The essential equipment needed for diagnostic ophthalmology is not universally available, and it is especially limited in emergency situations, primary care centers, and eye examinations camps. Recent technological advances, however, are bringing eye care providers new solutions for telemedicine and smartphone-based ophthalmic assessment. Between widespread use of these devices and the development of specific applications for ophthalmology, smartphones are an ideal tool for patient examination in a resource-limited setting.1 This article provides an overview of some smartphone- or tablet-based solutions that can aid in the clinician’s diagnostic decision-making.
QUANTIFYING VISUAL FUNCTION
Accurate visual acuity assessment is essential to the workup of any patient with visual complaints, especially those presenting in emergency settings. Studies have shown that vision measurements obtained by nonophthalmic emergency department staff using a mobile app were more accurate than those obtained with a Snellen chart.2 Apps such as those described below may serve as valuable tools for nonophthalmic emergency department staff.
Eye Chart Pro. Eye Chart Pro (Dok) is a randomizable visual acuity examination tool. In the app, the user can easily between Snellen and tumbling E charts. Eye Chart Pro is useful for patient triage, house visits, and patients who have memorized the office-based eye chart.
eyeTests Easy. The eyeTests Easy app (George Kong Software) evaluates several parameters, including distance and near visual acuity, color vision, macular function, and peripheral vision. One must remember that the difference in contrast ratio between the high-definition smartphone screen and the near vision cards may result in discrepancies in near visual acuity measurements.
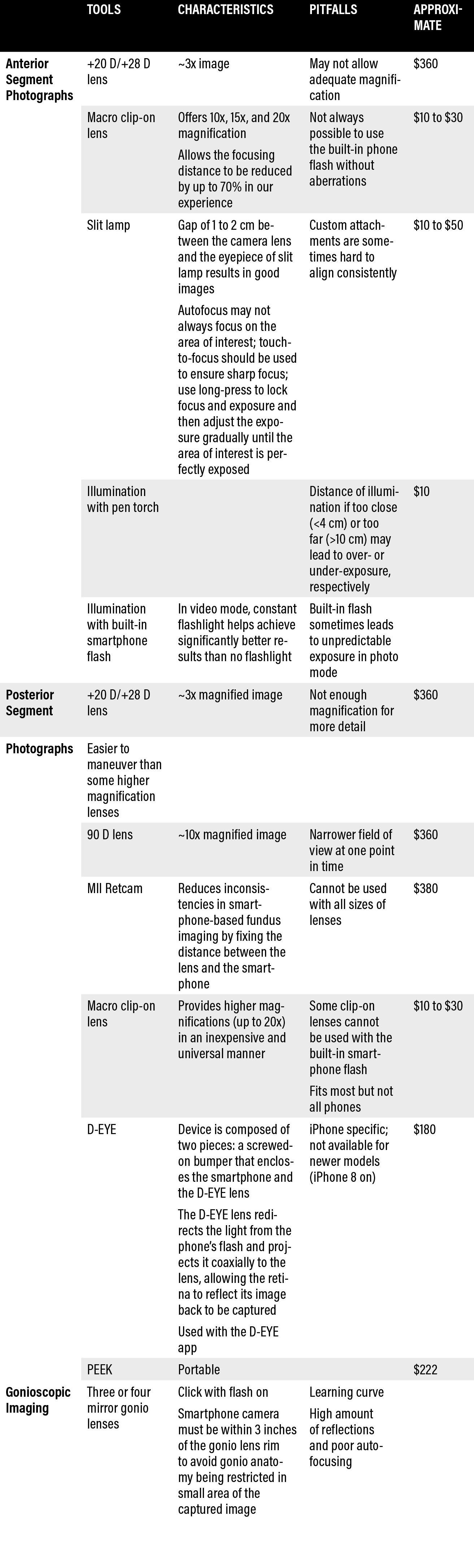
TABLE 1. TOOLS FOR SMARTPHONE-BASED OCULAR PHOTOGRAPHY
BEYOND SELFIES: SMARTPHONE CAMERA APP
Smartphone-based ocular photography has proven utilities in modern ophthalmology, especially for screening and telemedicine. Below are some solutions that utilize of the smartphone’s native camera app.
