A decision by health insurance giant Aetna to require preauthorization of cataract surgery procedures has drawn significant opposition from ophthalmic organizations and many of its members.
On July 1, Aetna made changes to its national precertification list for several procedures,1 the most common of which is cataract surgery. The policy requires preauthorization a minimum of 2 weeks before a cataract procedure is performed for Aetna members.
The decision, which opponents say was made swiftly and without consideration of safety concerns, drove the leadership of the AAO and the ASCRS to release statements voicing their opposition.2,3
“Put very simply, we think it’s unnecessary, disruptive, and burdensome,” David Glasser, MD, AAO secretary for federal affairs, said in an interview with BMC Vision. “Burdensome for patients, their families, and physicians; unnecessary because we don’t think that the issue of unnecessary cataract surgery is as large as Aetna thinks it is. And we don’t think that this method is an efficient or effective way of trying to reduce unnecessary cataract surgery—although we share Aetna’s goal of reducing or eliminating unnecessary surgery.”
Dr. Glasser, an assistant professor of ophthalmology at Johns Hopkins University School of Medicine in Columbia, Maryland, estimates that Aetna covers about 250,000 cataract surgeries per year, including patients with Medicare Advantage or Medicare Part C plans.
Preauthorizations, often referred to as prior authorizations, give health insurance companies a chance to review how necessary a certain procedure or medication may be in treating a condition. Preauthorization has a valid role in the health care process as a way to ensure that a service or drug is truly medically necessary. Opponents of the Aetna policy, however, say the decision to include cataract surgery was primarily a financial decision.
“I don’t think there’s much mystery here—its purpose is to basically slow down the amount of surgery that’s being done, and that’s not good for patients,” Steve Speares, ASCRS executive director, told BMC Vision. “It’s actually stunning that they’ve made this decision, particularly when you consider some of the peer-reviewed work that’s out there regarding [the] prevalence of auto accidents and falls that injure patients because of impaired vision due to cataracts.”
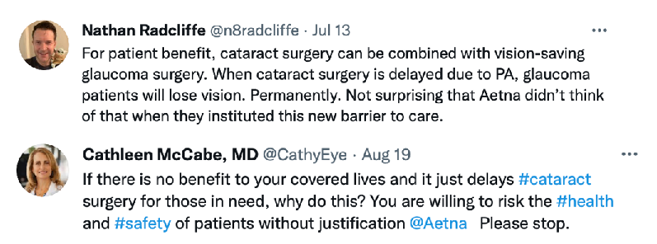
Figure 1 | Ophthalmologists on Twitter responded to the new Aetna policy.
The leadership of both ASCRS and AAO said they met with Aetna a week before the policy went into effect, but both organizations said the insurance company failed to provide concrete reasons why this policy is being implemented.
“In conversations with their leadership, [Aetna] said they want to reduce the risk of unnecessary surgery for patients and also that there was a significant potential financial impact. They said that their internal data suggested that somewhere around 4% to 5% of surgeries were worth investigating with respect to medical necessity,” Dr. Glasser said. “It doesn’t really make sense to disrupt care for every single Aetna beneficiary [who] needs cataract surgery to try to find that 5% or so who may or may not need it. Historically, the estimated percentage of unnecessary cataract surgery has been more in the 2% range, but even at 5%, that’s an awful lot of burden and disruption.”
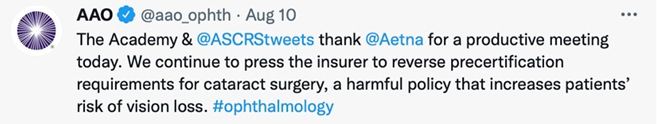
Figure 2 | On August 10, the AAO and ASCRS leadership met again with Aetna to discuss its preauthorization policy.
BMC Vision reached out to Aetna to ask why the company decided to initiate the preauthorization policy for cataract surgery. In an emailed statement, Aetna said, “Over the past few months, we’ve proactively reached out to ophthalmologists in our network regarding our new precertification policy on cataract surgery to inform them of this policy change. We also reached out to the American [Ophthalmological] Society and American Society of Cataract and Refractive Surgery to explain the rationale for and discuss this new policy, [assuring] them that we’d work collaboratively to make sure that their patients and our members would have timely access to appropriate, necessary care, with special attention during the first few weeks of this new policy.”
