To optimize refractive outcomes following cataract extraction, surgeons must address astigmatism correction. A simple way to manage astigmatism is with implantation of a toric IOL, whether a monofocal or presbyopia-correcting platform. Let us review the key steps for the use of toric IOLs.

PERFORM CAREFUL PATIENT SELECTION
Toric IOLs include the traditional monofocal lenses as well as the recently approved presbyopia-correcting platforms (Figure 1). Surgeons must optimize the cornea prior to insertion of these lenses. Patients with dry eye often have fluctuating astigmatism measurements, so screening and treatment prior to cornea and lens calculations is essential. A careful slit-lamp examination is needed to rule out anterior basement membrane dystrophy and corneal scars; diagnostics such as Placido-disc–based topography can show areas of irregular astigmatism or missing data correlating with these types of pathology.
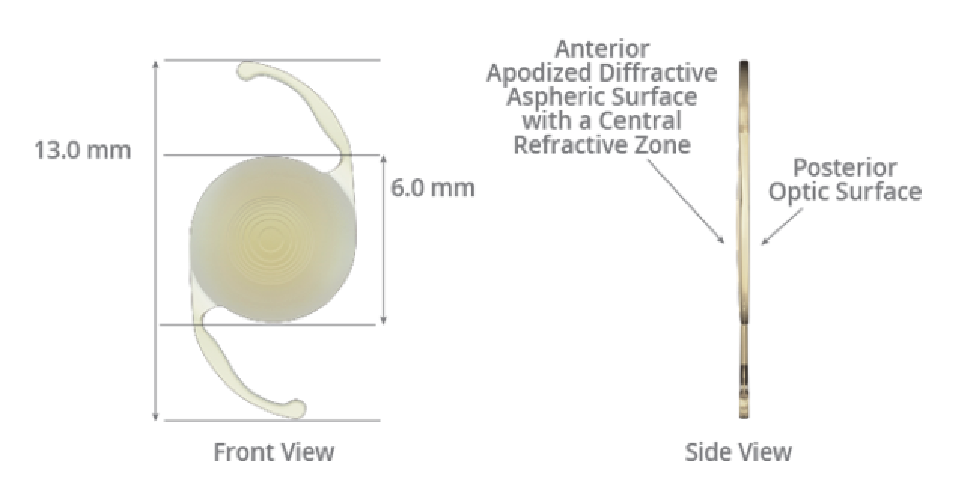
Figure 1. The AcrySof IQ ReSTOR +2.5 Multifocal Toric IOL with ActiveFocus (Alcon) for astigmatism management and presbyopia correction.
Exercise caution when treating patients who wear toric or rigid gas permeable contact lenses, as the amount of warpage is much higher with these lenses compared with soft or scleral lenses. We request that patients be out of soft lenses for 1 week, whereas with toric and hard lenses we suggest 3 weeks. However, contact lens warpage is proportional to the years of wear, so patients need to be out of the lenses and remeasured until stability is determined. This may take months for patients who wear rigid gas permeable lenses, so a discussion about timing and expectations is warranted.

CORRELATE YOUR DATA
You do not need an office full of expensive technology to place a toric lens. A corneal biometry measurement and topography measurement are an absolute minimum, although having a third device as a “tie-breaker” can go a long way.
There are many ways to correlate your data, but simply writing the name of each device, the astigmatism cylinder, and the axis can allow a quick review to ensure that there are no outliers. If outliers exist, go to the raw data to determine if it was a poor study due to technique or if the patient has pathology that was missed. Repeating these tests can confirm that you are using the best data for your patient; for example, we utilize topography on the day of cataract evaluation and repeat that test plus biometry and other topographies on the preoperative visit.