Anterior segment examination. Studies continue to substantiate the use of smartphone-based photography for anterior segment examination. Be it the use of a dual-camera setup for increased magnification or the use of macro lens attachments to capture highly detailed images, smartphone photography is a practical approach for patient screening, especially in low-resource settings. Newer iPhone models and many Android phones feature multiple-camera setups with varying degrees of magnification. Ideal illumination and framing are essential to ensure a high level of detail and to minimize digital noise. Apps that can be used to capture high-quality photos include Camera FV-5, Open Camera (Android only), or Camera Plus Pro Filmic Pro (iOS only).
In our experience, illumination using a yellow pen-torch at a distance of 4 to 10 cm from the ocular surface is ideal to capture detailed images of the ocular surface without under- or over-exposing any areas in the field of interest. Additionally, the use of a macro clip-on lens (15x magnification) yields significantly better images of the area of interest, as it helps to reduce the focal distance of the iPhone camera and enables better framing. However, caution must be exercised when using additional lenses as they may limit the ability to use the built-in camera flash as the source of illumination due to physical malalignment.
TABLE 2. ACCESS DETAILS FOR APPS AND ONLINE RESOURCES

Smartphone-based gonioscopic imaging. Imaging the angle using a gonio lens attached to a smartphone enables screening of angle closure and brings the advantages of telemedicine to gonioscopy.3 The image is taken with the flash on, as the flash acts as the light source for imaging. All four quadrants (mirrors) must be imaged by walking around the head of the patient in a sequential manner. For dynamic gonioscopy, the video mode (4K, 60 fps) of the native camera app is used with the flash in bulb mode to provide a constant source of light. The only limitation to this approach is that subtle changes in the anterior chamber angles can be missed because of blurred pixels at higher magnification.
Fundus photography. Mydriatic and nonmydriatic fundus images obtained from smartphones have revolutionized fundus screening in ophthalmology.4,5 An emergency doctor can even rule out papilledema using a smartphone prior to doing a lumbar puncture. Smartphone-based fundus photography can also be helpful in endocrinology clinics, neonatology units, and rural and remote settings. With newer, improved cameras and their advanced optics, evaluation of the optic nerve head is possible using a smartphone, even in the absence of an ophthalmoscope.
Additional lenses such as +20 D (Figure 1) and clip-on lenses for smartphones can be used to obtain higher magnification for better visualization of the fundus head. Using the smartphone’s native camera app in video mode or a third-party video recording app such Filmic Pro enables sustained video light, thereby making the fundus examination easier when no dedicated coaxial light source is available.
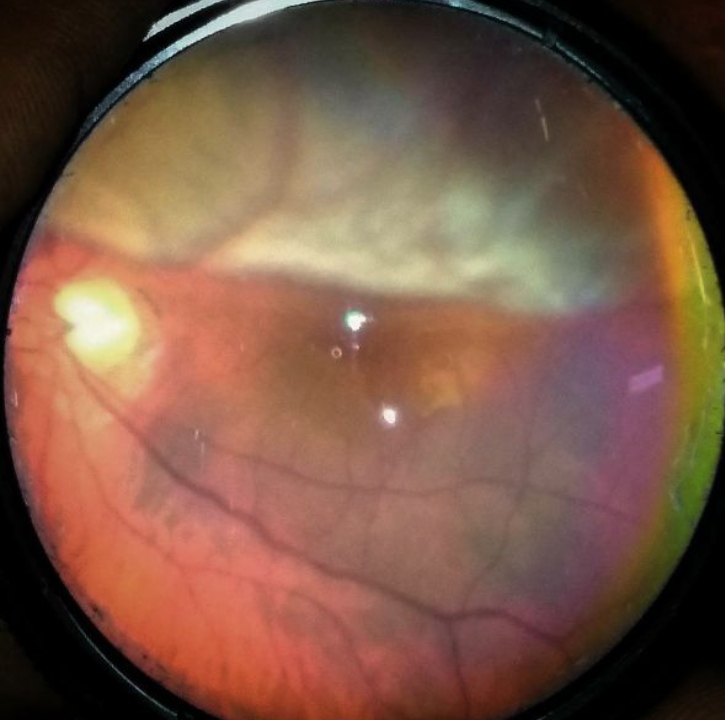
Figure 1 | Post traumatic retinal detachment, captured using a smartphone and +20 D lens.
