Sessions














































Sessions






















































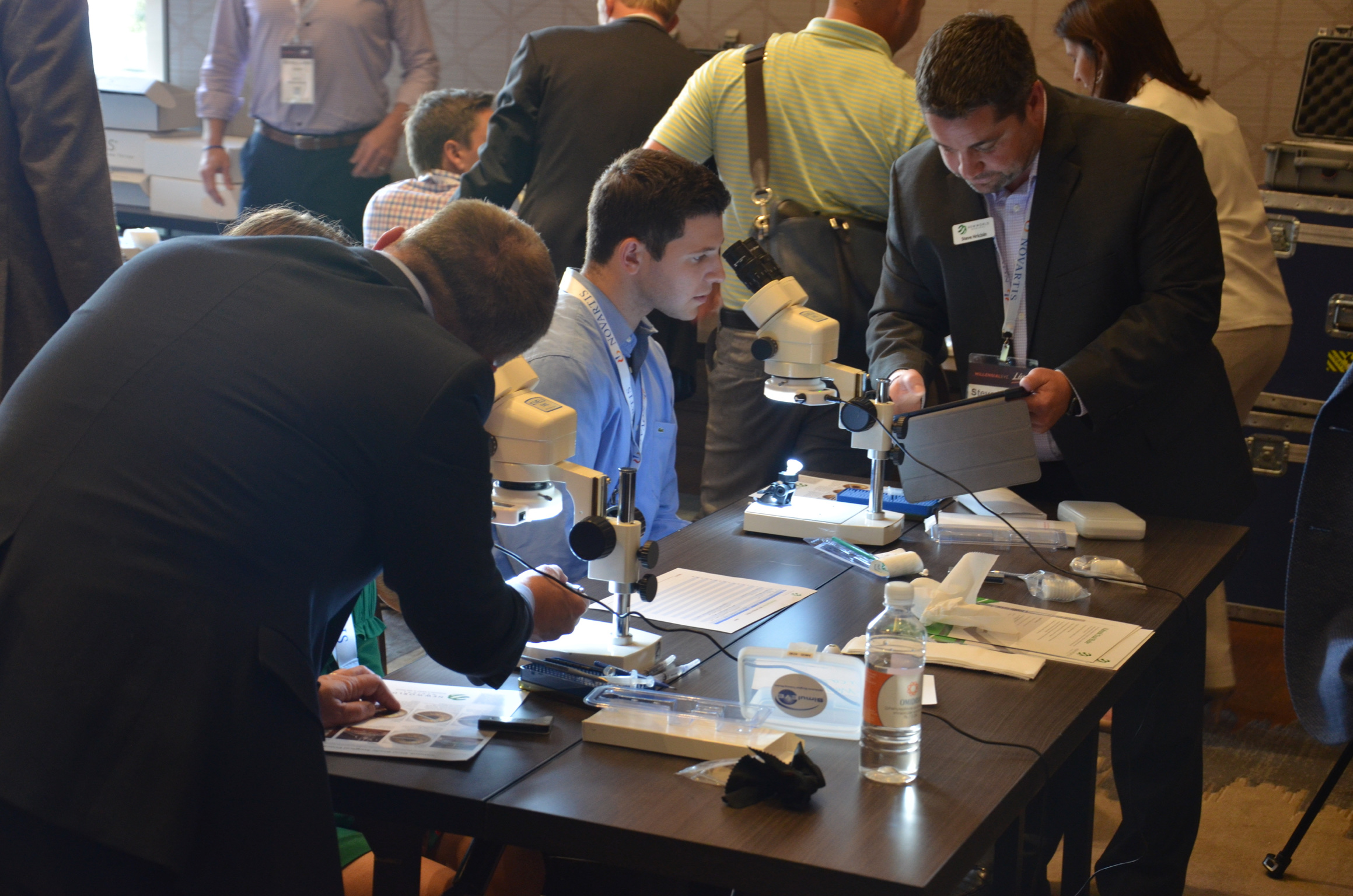
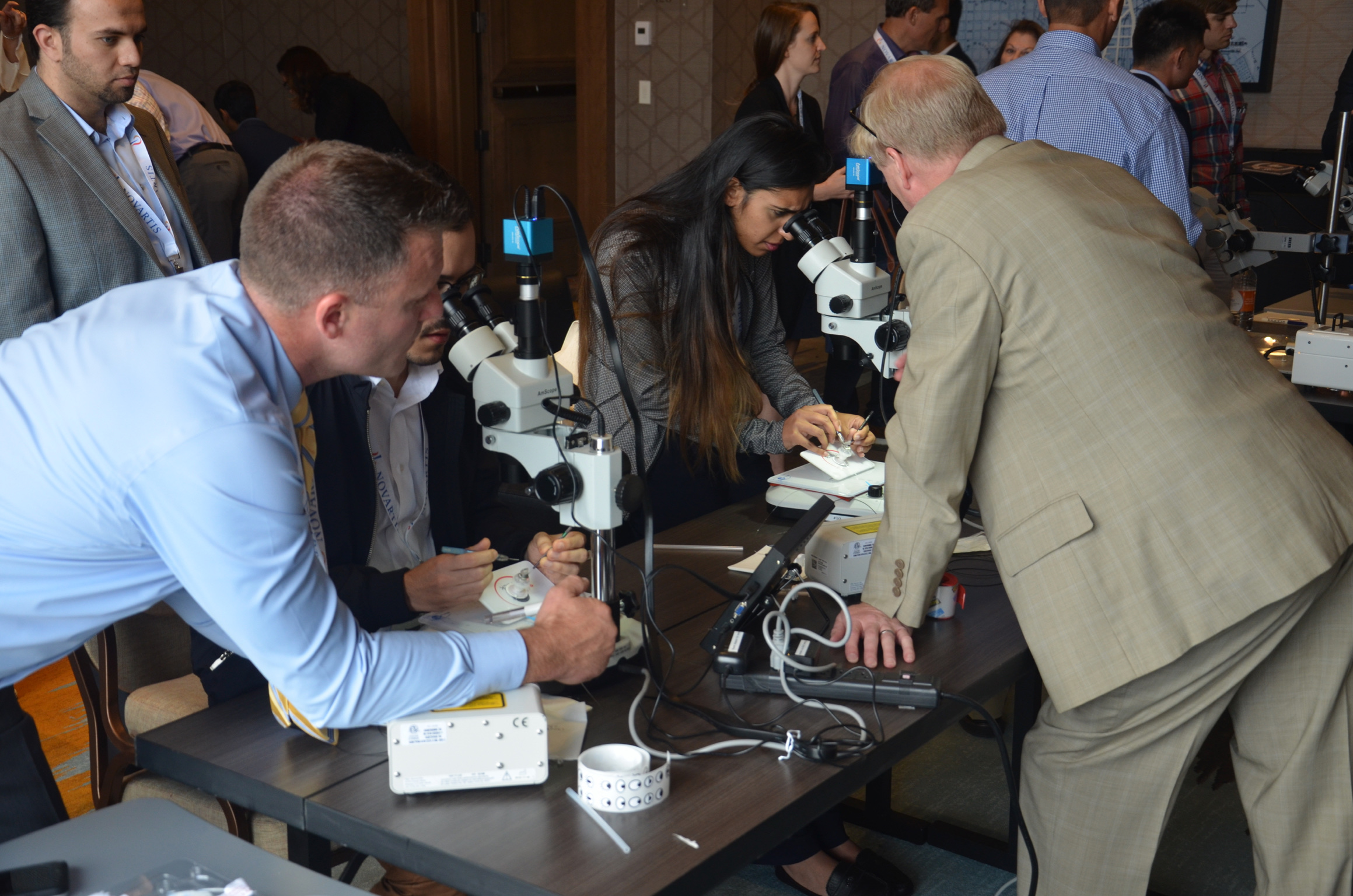
