CASE PRESENTATION
A 33-year-old man presents with an interest in laser vision correction. The patient is a mixed martial arts (MMA) fighter. He has a manifest refraction of -3.00 +1.00 x 038º OD and -2.50 +0.50 x 130º OS. After a discussion of PRK and LASIK as surgical options, he chooses to undergo LASIK. The procedure is performed without incident. One month after surgery, his UCVA is 20/15 OU, and he is happy with his result. He has agreed to avoid contact fighting for a total of 6 months postoperatively but has resumed his routine workouts while wearing appropriate eye protection.
Six weeks after surgery, the patient returns. He is wearing a contact lens on the left eye only and reports severe pain in that eye. He reports being hit by a car while riding his motorcycle. He sustained multiple traumas, including a fractured liver, ruptured spleen, broken left fibula, fractured tibia, and flail chest on the left side. He spent the past 3 weeks in the intensive care unit at a level 1 trauma center and reports undergoing ocular surgery on the left eye only in addition to the trauma-related interventions. The patient says that the intensive care unit’s discharge nurse told him that, while he was under anesthesia for the other interventions, the ophthalmic team refloated the LASIK flap in his left eye. He does not remember seeing anyone on the ophthalmology team.
The patient’s UCVA is 20/15 OD, and an ophthalmic examination reveals a normal cornea status post-LASIK in this eye. His UCVA is 20/125 OS, and pinhole visual acuity is 20/40. A 6 x 7-mm defect with ulcerated edges and a severe keratitis involving the LASIK flap are evident (Figure 1).
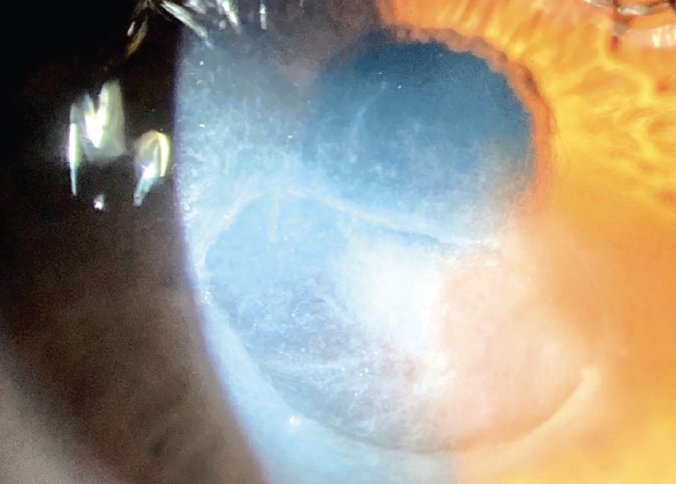
Figure 1. The appearance of the left eye 3 weeks after the LASIK flap was initially refloated.
How would you proceed? What medications would you prescribe? What cultures, if any, would you obtain? Do you routinely perform PRK or LASIK on patients with a history of contact sports?
Case prepared by Karl G. Stonecipher, MD; Monica Soni; and Ben Likins, MS

DEREK W. DELMONTE, MD
Counseling refractive surgery candidates on their options, including the relative advantages and disadvantages of LASIK and PRK, is not as straightforward as it used to be. With the introduction and continued improvement of femtosecond laser technology, the risks associated with creating a LASIK flap have decreased, as has the risk of postoperative traumatic flap dislocation. I explain to patients that direct trauma to the eye—even years after surgery—can lead to flap-related complications but that the risk of dislocation is exceedingly low and it no longer prevents me from recommending LASIK to professional athletes and others who are at increased risk of eye trauma. I think this case illustrates that the amount of trauma required to disrupt or dislocate a LASIK flap is associated with a high level of morbidity regardless of whether there is a history of ocular surgery.
Because presumed infectious keratitis was noted during this patient’s hospitalization for significant roadside trauma, culturing for a wide variety of organisms would be prudent. The initial trauma and the subsequent hospitalization and manipulation of the eye are risk factors for atypical infection. Using specific culture media for both mycobacteria (such as Lowenstein-Jensen medium) and fungus (Sabouraud agar) in addition to the standard blood and chocolate agars for aerobic and anaerobic bacteria could be helpful. Culturing a foreign body—this patient’s contact lens would qualify—at the time of presentation could also increase the likelihood of a positive culture.
