Editorially independent content supported with advertising from

Technological advances in our field have grown by leaps and bounds in the past several years, allowing ophthalmologists to not only improve patients’ vision but also refine it. In concert with this is the evolving understanding of astigmatism management in cataract and refractive surgery. Proper and comprehensive management of astigmatism can lead to excellent visual outcomes. Communication regarding diagnosis, treatment, and treatment planning is crucial between the treating ophthalmologist and the patient, as well as with other providers involved in his or her care (optometrist, optician, etc.).
Astigmatism evaluation starts the moment a patient is worked up for examination. Auto-refraction, automated keratometry, manual keratometry, and manifest refraction can provide a great deal of information regarding a patient’s refractive status. Any discordance between values found from these examinations should prompt review and perhaps repetition of the test(s). Corneal tomography and topography (eg, Pentacam; Oculus Optikgeräte) can provide important information in patients who demonstrate high degrees of astigmatism and/or irregular astigmatism.
IS IT REAL?
An important concept to understand is that untreated or poorly treated ocular surface disease can simulate irregular astigmatism and cause fluctuations in astigmatic measurements from visit to visit. The Prospective Health Assessment of Cataract Patient Ocular Surface (PHACO) study highlighted the high prevalence of dry eye in the cataract surgery populations and the implications of untreated ocular surface disease on visual outcomes.1-3 It has been demonstrated that changes in the ocular surface, even from blink to blink, may elicit variations in topography and keratometry values.1-3 A diseased or poorly treated ocular surface may therefore cause unreliable preoperative measurements and treatment planning and less-than-optimal visual outcomes in cataract and refractive surgery patients.1-3
In addition, the presence of epithelial basement membrane dystrophy (eg, map-dot-fingerprint dystrophy, anterior basement membrane dystrophy) and other superficial corneal degenerations (eg, Salzmann nodular degeneration) may produce erroneous astigmatic measurements. If these conditions are present and significant on examination, especially in a preoperative (cataract or laser vision correction) patient, it may be worthwhile to perform superficial keratectomy and/or epithelial debridement to allow for normalization of the corneal surface prior to corneal topography, IOL calculations, and biometry measurements. Figure 1 shows an example of irregular corneal topography secondary to a large Salzmann nodule.
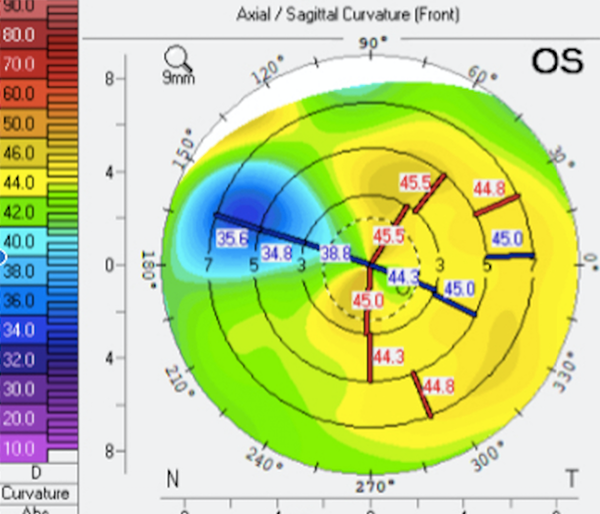
Figure 1 | Irregular corneal topography secondary to Salzmann nodular degeneration.
IS IT IRREGULAR?
Irregular astigmatism caused by corneal scarring, severe ectasia with thinning, or anterior segment dysgenesis often necessitates surgical intervention if vision cannot be improved with the use of glasses or contact lenses. Often, in these cases, definitive treatment is corneal transplantation.
In comparison, irregular astigmatism without severe thinning or scarring is now viewed as a refractive opportunity by many surgeons. A novel approach to management of irregular astigmatism has arisen secondary to the widespread implementation of corneal crosslinking (CXL) for keratoconus and post-LASIK ectasia. Although, in the past, spectacles, rigid gas permeable contact lenses, and intrastromal corneal ring segments (eg, Intacs; AJL Ophthalmics) were the mainstays of therapy, the ability to stabilize keratoconus or ectatic corneas brings about the question, “What next?”4
Topography-guided photorefractive keratectomy (PRK) is a novel approach to addressing this question, as the procedure can “reshape” irregular corneas—in some cases, providing excellent vision.5-11 The unique aspect of this technology is that it can treat steep areas of the cornea with a myopic ablation and flat areas with a hyperopic ablation independently, thereby not only creating a more regular surface but also conserving tissue (versus the magnitude of tissue removed during wavefront-guided treatment).5-11 An example of a keratoconic eye before and after topography-guided PRK (following CXL) is shown in Figures 2 and 3, demonstrating a more regular corneal surface.