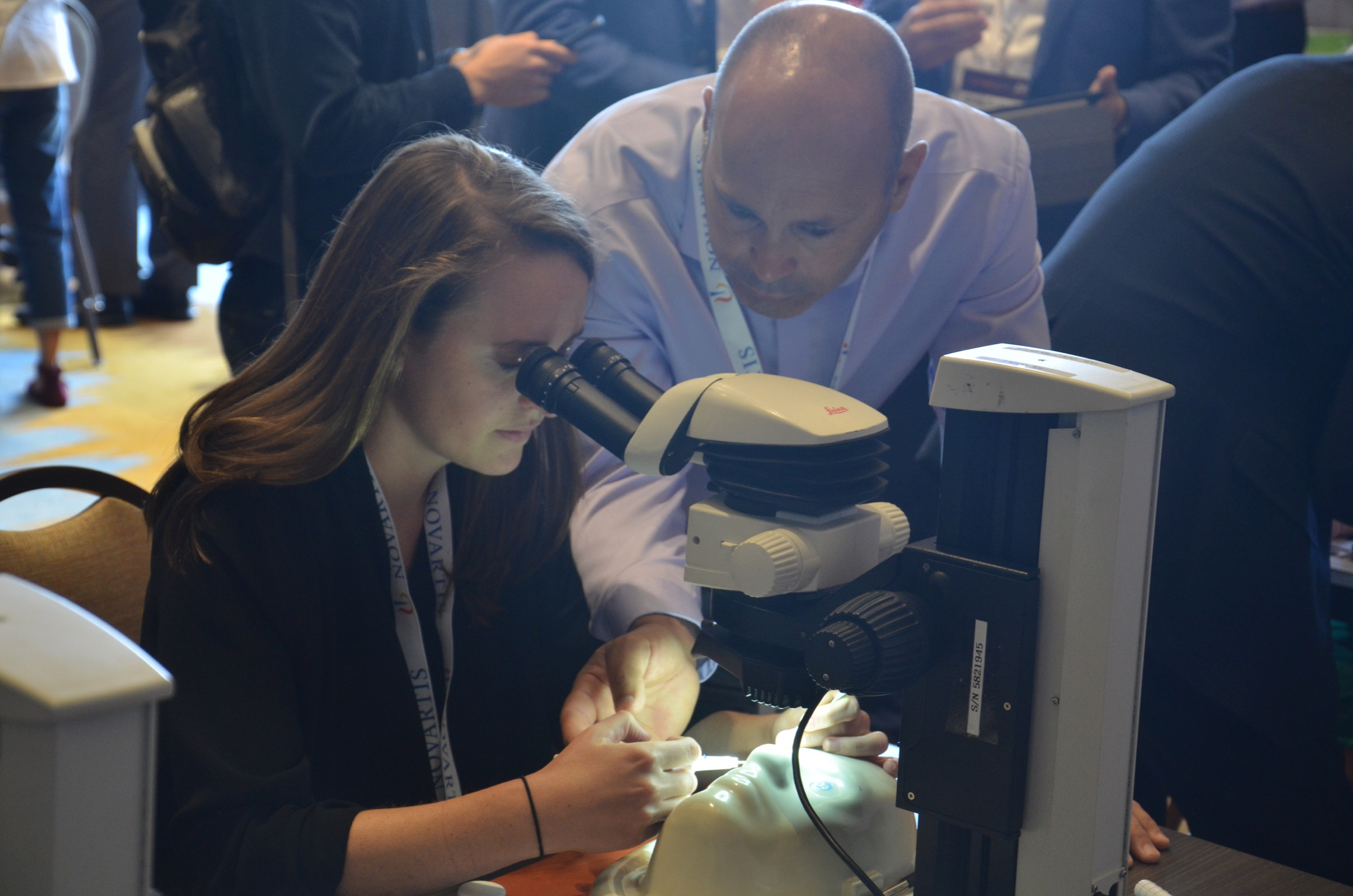
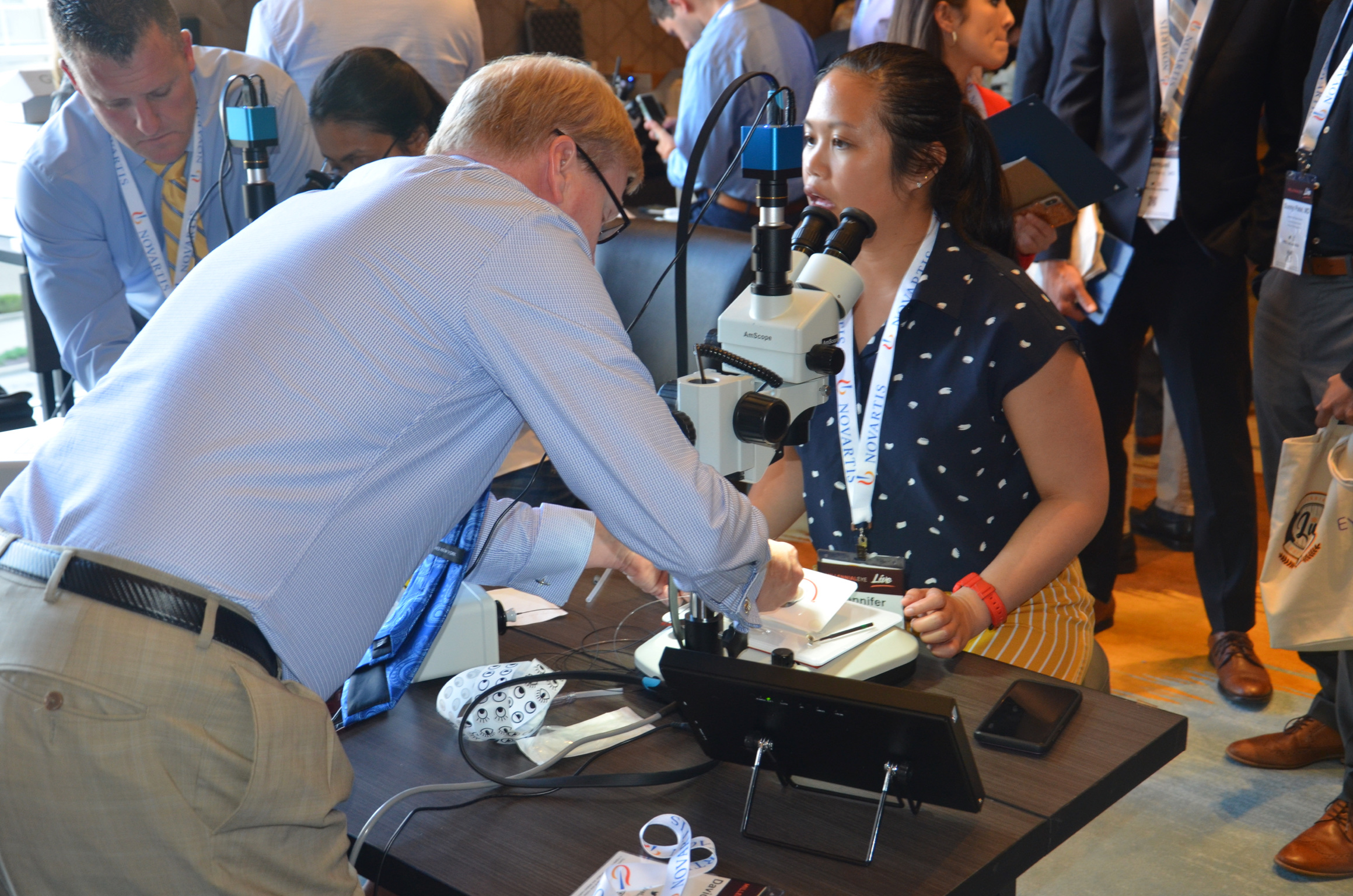
Wet Labs + Exhibits


























Top Resident/Fellow Scientific Posters
Kristen Ashourian | Pressure-Induced Interlamellar Stromal Keratitis in a Patient After DSEK Surgery
Purpose: To describe a rare case of PISK that developed after DSEK surgery in a patient with prior history of LASIK.