LASIK flaps present a unique challenge in cases of infectious keratitis because they can harbor infectious organisms in a relatively protected environment, out of reach of culture or treatment. It is not necessary to lift, manipulate, or amputate the flap in most situations. It may, however, be necessary in the setting of advanced or atypical infection (such as in this case) or when the flap is damaged or melting to help identify the infectious organism and facilitate treatment with topical medications. If a LASIK flap is amputated, the tissue should be divided and cultured on media whenever possible.
When initiating topical therapy for extensive or visually significant keratitis, I like to begin with broad-spectrum antibiotics such as vancomycin (25 mg/mL) and tobramycin (14 mg/mL) and make adjustments based on culture results when available. I prefer not to start with topical antifungals or antiparasitic medications until a positive culture result is obtained in order to avoid unnecessary and prolonged treatment with toxic medications that may delay healing.

PREEYA K. GUPTA, MD
Choosing between LASIK and PRK can be difficult when a patient is a candidate for both procedures. Patients often elect to undergo LASIK because visual recovery is faster after this procedure. My preference for an MMA fighter, however, would be PRK because this person is at increased risk of contact-related trauma.
It is not surprising that a catastrophic motor vehicle accident (MVA) traumatized the LASIK flap and resulted in infectious keratitis. I would initiate aggressive therapy with topical antibiotics and culture the flap for pathogens, including bacterial (aerobic and anaerobic), fungal, saprophytic, and other environmental opportunistic pathogens such as mycobacterium.
An infected LASIK flap can also be managed with amputation, which can help to isolate the pathogenic species (through culturing of the flap), debulk the infection, and increase the penetration of antiinfective medications. Fungal keratitis can take weeks to months to resolve. The penetration of medications used to treat fungal keratitis is poor if the epithelium is intact; epithelial debridement can be performed to assist drug penetration.
In situations similar to the one presented, I typically prescribe hourly topical drops such as natamycin or amphotericin B, depending on the species identified on the culture, and slowly taper the medication as the clinical response improves. Oral agents can be used as an adjunct. It is worth emphasizing the fine balance between treatment with antiinfectives and the prevention of scar formation from a prolonged epithelial defect. The long-term use of topical medication can impede and draw out epithelial recovery.

KEITH A. WALTER, MD
This case presents an exceedingly rare but incredibly unfortunate event after LASIK. It is ironic that an MVA rather than an MMA fight dislocated the LASIK flap. This may suggest that severe trauma is required to dislocate a LASIK flap created with a femtosecond laser. I know this patient promised not to engage in MMA activities, but I doubt he adhered to that promise for fear of becoming less physically fit. My point is that I think it is totally appropriate to offer LASIK to patients like this one. The delayed healing, pain, and prolonged visual recovery associated with PRK can be a burden on patients and surgeons. Since I have started using a femtosecond laser to create LASIK flaps, I have yet to see a traumatic dislocation or even a slipped flap. I suspect that the vertical edge of a laser flap and the manhole cover–like geometry account for the reduced slippage. Even with severe trauma, a laser flap holds up well in most cases.1
It is possible that severe trauma from the MVA would have ruptured the globe if this patient had undergone PRK. In theory, the LASIK flap could have absorbed the traumatic forces, resulting in a dislocation but not a full-thickness laceration or ruptured globe.
His severe life-threatening injuries obviously warranted more attention, but the patient’s eye injury was treated appropriately at the time. That said, his current presentation appears to be infectious and/or neurotrophic. The infiltrate does not have the typical appearance of a bacterial ulcer, so cultures for atypical organisms are warranted.



