among US women. Am J Ophthalmol. 2003;136(2):318-326.
6. US Census Bureau. Age and sex composition: 2010. www.census.gov/prod/cen2010/briefs/c2010br-03.pdf. May 2011. Accessed June 19, 2015.
7. The epidemiology of dry eye disease: report of the Epidemiology Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007;5(2):93-107.
8. Afsharkhamseh N, Movahedan A, Motahari H, Djalilian AR. Cataract surgery in patients with ocular surface disease: An update in clinical diagnosis and treatment. Saudi J Ophthalmol. 2014;28(3):164-167.
9. The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007;5(2):75-92.
10. Schargus M, Wolf F, Tony HP, Meyer-Ter-Vehn T, Geerling G. Correlation between tear film osmolarity, dry eye disease, and rheumatoid arthritis. Cornea. 2014;33(12):1257-1261.