Methods: Case report and review of the literature
Results: We present a rare case of a patient who after DSEK surgery for bullous keratopathy developed pressure-induced stromal keratitis secondary to steroid drop therapy. Our patient experienced eye pain and progressively worsening blurry vision 5 weeks postop DSEK. Despite steroid drop therapy stromal haze continued to be non-clearing and IOP appeared normal. A fluid cleft was seen on exam and PISK was diagnosed. After stromal puncture of fluid cleft, cessation of steroid drops, and ocular antihypertensive therapy the patient experienced an improvement in visual acuity and there was less interface haze on slit lamp exam. OCT of the optic nerve showed no signs of glaucomatous damage.
Conclusions: Our case demonstrates a unique and rare complication of DSEK surgery in a patient with prior history of LASIK. Our patient developed PISK, where a rapid steroid response leads to elevated intraocular pressures driving fluid collection into a potential space. It is a devastating disease as the increased intraocular pressures are masked when the applanation is done over the soft fluid cleft, termed the “cushioning effect”. Treatment includes cessation of the steroid drops with topical IOP lowering medications. It is important to recognize the signs, the patient’s symptoms postop and recognizing true IOP in these patients in order to prevent glaucomatous vision loss.
Shehzad Batliwala | Spaceflight-Associated Neuro-Ocular Syndrome: Ophthalmology’s Role on the Final Frontier | Top 3
Purpose: Astronauts as returning from space with ocular changes consisting of hyperopic shift, cotton-wool spots, choroidal folds, optic disc edema, and posterior globe flattening with varying degrees of severity and permanence. These changes dene Spaceflight Associated Neuro-ocular syndrome (SANS), which is one of the top risks of long duration spaceflights identified by NASA. The purpose of this study was to review the literature to detail and describe the current prevailing theories regarding the pathophysiology underlying this syndrome. This information was used to assess the validity of using Idiopathic Intracranial Hypertension (IIH) as a terrestrial model for SANS.
Methods: A systematic review was conducted on literature published about the current prevailing theories of mechanisms underlying SANS etiology. This information was then applied to assess which terrestrial analogs are suitable to study SANS, and what are some effective countermeasures to mitigate changes in ocular structure and function caused by microgravity.
Results: The current prevailing theories behind SANS etiology include (1) increased intracranial hypertension, (2) increased optic nerve sheath CSF pressure causing a compartment syndrome effect, and (3) venous congestion in the brain and eye and subsequent exacerbation of choroidal volume changes. Application of lower-body negative pressure has been proposed as an effective countermeasure to mitigate choroidal venous congestion and optic disc edema seen in microgravity. Idiopathic Intracranial Hypertension (IIH) has been proposed as a suitable analog to study SANS, albeit there are key differences that must be taken into account.
Conclusions: Given the similarities between signs seen in both IIH and SANS, IIH is a suitable analog to study SANS but there are important differences unique to SANS that must be studied independently. Current literature suggests that SANS is caused not by an absolute, acute increase in ICP but rather likely results from a chronic, unrelenting, slow rise in ICP. Given the constellation of ocular signs seen in SANS, the pathophysiology is likely multi-factorial with contribution of altered hemodynamics from both blood ow and CSF. Additional investigation of these theories are required to better understand SANS and decrease the ocular disease burden of future long duration missions, such as the anticipated Mars mission.
