Phacoemulsification is a crucial procedure to learn during ophthalmology residency, and it is considered a central element of ophthalmic education. Despite the development of various guidelines and syllabi, residents’ real-world educational experiences vary, and many factors affect the learning process. Although it is difficult to generalize the process of learning phacoemulsification for all ophthalmology residents across teaching programs worldwide, this article presents pearls gleaned from my experience performing 100 cases in the first 3 years of my ophthalmology residency.
Did you know?
Eyetube has a dedicated cataract channel that features thousands of surgeon-submitted surgical videos.
Step 1: Study the Fundamentals and Watch Videos
The first step to learning the basics of phacoemulsification can be taken at home by reading about and watching videos of the procedure. Rather than study the nuances, it is advisable at this point to focus on the general concepts: the fundamentals of the different phaco machines, the uses of the required materials and instruments, the anesthesia settings, and the steps of phaco surgery and their importance.
Watching videos of phacoemulsification is a valuable exercise. Some of my favorite resources include the following:
- Cataract Coach by Uday Devgan, MD (my top choice)
- University of Iowa’s Eye Rounds
- University of Utah’s Moran CORE
- Eyetube
- Eye Guru
Step 2: Build Manual Dexterity
All surgeons in training must practice bimanual coordination, minimize tremor, and develop spatial awareness of their hands. These goals can be achieved, to a certain degree, before starting to work under a microscope. Manual dexterity can be honed while practicing suturing in a wet lab, placing sutures for trauma patients in an emergency department, and even when simply eating with a knife and fork.
At the same time, it is important for new phaco surgeons to practice skills under the microscope in a wet lab or OR after surgery when possible. This can help to build their confidence with handling a microscope, including how to gain optimal focus, control pedals with different functions, and become familiar with the surgical view.
After completing these tasks, the surgeon can begin to practice simple extraocular surgeries, including adnexal benign mass removal, corneal sutureremoval, and pterygium excision, under the microscope. Practicing these operations can reduce the trainee’s awe of intraocular surgery. Surgical videos can also be helpful for studying and improving manual dexterity.
Step 3: Start With the More Basic Phaco Steps
The phaco procedure is typically divided into steps, from draping and speculum insertion to phacoemulsification itself. Many ophthalmologists agree that creating the capsulorhexis and dividing the nucleus are the most difficult phaco steps to perform, so it may be helpful to try to master intraocular manipulation through other steps beforehand.1 I worked on different steps in tens of cases before proceeding to my first full phaco case under direct supervision.
Surgeons in training should know when to stop operating and consult a supervisor. Complications may occur during a trainee’s initial phaco cases, so it is important to be familiar with the challenges that typically present during phacoemulsification. The best way to do this is by watching videos and learning from others’ mistakes. The most important complications to recognize include a run-out capsulorhexis, radial tears in the capsulorhexis margin that travel toward the lens equator, and posterior capsular rupture. Some signs of posterior capsular rupture include shallowing of the anterior chamber, an iris snip, and vitreous prolapse. Recognizing such signs as early as possible will enable better handling of complications.
The use of general anesthesia, sedation, or at least local anesthesia can promote a more comfortable and less stressful teaching and learning environment, especially in the early cases.
Videos are an important resource during this phase of training as well. The quality and quantity of information gained from these videos will change once the surgeon starts actually performing the steps of phacoemulsification; the knowledge gained from watching surgical footage is augmented by hands-on experience.
Step 4: Perform a Full Phaco Procedure
Before performing a full phaco case, it is essential to master intraocular instrument handling and to be aware of common complications and strategies for their management. Surgeons should choose their initial cases wisely and consider the use of general anesthesia, sedation, or at least local anesthesia.
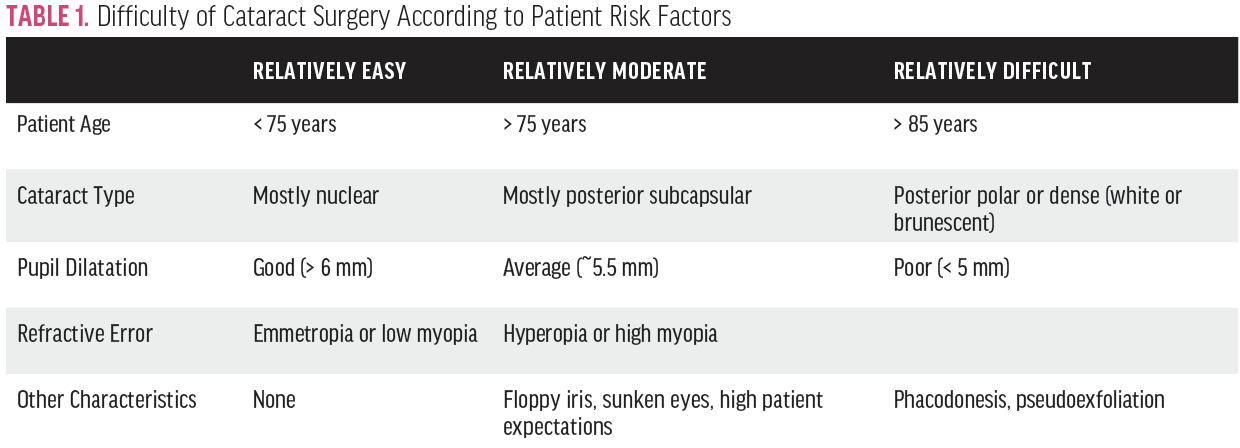
According to the literature and in the experience at our institution,2,3 cataract cases typically can be categorized by relative difficulty as easy, moderate, and difficult (Table 1). Those who are just starting out should begin with relatively easy cases and recognize that not every step can be mastered at once. For example, it usually takes longer to master nuclear disassembly than other steps. Another important point is preoperative patient counseling. Some patients may refuse to have residents perform their surgeries; assuring them that senior consultants will be available throughout the procedure may be a good initial step in their counseling.