PICK YOUR NOMOGRAM OR CALCULATOR
We are fortunate there are several calculators and nomograms available, but it can be confusing. I suggest picking an online calculator and then correlating the result with a nomogram such as the Baylor nomogram. In my practice, we utilize the Alcon toric calculator, making sure to click the icon for posterior astigmatism. I utilize the biometry data, keeping the surgical astigmatism minimum, as small incisions nowadays do not create much flattening. Once the results are printed, I confirm that the lens choice follows the Baylor nomogram (Figure 2) and that the axis correlates with the other studies.
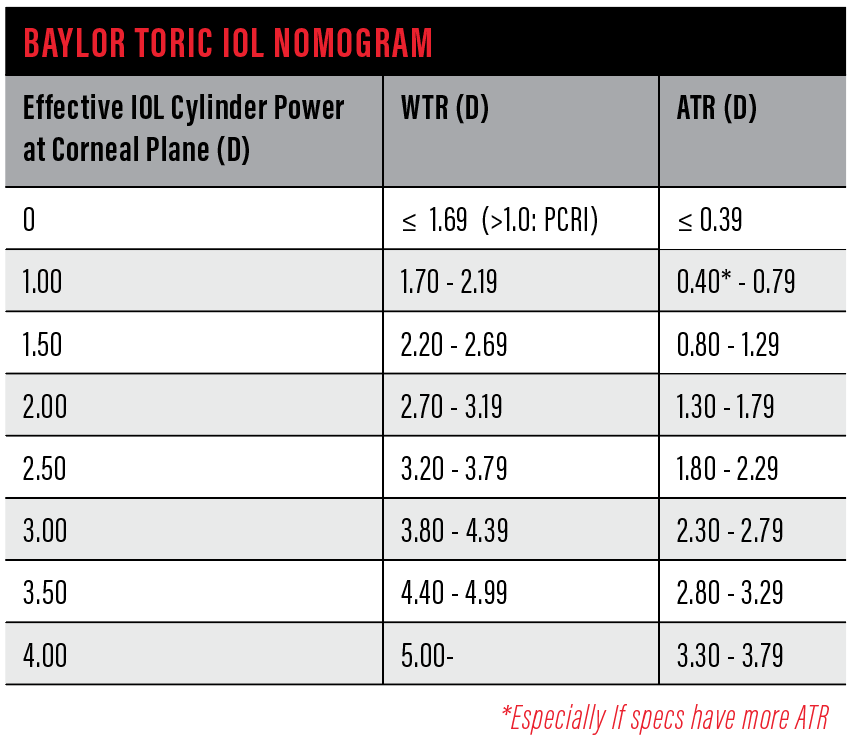
Figure 2. The Baylor Toric IOL Nomogram.