Subhashini Chandrasekharan | Telemedicine vs. Clinical Evaluation for Glaucoma New Jersey Health Foundation Prospective Clinical Study | Top 3
Purpose: Telemedicine allows for subjects who have limited access to health care to get ophthalmic care. It was noted in the past that individuals would fail to return for a clinical examination even when told they have glaucoma. Telemedicine allows a trained person, with varying levels of experience, to capture data and images. Then, a physician would get remote access to the screened individuals’ data. The purpose is to: (1) test the technical feasibility of developing a system for telemedicine for glaucoma that will allow a physician comprehensive access to a patient’s data and images, and (2) compare teleglaucoma to traditional physical presence evaluation in a glaucoma clinic. The ultimate aim is to minimize the need for the subject to return for an appointment after a positive screening by providing care at the time of initial encounter.
Methods: Subjects, who were presenting at University Hospital glaucoma clinic, were enrolled on the same day into the teleglaucoma screening program. Upon informed consent, the subjects went through several stations, which included personal/family health history, auto-tonometer for noncontact measurement of IOP, auto-refractor, and OCT (Optovue) of the anterior segment, optic nerve and posterior pole (corneal thickness, angle anatomy, cup-to-disc ratio, retinal nerve fiber layer, and ganglion cell complex data were collected). At the last station, nonmydriatic retinal camera (Canon CR2) was used to acquire anterior segment, fundus and auto fluorescence images. Collected data and images were analyzed by a physician who provided diagnostic and therapeutic recommendations. The subjects were also examined on the same day in glaucoma clinic. The data collected from teleglaucoma and physical presence were compared for accuracy using means and Pearson Correlation coefficient. The accuracy of glaucoma diagnosis and therapeutic recommendations were also compared. Limitations on adequate ocular examination or imaging during teleglaucoma were recorded.
Results: In total, 107 subjects were enrolled (mean age of 61 ±15 years, 61% females, 51% African American, 38% Hispanic, 7% Indian, and 4% Caucasian). A strong positive Pearson Correlation was seen for IOP of OD (right eye) and OS (left eye), optic nerve cup-to-disc (C/D) ratio OD, OS and diagnosis (no glaucoma, glaucoma suspect or glaucoma diagnosis). There was a moderate positive Pearson Correlation for treatment plan/return to clinic time (RTC), with an average shorter RTC in teleglaucoma of 2.7 months compared to clinic examination, 3.9 months. There was a shorter RTC in 49% of the subjects in teleglaucoma. Teleglaucoma was more likely to elicit a non-glaucoma diagnosis not found in the clinic vs a diagnosis found only in clinic (18% of subjects vs 5%). One trained person was able to complete the entirety of the teleglaucoma evaluation in an average of 24 mins.
Conclusions: In certain cases, OCT analysis was possible when non-mydriatic retinal imaging was precluded by media opacities. Both OCT analysis* and physician analysis of retinal images provided C/D ratios in 82% of the eyes. Average grade (range: 1 [worst] to 5 [best[) of the retinal images were 3.5. 7% of the images received a grade of 1 as the images were unreadable. In 50% of the subjects with an unreadable image, OCT was able to capture data and C/D ratios. Additionally, the OCT was able to provide anterior chamber angles (Average: 31°OU (both eyes); 94% of eyes) and central corneal thickness (Average: 498; 93% of eyes). Corneal thickness was thinner than average. Teleglaucoma was not able to pick up anterior segment pathology as well as physical exam (Trabeculectomy, Peripheral Iridotomy). In addition, in 6.5% of the eyes, Tele-glaucoma was not able to capture C/D ratios when clinic exam was possible. *C/D ratio was only attempted on the OCT in 67 subjects.
Joshua Frenkel | Virtual Reality Goggles: A Novel Method for Visual Field Perimetry | Top 3
Purpose: To report the development and preliminary evaluation of a portable, inexpensive automated perimetry system that utilizes affordable, commercially available VR hardware (Oculus Rift DK2) and easily extensible software developed in a cross- platform framework.
Methods: We developed an algorithm that utilizes a binary search algorithm for thresholding of stimulus intensity and presents stimuli in regions known to be associated with glaucomatous change in a pseudo-random manner. To accomplish this, we utilize a graphic client developed using the Unity graphics engine communicating asynchronously with a python backend for experimental visualization and control. This was then deployed into the commercially available VR hardware (Oculus Rift DK2).
A cross-sectional study including 23 patients (28 eyes) with glaucoma and eight healthy controls (16 eyes) recruited at Tulane University. All subjects underwent Oculus Rift testing and the results were compared to same-day testing using standard Humphrey Field Analyzer (HFA II), with the order of testing randomized. A standardized survey was also administered soon after both tests were performed questioning the patient in regard to the ease of use of the two devices. Glaucoma patients were categorized as mild, moderate and advanced based on the HVF changes. An experienced examiner analyzed each virtual reality test output as normal or mild, moderate or advanced glaucomatous change. This data was then compared to the HVF changes to generate sensitivity and specificity.