Basic steps for smartphone-based fundus photography include obtaining a red reflex in the mydriatic eye from 30 to 50 cm from the ocular surface and then moving the smartphone-lens setup toward the ocular surface until the desired level of magnification is achieved.4 The system can be moved in either direction to visualize the corresponding part of the retina, and tap to focus can be used to obtain a sharp focus before capturing the image.
Perimetry apps. Online perimetry tools such as Peristat (www.keepyoursight.org) can be useful for screening glaucomatous or neurological visual field defects. Melbourne Rapid Fields and visualFieldsEasy (Figure 2) are offline alternatives for visual field assessment. Additionally, portable perimetry devices for smartphone-based virtual reality perimetry such as VirtualEye and C3FA have been subject to active research.6-8
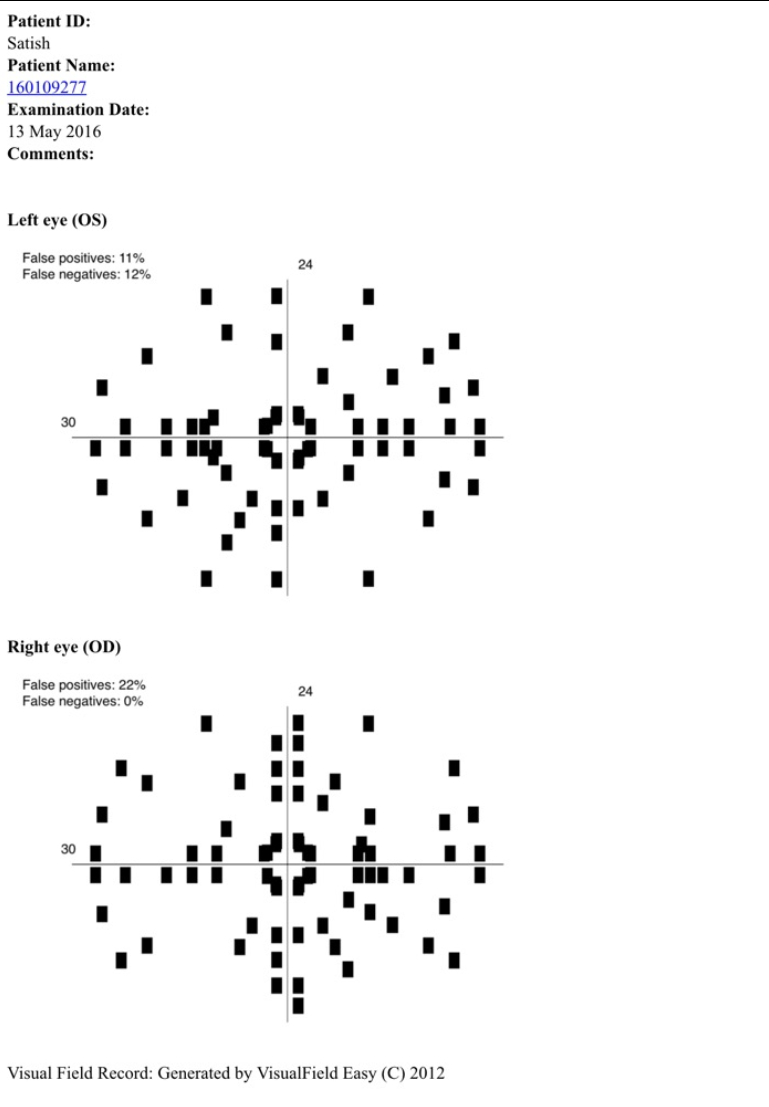
Figure 2 | Visual Field Test results of a patient with glaucomatous discs, generated by VisualField Easy.