HONE YOUR SURGICAL TECHNIQUE
Studies have shown that patients may have as much as 10° of cyclotorsion once lying flat. Therefore, it is important to mark the axis prior to surgery. Options include marking the patient at the slit lamp if available the day of surgery or using a weighted marker to mark the 0° and 90° axis with the patient sitting up and staring at a distance target (Figure 3). The IOLMaster 700 (Carl Zeiss Meditec) provides an excellent image of the limbus architecture with orientation of the lens based on the biometry data and Barrett calculator (Figure 4).
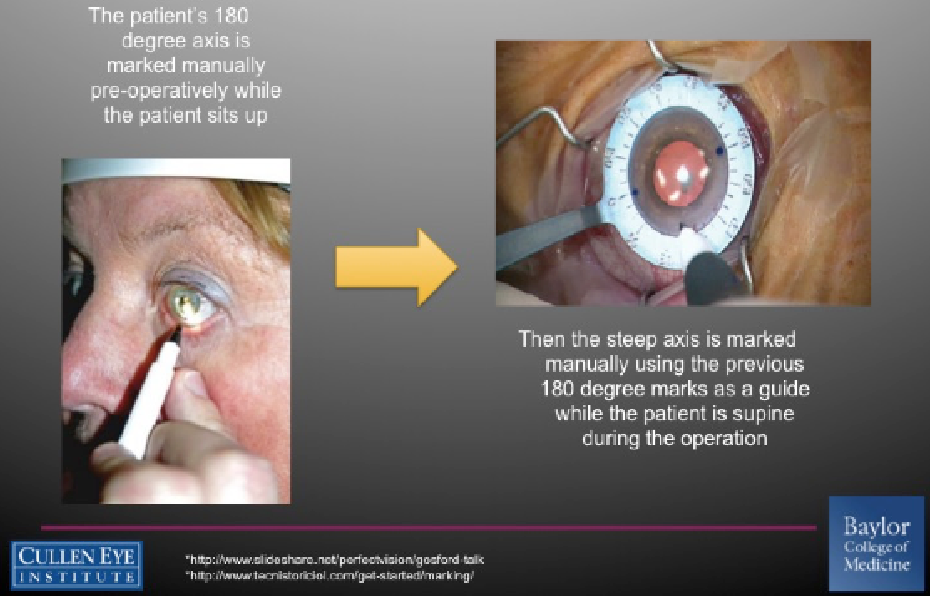
Figure 3. Conventional technique for marking a patient before toric IOL implantation.
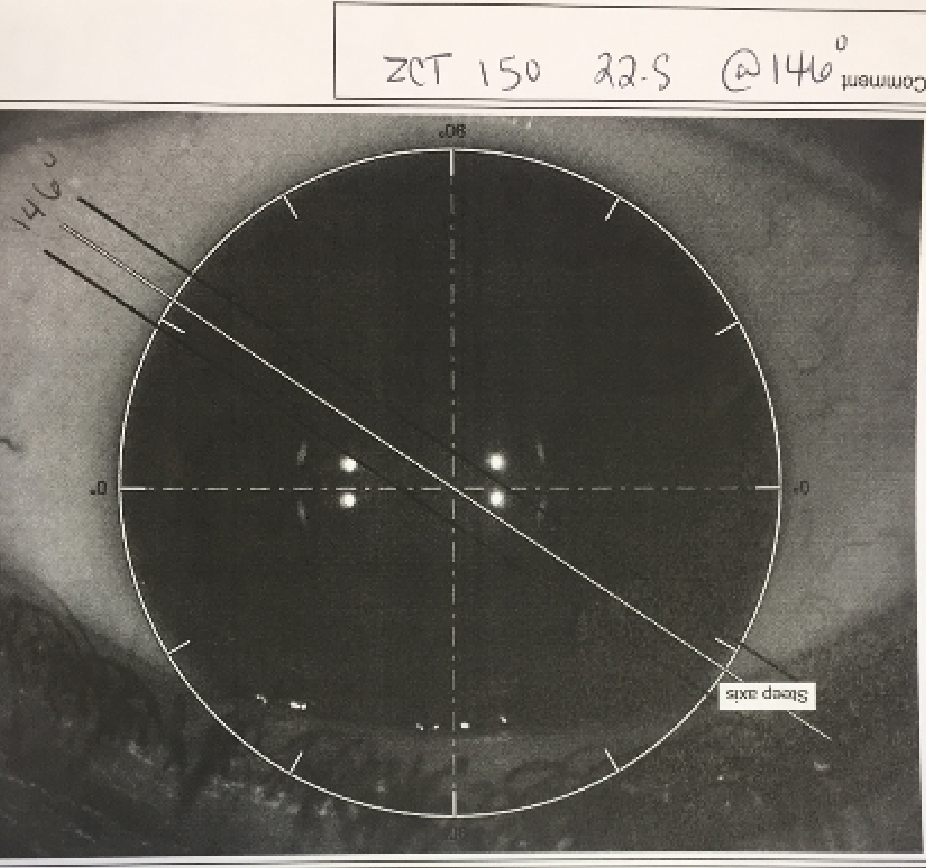
Figure 4. The IOLMaster 700 provides an excellent image of the limbus architecture with orientation of the lens based on the biometry data and Barrett calculator
Image-guided systems such as the Verion (Alcon) can eliminate the need for marking, as preoperative images of the iris and limbus can guide orientation of the lens (Figure 5). Studies have shown the results from image-guided systems to be as effective as marking systems without the need to mark the patient or concern of washing off the mark. These devices may also have programs that can assist in picking the lens and axis.
In the operating room, a few pearls can help prevent intraoperative rotations. First, place the IOL in the axis needed and hold the lens in place when removing the viscoelastic. Then let the anterior chamber form with the irrigation still in the eye and hydrate your paracentesis, continuing to fill as you remove the irrigation handpiece. This prevents the chamber from shallowing and the IOL from rotating again. Always confirm the orientation of the lens even if it means using an instrument to move the iris in patients with smaller pupils.

CONSIDER AN ENHANCEMENT
Postoperative lens orientation and refraction are keys to determine the success of your toric placement. The ideal time to rotate a lens has been shown to be 1 to 3 weeks after surgery—any earlier, the lens may re-rotate; any later, rotation may be difficult due to phimosis.
If the postoperative refraction shows an under- or over-correction of more than 0.50 D of cylinder, you must decide the best way to correct this. The Berdahl & Hardten calculator is helpful for determining how much a toric IOL should be rotated or if it should be exchanged (Figure 5). Either way, the choices are to rotate the lens, to exchange the lens, or to perform a corneal enhancement such as a limbal relaxing incision or surface ablation.
SUMMARY
Toric IOLs are an excellent entry into the premium market for new surgeons, as outcomes are generally excellent. Careful patient selection, use of a calculator and nomogram, and a plan for enhancement can allow superior results for premium patients.