Again, videos can demonstrate how complications occur and present tips for their management and prevention.
Step 5: Learn to Manage Difficult Cases and Complications
The average complication rate reported for resident-performed phaco surgery varies, with an average of around 17.5%.4 Complication rates are higher for more senior residents, probably owing to the increased difficulty of the cases they perform. Step by step, complication rates are highest for the creation of the capsulorhexis.
After confidently completing relatively easy cataract surgeries, surgeons in training must learn more advanced skills for performing complex cataract procedures and handling complications. If necessary, trainees can ask a supervisor to provide education on the following:
- Different techniques for lens division;
- Management of an overly small and run-out capsulorhexes;
- Management of a ruptured posterior capsule;
- Insertion of a three-piece IOL in the sulcus; and
- Placement of iris-dilating devices.
After independently performing the steps of phacoemulsification and learning the skills to manage difficult cases and complicated situations, surgeons in training can identify the next milestones to reach. These may include performing moderately difficult cataract surgery and operating under topical anesthesia. Figure 1 shows the learning curve that I experienced when following the aforementioned steps.
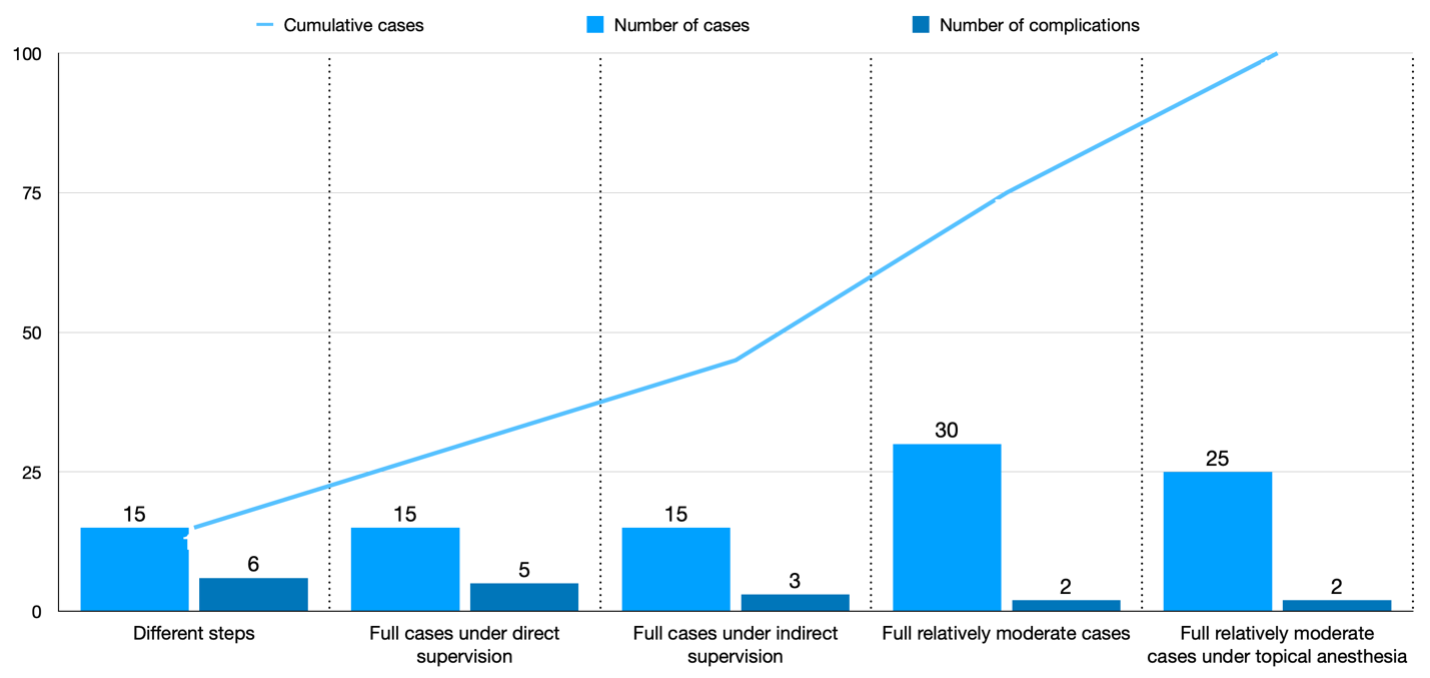
Figure 1. The learning curve from performing scattered phaco surgery steps to independently performing a moderately difficult case under topical anesthesia, based on Dr. AlRyalat’s experience.
1. Kaplowitz K, Yazdanie M, Abazari A. A review of teaching methods and outcomes of resident phacoemulsification. Surv Ophthalmol. 2018;63(2):257-267.
2. Muhtaseb M, Kalhoro A, Ionides A. A system for preoperative stratification of cataract patients according to risk of intraoperative complications: a prospective analysis of 1441 cases. Br J Ophthalmol. 2004;88(10):1242-1246.
3. Weingessel B, Wahl M, Huf W, Vécsei‐Marlovits PV. Decision‐making for cataract surgery: changes within 7 years. Acta Ophthalmologica. 2019;97(1):e139-e140.
4. Al-Jindan M, Almarshood A, Yassin SA, et al. Assessment of learning curve in phacoemulsification surgery among the Eastern Province ophthalmology program residents. Clin Ophthalmol. 2020;14:113.