Results: Sensitivity of our visual testing in detecting glaucomatous changes was 82.1% and specificity was 87.5%. 92% of the users preferred the portable device both for ease of use and comfort as opposed to the HVF. Results from the portable device agreed with the HVF data in 100% of the healthy patients and cases with moderate to severe glaucoma visual field changes but failed to detect those with early paracentral scotoma.
Conclusions: Clinical results indicate that our newly developed portable visual field testing system using commercially available Oculus Rift goggles is sufficiently accurate to serve as a glaucoma screening tool. Improving the algorithm and performing subsequent point-by-point comparison between future results is necessary to prove our system’s diagnostic test potential. Our system has advantages over conventional methods, as it is portable and inexpensive.
Anita Goyal | The Use and Viability of Two Autologous Grafts as Anterior and Posterior Lamellar Spacers in Eyelid Reconstruction
Purpose: The viability of two separate autologous grafts as anterior and posterior lamellar spacers in eyelid reconstruction remains unverified. We performed a retrospective, observational study to test the efficacy of dual autologous grafting in reconstruction of moderate eyelid defects resulting from basal cell carcinoma resection.
Methods: In the study, six eyelids of six patients (three men, three women; mean 76 years old, range 68-85) underwent simultaneous anterior and posterior lamellar reconstruction following extensive basal cell tumor resection (mean resection diameter 2.1 cm) between 2014 and 2017. The anterior lamella was reconstructed with the use of skin from the contralateral eyelid, while the posterior lamella was reconstructed from the hard palate. The study consisted of reconstructions of one left upper eyelid, one right upper eyelid, and four right lower eyelids. Outcomes measured over 36 months included post-operative eyelid mobility and stability, surgical site complications, and lack of contracture and rejection.
Results: All patients in this study had complete viability of both anterior and posterior lamellar grafts following reconstruction. Significant eyelid mobility was recovered postoperatively. Restoration of the original eyelid structure and stabilization of the eyelid margin was attained, creating a natural cosmetic appearance. Contraction and graft rejection were not encountered. Ectropion was not encountered. Keratinization, common to autologous skin grafts, did not occur.
Conclusions: Eyelid reconstruction with the use of two separate autologous grafts as anterior and posterior lamellar spacers can be achieved with complete viability of both grafts. The use of autologous grafts avoids the need to use expensive non-autologous grafts with the possibility of rejection. The use of two autologous grafts creates a natural cosmetic appearance that is dicult to obtain with individual synthetic grafts. Viability of both grafts may be attributed to the dual blood supply to the eyelid formed by the ophthalmic and lacrimal arteries.
Katelyn Joubert | Clinical Outcomes of Descemet Membrane Endothelial Keratoplasty in Super-Seniors | Top Cornea (Supported by Azura Ophthalmics)
Purpose: To evaluate the clinical outcomes of Descemet membrane endothelial keratoplasty (DMEK) performed in the “oldest old” patients, ie, ≥90 years.
Methods: Between 2009 and 2019, 20 consecutive eyes of 17 patients aged ≥90 underwent DMEK for endothelial dysfunction. Best corrected visual acuity (BCVA), central corneal thickness (CCT), endothelial cell density (ECD), graft survival, and intra- and postoperative complications were assessed.
Results: Except in one case in which the DMEK surgery could not be completed, all operated eyes experienced an improvement in BCVA, although only 50% achieved 20/40 (0.5) by 1 year postoperatively. One year after surgery, median CCT had declined from 641 (±161) μm to 480 (±34) μm, and median endothelial cell density was reduced by 53%, from 2574 (±286) to 1226 (±404) cells/mm2. Six of 19 eyes receiving DMEK grafts (32%) developed partial graft detachments requiring re-bubbling. One eye experienced a secondary graft failure at 6 months and underwent repeat endothelial keratoplasty.
Malcolm Kates | Antifungal Efficacy of Betadine in Optisol GS Corneal Storage Media
Purpose: To compare the antifungal efficacy of multiple concentrations of Betadine in Optisol-GS
Methods: Eighteen donor corneas were donated by Lions Eye Institute for research. A suspension of Candida Albicans was prepared to 0.25 on the McFarland scale of turbidity (using DensiCHEK optical densitometer) in the UF Microbiology lab. All corneas were sequentially bathed in the suspension of Candida. Two corneas were placed in Optisol GS without betadine and four corneas each were placed in solutions containing 1%, 0.75%, 0.5%, and 0.25% betadine. After 5 minutes of thermal equilibration time the corneas were removed from their individual storage solutions under sterile technique, swabbed with a 10 uL inoculation loop, and streaked onto Sabouraud agar plates. Corneas were placed back into their storage medias and placed in a monitored refrigerator at 4oC. The Sabouraud plates incubated at 37oC for 48 hours, at which time viable colony counts were measured and photo-documented. The corneas remained refrigerated and were then re-plated on days 2, 4, 6, 8, 10, 12, and 14. The Sabouraud plates were assessed on days 2, 4, 6, 8, 10, 12, 14, 16, 18, 20 for growth. The same individual counted all plates.