WHAT WE DID: KARL G. STONECIPHER, MD; MONICA SONI; AND BEN LIKINS, MS
The patient’s contact lens was immediately removed and sent for polymerase chain reaction and culture. The culture of the eye was promptly carried to the hospital. In the clinic, the patient was started on hourly besifloxacin ophthalmic solution 1.5% (Besivance, Bausch + Lomb) and gentamicin eye drops alternating every 30 minutes. Vancomycin 12.5 mg/mL eye drops and natamycin ophthalmic suspension 5% (Natacyn, Eyevance Pharmaceuticals) were ordered, and both were available within 36 hours of presentation. The initial cultures grew nothing but a Staphylococcus species that was later classified as Staphylococcus capitis. The patient continued alternating the vancomycin, gentamicin, and natamycin hourly. He also continued to undergo outpatient surgery for his other injuries. By day 14, it was obvious that his ophthalmic presentation was worsening (Figure 2).
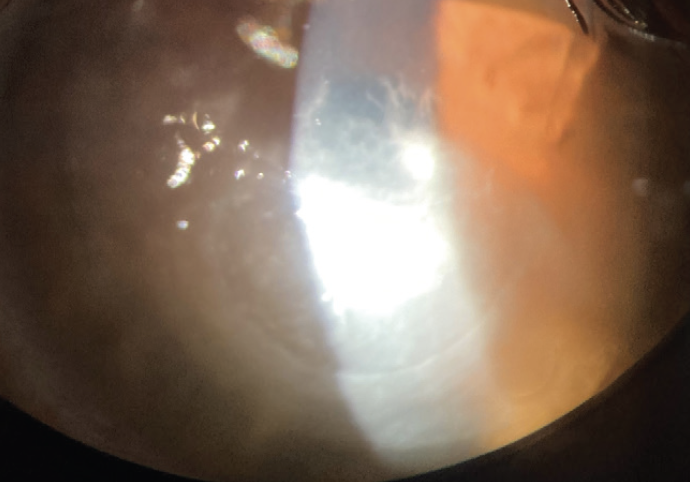
Figure 2. The appearance of the left eye 2 weeks after the hourly alternating administration of vancomycin, gentamicin, and natamycin eye drops was initiated.
At this point, it was decided to remove the LASIK flap for therapeutic reasons and culturing (Figure 3). After its amputation, the flap was divided into four pieces, which were sent for bacterial, fungal, and anaerobe culture and maceration for additional testing if indicated. Final reports were positive for S capitis, which was sensitive to everything, including vancomycin and gentamicin. The initial reports were mold species, which were later identified as Chaetomium homopilatum.2,3 Systemic fluconazole (Diflucan, Pfizer) and voriconazole were added to the patient’s drug regimen owing to lack of response (Figure 3).
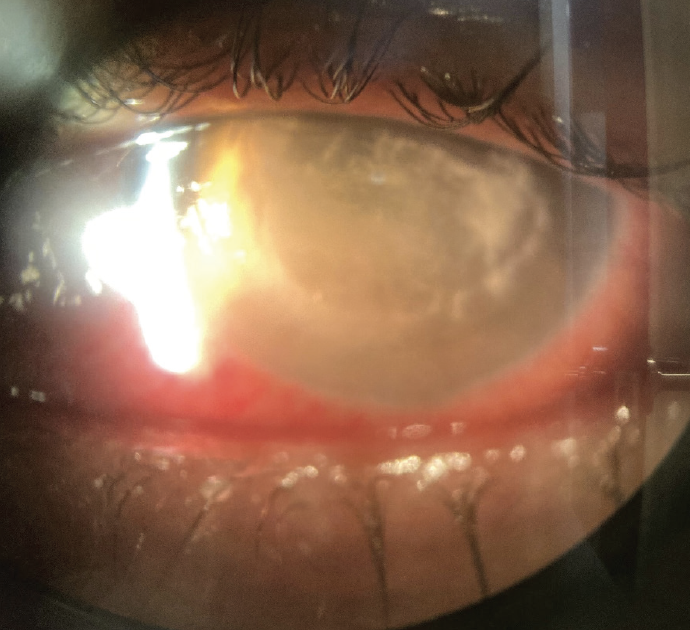
Figure 3. One day after removal of the LASIK flap.