Contrast sensitivity apps. Contrast sensitivity is a key component of visual function and one of the earliest abilities to deteriorate in cataract, glaucoma, age-related macular degeneration, and diabetic eye disease. Evaluating contrast sensitivity may enable earlier disease diagnosis and intervention, thereby helping to prevent irreversible vision loss.9 Newer automated online methods include the Spaeth/Richman Contrast Sensitivity Test, Variable Contrast Sensitivity Chart, and Berkeley Contrast Squares (Figure 3).10
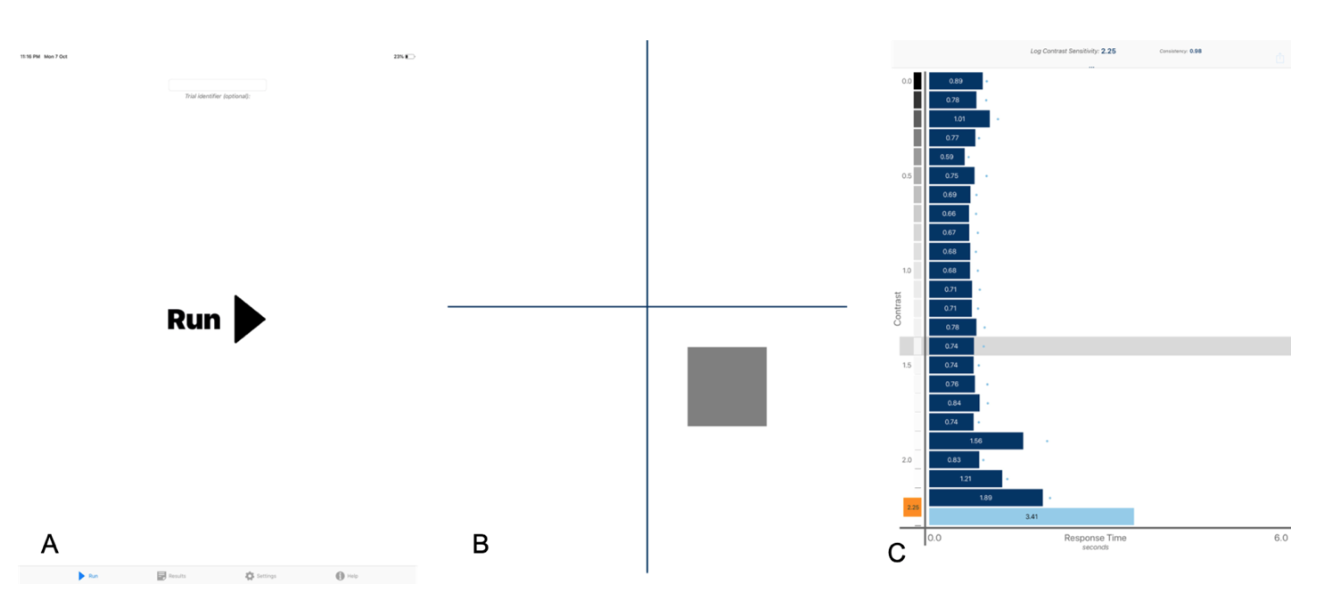
Figure 3 | Berkeley contrast sensitivity. The user taps run to start the test (A); a four-quadrant test with blinking squares of different contrasts appears (B); and the results per response with logarithmic contrast sensitivity are calculated (C)
AI-based systems. Deep learning and AI are revolutionizing ophthalmology with automation in diagnostics and screening.11-13 These systems analyze test images against a reference model using AI and deep learning algorithms to identify pathologic changes. Netra.AI (Leben Care Technologies) is one such AI-based system that can be used to evaluate glaucomatous fundus photographs. Several studies have also looked at different deep learning techniques to detect glaucomatous optic neuropathy from disc photographs.14
CONCLUSION
Smartphones and other digital devices are revolutionizing the eye care provider’s ability to examine patients, particularly when limited resources are available. As these technologies continue to advance, additional smart resources will undoubtedly become available for the benefit of patients and practitioners alike.