BMC Vision asked Aetna for more clarification regarding the reason behind the decision to implement the preauthorization policy, but the health insurance giant did not respond to that request.
Adding to the burden of the Aetna policy, according to the ASCRS and AAO, is that the COVID-19 pandemic has already caused a significant backlog of patients who put off undergoing cataract surgery in 2020.4 Studies have shown that ophthalmology was the surgical specialty hit hardest by the COVID-19 shutdown.5
“Practices are already strained all over the United States as they rebound from the pandemic,” Mr. Speares said. “Patients were still hesitant—even as late as March and April—to come in for their regular visits. So, we’ve got a backlog of cataract cases already.”
Aetna first alerted providers to the policy change and the July 1 deadline in its March newsletter.6
On its website, Aetna stated that providers can make their preauthorization request online in a “fast, secure, and simple” manner through its Availity portal (availity.com/healthplans). Providers can also use the electronic medical record system portal. According to administrators, however, the process of obtaining preauthorization is burdensome even with the online portal and, in many cases, costly.
“Any time that there’s a blanket policy on preauthorizations, whether or not they put it in writing, the intent is to restrict or delay access to necessary surgeries,” said Hayley Boling, CEO of Boling Vision Center and Insight Surgery Center in Northern Indiana, which operates four locations and an ambulatory surgery center and has 110 employees.
“On the patient care side, it is a major issue … because we have people [who] depend on their vision not only to be productive members of society but also to live a whole … full, and happy life. By delaying that, even if it’s by several weeks, it really can impact not only the physical health of an individual but also the mental health of an individual,” Ms. Boling said. “The other side of the coin that I look at as the administrator or CEO is … resource allocation. Not only is there a patient access issue because it’s being restricted, but there’s a resource … that the practice has to allocate, which takes more time or effort and therefore more money. If the whole goal in this industry, or in [medicine] in general, is to reduce the cost of care, adding burdens like this actually increases the cost of care.”
There is no uniform way of doing preauthorizations across all insurance carriers. Ms. Boling said that her providers are therefore constantly having to guess and jump through various hoops and that she has dedicated people who “all day long [do] preauthorizations for cataract surgery.”
The ASCRS, AAO, and American Society of Ophthalmic Administrators have called on Aetna to rescind the policy and have asked members to voice opposition directly to Aetna regarding the policy. More details on how to comment may be found at the organizations’ websites.
Although Aetna represents a small percentage of the overall cataract surgery market, opponents say the most significant impact of the policy could be the precedent it sets.
“The problem with having a blanket policy like this with one of the major insurance companies is that it’s essentially a slippery slope for other insurance and payers to say, ‘We’re now going to provide our mandate [for] 100% of cataract surgeries to be [preauthorizations]. We’re also going to do this for other services and procedures as well,’” Ms. Boling said. “It’s a dangerous precedent to set if Aetna continues to push this and not give any leniency.”
1. Changes to our National Precertification List (NPL). Aetna. Accessed July 7, 2021. www.aetna.com/health-care-professionals/newsletters-news/office-link-updates-march-2021/90-day-notices-march-2021/changes-to-our-national-precertification-list.html
2. Statement: American Academy of Ophthalmology and ASCRS urge Aetna to reverse disruptive new policy on cataract surgery. AAO. July 1, 2021. Accessed July 5, 2021. www.aao.org/newsroom/news-releases/detail/aetna-urged-to-reverse-policy-on-cataract-surgery
3. Insurance company policy delays sight-restoring surgery, puts patients in jeopardy. ASCRS. July 1, 2021. Accessed July 5, 2021. https://ascrs.org/news/ascrs-news/ascrs-press-release-regarding-prior-authorization-policy
4. Aggarwal S, Jain P, Jain A. COVID-19 and cataract surgery backlog in Medicare beneficiaries. J Cataract Refract Surg. 2020;46(11):1530-1533.
5. Gillis K. Changes in Medicare physician spending during the COVID-19 pandemic. AMA. March 2021. Accessed July 15, 2021. www.ama-assn.org/system/files/2021-03/prp-covid-19-medicare-physician-spending.pdf
6. OfficeLink Updates. Aetna. March 2021. Accessed July 12, 2021. www.aetna.com/content/dam/aetna/pdfs/olu/officelink-updates-march-2021-olu.pdf