Three weeks after initial presentation, the patient started to show improvement, but the epithelial defect was not healing (Figure 4). Cengermin-bkbj ophthalmic solution 0.7% (Oxervate, Dompé) was therefore added to the regimen, and the size of the epithelial defect subsequently decreased significantly (Figure 5).
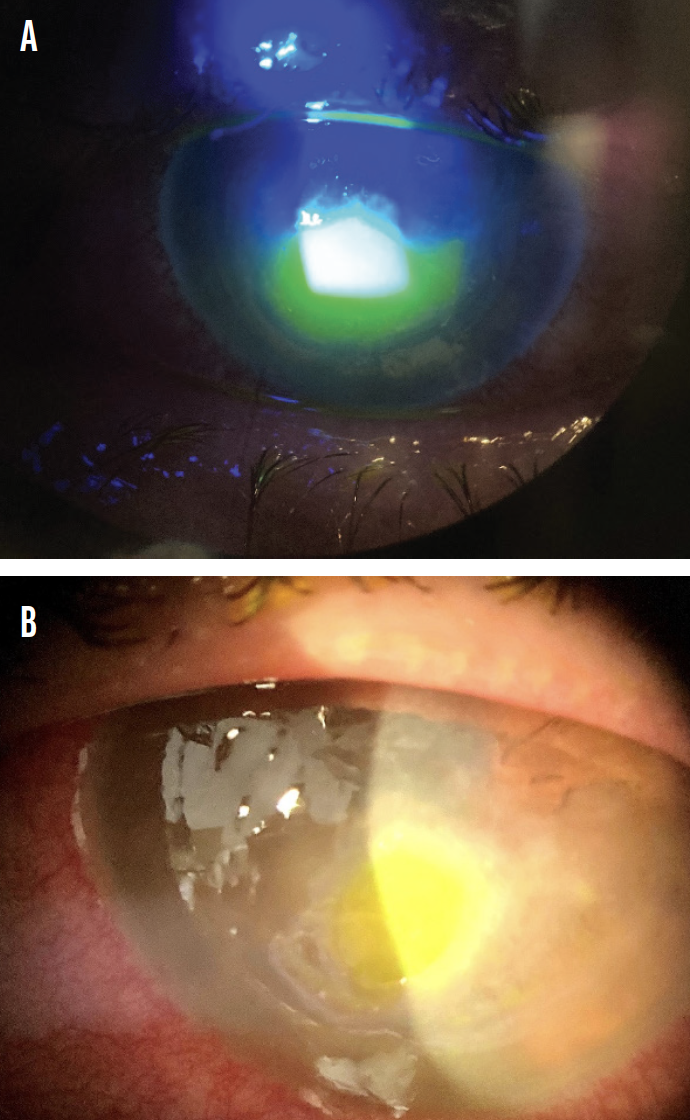
Figure 4. Fluorescein staining of the cornea 3 weeks after initial presentation (A). The appearance of the infection has improved, but severe inflammation remains after systemic fluconazole and voriconazole are added to the patient’s drug regimen (B).
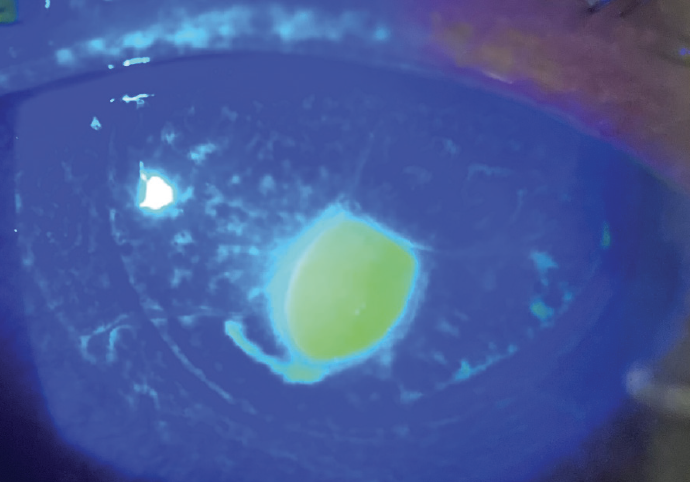
Figure 5. A significant reduction in the size of the epithelial defect is seen after cengermin-bkbj ophthalmic solution 0.7% is added to the patient’s drug regimen.