Results: Betadine 1% & 0.75% demonstrated a significant decrease in Candida growth compared to control early in the study that persisted. Betadine 0.50% demonstrated a significant decrease in Candida growth compared to control but not until plated day 10. Betadine 0.25% was not effective.
Peter Lam | Outcomes of Resident-Performed Combined Cataract Surgery and MIGS at 1-Year Follow-Up
Purpose: To evaluate the efficacy and safety of resident-performed combined cataract surgery and MIGS
Methods: A retrospective chart review was done at a single site, which was a large state hospital in Louisiana. Chart review of 130 patients with inclusion of 122 eyes from July 2015 to March 2019. Inclusion criteria included any patients with primary open angle glaucoma or narrow angle glaucoma who underwent combined cataract surgery with either iStent or Kahook Dual Blade. Exclusion criteria included previous ocular surgeries and prior intravitreal injections. Patients who required additional glaucoma surgeries for poorly controlled intraocular pressure after combined cataract surgery and MIGS were also excluded if the surgery was done before 1-year follow-up. Patients who had complications during cataract surgery that prevented the MIGS procedure were also excluded. Main outcome measures were mean postoperative IOP at 1 year follow-up and mean number of IOP-lowering eye drops at 1 year follow-up. The data was analyzed using GraphPad (Prism 8.1.2, La Jolla, CA). T-test was used with statistically significance defined as P <0.05.
Results: The mean preoperative IOP was 16.4 ±3.68 mm Hg. The mean postoperative IOP at 1 year was 14.5 ±3.37 mm Hg. This was a 12% decrease in IOP at 1 year (P < .01) Mean baseline preoperative number of drops were 1.19 ±0.915. Mean number of postoperative drops were 0.958 ± 1.02. This was a 19.5% decrease in number of IOP-lowering drops at 1 year (P < .065). 86% of eyes had IOP of 18 mm Hg or lower. Most common complications were hyphema, corneal edema, and rebound iritis, which resolved by 3 months.
Joseph Ling | Investigating Clinical Outcomes of Selective Laser Trabeculoplasty After Failed First-Generation Trabecular Microbypass Stent in Glaucoma
Purpose: To evaluate the clinical outcome of selective laser trabeculoplasty (SLT) after failed trabecular microbypass stent (model G1)
Methods: Records of 22 eyes of 14 patients who underwent SLT after failed iStent surgery were retrospectively reviewed. 17 patients who underwent primary SLT without history of iStent were reviewed as age-matched controls.
Results: Patients were determined to have failed iStent surgery after having a mean IOP rise of 10% at 24 months and were treated with SLT. Mean reduction in the IOP after SLT was similar in the failed iStent group vs. primary SLT group at 3 months (24% vs. 27%) and 6 months (23% vs. 26%). At follow-up (6 months) the IOP was significantly reduced from baseline in both groups (iStent P < .01 and primary SLT (P < .0001).
Brett Mueller | Comparing Clinical Outcomes of Two Microinvasive Glaucoma Surgical Procedures: iStent vs. CyPass
Purpose: To determine the efficacy and safety profile of the iStent and CyPass implantation by a single center teaching institution.
Methods: A retrospective chart review was performed on 62 patients for a total of 73 eyes who received either an iStent (35 eyes) or a CyPass (38 eyes) implanted at the time of cataract extraction at the Robley Rex VA Medical Center in Louisville, Kentucky, from July 1, 2014 to March 28, 2018. The primary outcome was reduction of IOP. The secondary outcomes were the reduction in the number of glaucoma medications and intraoperative and postoperative complications.
Results: In the iStent cohort, mean IOP decreased from 19.28 mm Hg ±5.42 preoperatively to 15.34 mm Hg ±3.65 (P < .001) at 1 month, 15.69 mm Hg ±4.57 (P < .001) at 6 months, and 16.6 mm Hg ± 3.65 (P = .003) at 12 months postoperatively. The mean number of glaucoma medications used decreased from 1.29 ±0.98 preoperatively to 1.14 ±1.2 (P = .298) at 6 months and 1.2 ±1.21 (P = .373) at 12 months postoperatively. Intraoperative complications included failure of placement of the iStent in four eyes due to poor visualization from bleeding or technical error. No major postoperative complications occurred.
In the CyPass cohort, IOP decreased from the average preoperative IOP, 19.1 mm Hg to 13.0 mmHg (P < .001) at 1 month and 15.13 mm Hg at 6 months postoperatively (P < .001). The average number of IOP lowering drops also decreased from 1.6 to 0.23 drops (P < .001) and 90% of the operative eyes did not need to be started back on their IOP lowering drops. Three patients suffered an intra-operative hyphema from the placement of the CyPass and two patients could not have the CyPass placed into the suprachoroidal space. Postoperative complications occurred in 16% of patients with 11% of patients having recurrent inflammation requiring either a sub-tenons Kenalog injection and/or prolonged treatment with Durezol.