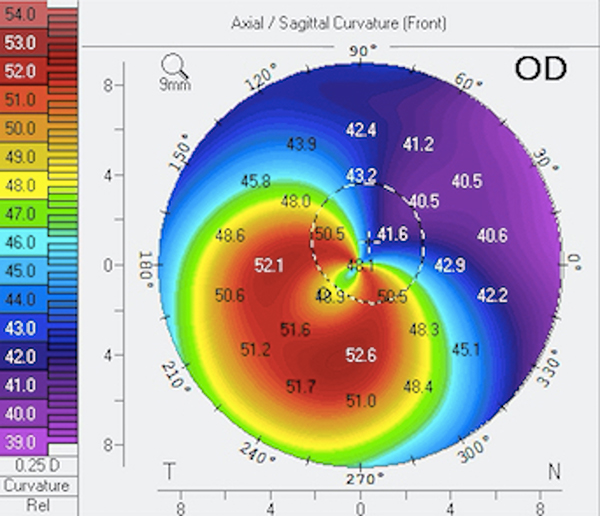
Figure 2 | Before topography-guided PRK in patient with keratoconus.
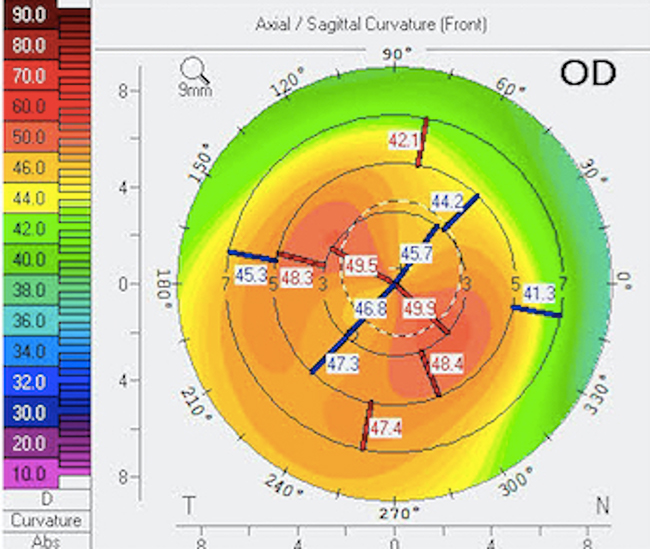
Figure 3 | After topography-guided PRK in patient with keratoconus, with increased topographic and keratometric regularity.
Additional studies continue to be published on diverse techniques with the aim of providing visual improvement in this patient population. These strategies include combinations of PRK and intrastromal corneal ring segments as well as phakic IOL implantation.9,12,17-22
WHAT ABOUT CATARACT SURGERY?
In patients with high degrees of astigmatism, toric IOLs can be successful, but their use should be reserved for cases of regular, stable astigmatism.23-30 In patients with irregular astigmatism, it may be best to implant a monofocal IOL and discuss postoperative options such as rigid gas permeable contact lenses or even topography-guided PRK to further treat residual refractive error.5-9,17-22,31-33
For cases in which a toric IOL will be used, intraoperative aberrometry (eg, the ORA System; Alcon) is helpful in defining and confirming the correct axis placement and IOL power. An additional aspect of treating these patients is that secondary to high myopia, deep anterior chamber, and/or steep corneas, toric IOLs may be at increased risk of rotation following implantation, necessitating surgical repositioning.31-33
CONCLUSION
Astigmatism evaluation and management have evolved tremendously. The ability to perform a wide variety of refractive procedures allows us to not only correct but also enhance vision in patients with both regular and irregular astigmatism. Knowledge of the available tools as well as pertinent exam findings that may affect visual outcomes is imperative to guiding the visual rehabilitation process for our patients.