The antifungals were continued with a dosing frequency of four times per day for 8 weeks and then stopped. The antibiotics were stopped after a total of 4 weeks of treatment. Cengermin-bkbj ophthalmic solution 0.7% was continued for a total of 2 weeks. After a total of 8 weeks of therapy, the patient reported a significant improvement in vision. Six months after the initial trauma, his UCVA was 20/60, not improved with pinhole or refraction. The defect had completely reepithelialized (Figure 6).
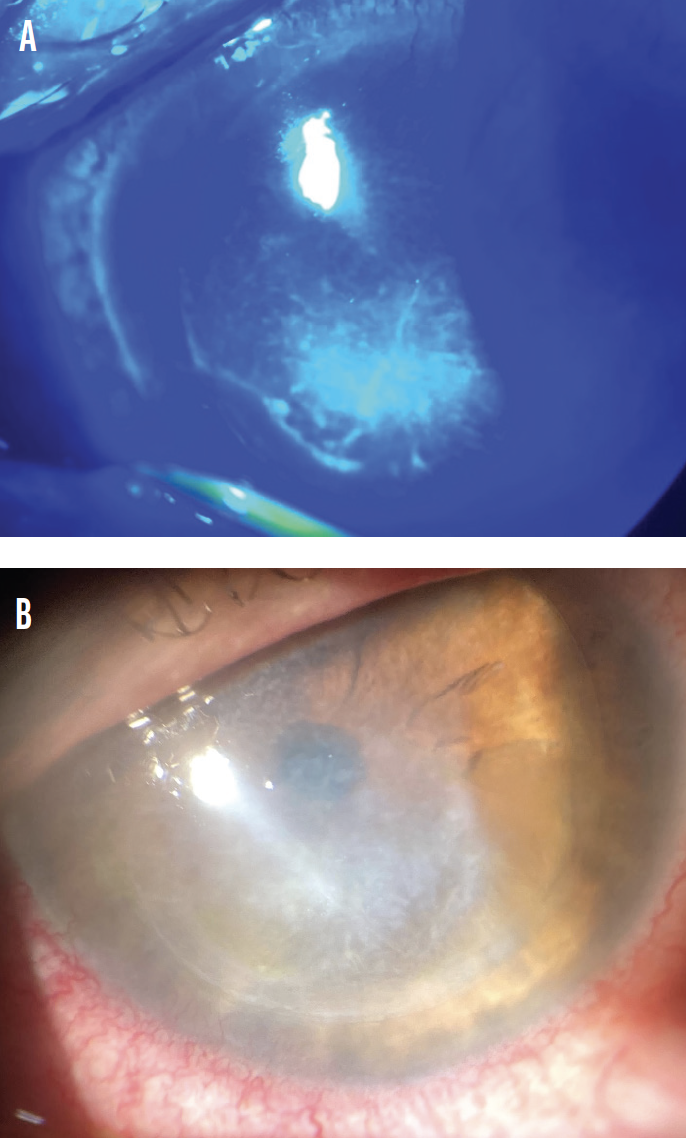
Figure 6. Six months after the initial trauma, there is no fluorescein staining (A), and reepithelialization of the defect is complete (B).
1. Todd T, Mondzelewski T, Cason J, et al. LASIK flap stability after severe ocular injury. Am J Ophthalmol Cas Rep. 2020;18:100608.
2. Kaliamurthy J, Kalavathy CM, Nelson Jesudasan CA, Thomas PA. Keratitis due to Chaetomium sp. Am J Ophthalmol Cas Rep. 2011;2011:696145.
3. Reddy M, Venugopal R, Prakash PY, Kamath YS. Corneal ulcer due to a rare coelomycetes fungus Chaetomium strumarium: case report and global review of Chaetomium keratomycosis. Indian J Ophthalmol. 2017;65(9):871-874.