Conclusions: The iStent trabecular microbypass implant resulted in a significant reduction of mean intraocular pressure at all follow-up intervals through 12 months but did not significantly reduce medication burden. Therefore, iStent implantation may be a successful adjunct to drop use in patients with mild to moderate primary open-angle glaucoma. In addition, the side effect profile of the iStent was very low.
The data obtained from the CyPass cohort demonstrated that canalizing the suprachoroidal space was a viable surgical option for decreasing IOP and dependence on IOP-lowering drops in patients with open angle glaucoma. However, this surgical device had a considerable postoperative complication prole that should be considered for each patient getting this procedure. This device has recently been removed from the market because of decreasing endothelial cell count. This study did not demonstrate this side effect profile, but it is something that should be considered when implanting a device in the suprachoroidal space. As new MIGS devices are being developed, it is important to consider their surgical efficacy and safety. Further studies are needed to investigate the long-term effects of placing a trabecular meshwork or suprachoroidal stent in patients to lower IOP and slow the progression of glaucoma.
Sabrina Mukhtar | The Novel Application of Optical Coherence Tomography as an Intraoperative Adjunct for Oculoplastic Surgery
Purpose: To demonstrate the novel use of intraoperative optical coherence tomography (iOCT) as an adjunct in Oculoplastic surgical procedures to improve intraoperative surgical decision making in patients with challenging tissue planes.
Methods: A microscope integrated iOCT system, RESCAN 700, was utilized throughout the operative procedure of three patients, one with obliterative conjunctival disease and two patients with congenital ptosis, where en face delineation of tissue was dicult, to provide real-time non-invasive imaging feedback.
Results: In the case of obliterative conjunctival disease, iOCT was used to correctly identify and differentiate scar tissue from conjunctival and corneal tissue, which aided in safer resection without causing structural damage. Similarly, in a pediatric patient with congenital ptosis and history of previous surgeries, iOCT correctly identified levator tissue and aided with appropriate scar tissue resection for proper placement of mersilene sutures. Lastly, iOCT allowed for placement of the frontalis sling in the correct tissue plane in a second case of congenital ptosis. No postoperative complications related to the imaging modality were observed.
Craig Thiessen | A Comparison of Postoperative Management in Resident Cataract Cases: Dropless vs. Traditional Regimen
Purpose: To compare postoperative efficacy of a dropless regimen to that of a traditional topical regimen in resident cataract cases.
Methods: This retrospective study used data from a single electronic medical record to compare the control group, topical antibiotics and steroids, and the study group, intracameral Vigamox and Kenalog or subconjunctival Kenalog. Visual outcomes, intraocular pressure, rebound inflammation, corneal edema, and endophthalmitis were the primary measured outcomes. Intraocular complications were also measured between the two groups including torn capsules, secondary sulcus lens placement, and cystoid macular edema. All statistical measures were completed using SPSS Statistics.
Results: 89 eyes were included in this study, 42 in the control group and 19 in the dropless group. The preoperative vision was 20/400 in the control group and 20/160 in the dropless group. Postoperative visual outcomes were not statistically different in each group at each postoperative visit. There was a statistically (P = .002) higher rate of rebound inflammation in the dropless group, which required additional topical steroids in 10 (53%) patients. Only one (2%) topical regimen patient was diagnosed with rebound inflammation. There were zero cases of increased intraocular pressure or endophthalmitis between either group. Corneal edema was also not statistically different at any postoperative visit.
Surgical complications included 6 (9.8%) torn capsules and 3 (4.9%) cases of cystoid macular edema (CME). Four capsular tears occurred in the control group and two in the dropless, requiring three sulcus lenses to be placed. Of note, all torn capsules were in hand-motion cataracts or worse. CME occurred in two (10%) of the dropless patients, one of which also had a capsular rupture.
Thanks to all who contributed to the 2019 ME Live scientific poster submissions!
Sameer Al-Shweiki | Kristen Ashourian | Samuel Barry | Shehzad Batliwala | Siddharth Bhargava | Judd Cahoon | Maria Castanos | Carlos Salgado Cerrate | Subhashini Chandrasekaran | Naja Chisty | Nitin Chopra | David Felsted | Erin E. Flynn | Joshua Frenkel | Zafar Gill | Jason Goldberg | Anita Goyal | Valentina Gracia | Daniel Henick | Lena Hummel | Arjan Hura | Adam Jacobson | Katelyn Joubert | Malcolm Kates | Mahmood Khan | Brent Kramer | Marharyta Labkovich | Peter Lam | Joseph Ling | Danny Mammo | Charles McGuffey | Huan Mills | Abhiniti Mittal | Brett Mueller | Sabrina Mukhtar | Jeb Ong | Sunny Patel | Ruju Rai | Devasis Reddy | Jorge Andrade Romo | Eric Rosenberg | Mohammad Ali Sadiq | Ayesha Shariff | Barbara Smith | Casey Smith | Subhan Tabba | Craig Thiessen | Lillian To | Nandini Venkateswaran | Jijo Wang | Caroline Watson | Logan Vander Woude | Melissa Yuan | Davis Zhou