1. Are smartphones the solution to eye care in developing countries? Borgen Project. https://borgenproject.org/smartphone-eye-care-solutions/. Accessed January 3, 2020.
2. Pathipati AS, Wood EH, Lam CK, Sáles CS, Moshfeghi DM. Visual acuity measured with a smartphone app is more accurate than Snellen testing by emergency department providers. Graefes Arch Clin Exp Ophthalmol. 2016;254:1175-1180.
3. Kumar N, Francesco B, Sharma A. Smartphone-based gonio-imaging: a novel addition to glaucoma screening tools. J Glaucoma. 2019;28(9):e149-e50.
4. Pujari A, Mukhija R, Chawla R, Phuljhele S, Saxena R, Sharma P. Smartphone-based evaluation of the optic nerve head. Indian J Ophthalmol. 2018;66(11):1617-1618.
5. Russo A, Morescalchi F, Costagliola C, Delcassi L, Semeraro F. A novel device to exploit the smartphone camera for fundus photography. J Ophthalmol. 2015;823139.
6. PeriScreener. www.periscreener.com. Accessed December 1, 2019.
7. C3 Field Analyser. www.c3fields.com. Accessed December 1, 2019.
8. Gardiner SK, Crabb DP. Examination of different pointwise linear regression methods for determining visual field progression. Invest Ophthalmol Vis Sci. 2002;43(5):1400-1407.
9. Ichhpujani P, Thakur S, Spaeth GL. Contrast sensitivity and glaucoma. J Glaucoma. 2020;29(1):71-75.
10. Thakur S, Ichhpujani P, Kumar S, Kaur R, Sood S. Assessment of contrast sensitivity by Spaeth Richman Contrast Sensitivity Test and Pelli Robson Chart Test in patients with varying severity of glaucoma. Eye. 2018;32(8):1392-1400.
11. Appropriateness of Treating Glaucoma Suspects RAND Study Group. For which glaucoma suspects is it appropriate to initiate treatment? Ophthalmology. 2009;116(4):710-716.
12. Thompson AC, Jammal AA, Medeiros FA. A deep learning algorithm to quantify neuroretinal rim loss from optic disc photographs. Am J Ophthalmol. 2019;201:9-18.
13. Al-Aswad LA, Kapoor R, Chu CK, et al. Evaluation of a deep learning system for identifying glaucomatous optic neuropathy based on color fundus photographs. J Glaucoma. 2019;28(12):1029-1034.
14. Raghavendra U, Fujita H, Bhandary SV, Gudigar A, Tan JH, Acharya UR. Deep convolution neural network for accurate diagnosis of glaucoma using digital fundus images. Inform Sciences. 2018;441:41-49.
15. Mariakakis A, Wang E, Patel S, Wen JC. A smartphone-based system for assessing intraocular pressure. Conference Proc IEEE Eng Med Biol Soc. 2016; 2016:4353-4356.
16. Bastawrous A, Giardini ME, Bolster NM, et al. Clinical validation of a smartphone-based adapter for optic disc imaging in Kenya. JAMA Ophthalmol. 2016;134(2):151-158.




