Presbyopia affects virtually everyone as they begin to approach middle age. Although there are a number of FDA-approved methods designed to correct presbyopia, all of them sacrifice quality of vision at distance. However, a new surgical option nearing submission for FDA approval seeks to change that.
THE VISABILITY MICRO-INSERT SYSTEM
The VisAbility Micro-Insert System (Refocus Group) is the first and only presbyopia procedure performed outside the visual axis (ie, the eye’s line of sight). VisAbility was designed to restore near vision without any compromise to depth perception, or to distance or intermediate vision. Because the procedure is performed in the sclera, VisAbility does not alter or touch the cornea or natural crystalline lens; thus, the eye is completely preserved for future refractive or cataract procedures.

Figure 1 | The VisAbility Micro-Insert.
The VisAbility procedure is the only non-cataract presbyopia treatment that is performed binocularly. It consists of inserting four micro-thin inserts (Figure 1) just below the surface of the sclera in an area covered by the eyelids and is designed to restore the eye’s natural ability to bring near objects back into focus. The inserts are so small that they cannot be felt by the patient or be seen by others (Figure 2). VisAbility inserts are placed under topical anesthesia during an outpatient procedure. The theory behind the technique is to restore tension to the zonules so that the eye’s focusing muscles can once again change the shape of the lens, restoring near vision.
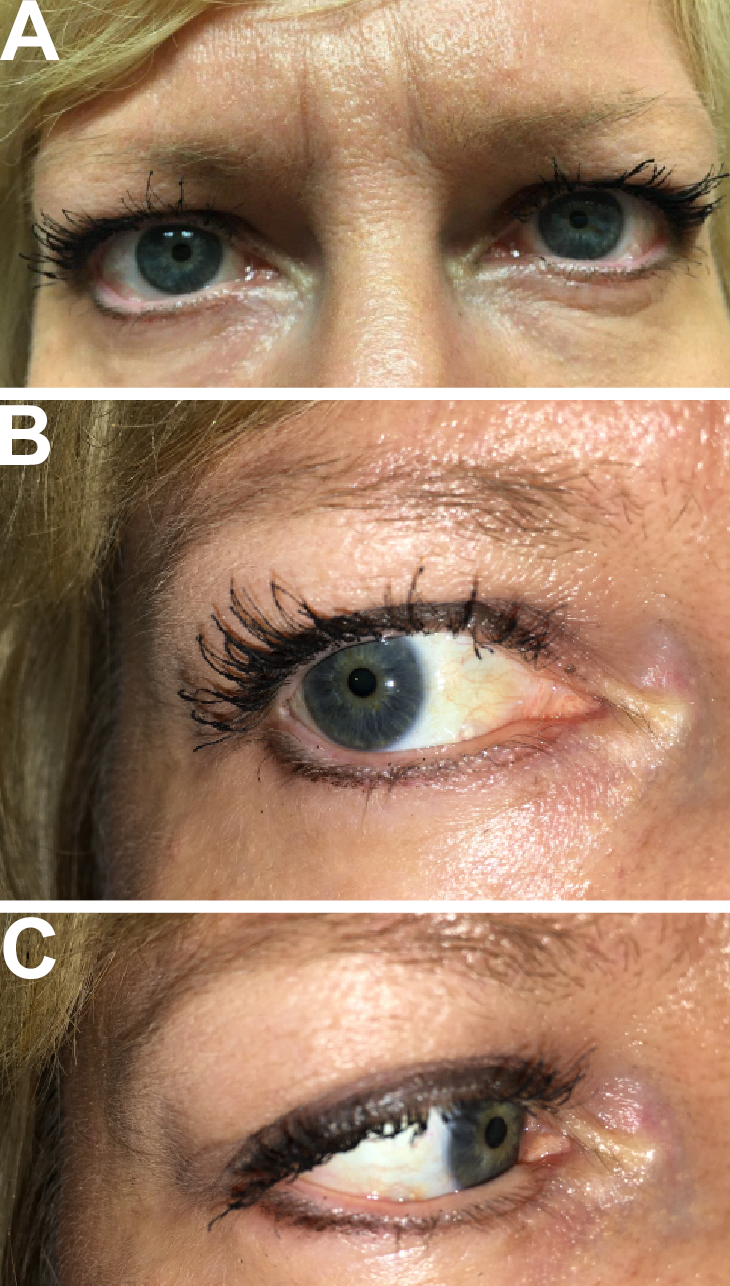
Figure 2 | A patient implanted with the VisAbility Micro-Insert, showing a normal gaze (A), extreme right gaze (B), and extreme left gaze (C).
PERSONAL EXPERIENCE AND RESULTS
When I was first approached by Refocus Group to participate in the VisAbility clinical trials, I was initially skeptical about the potential effectiveness of the procedure. So, I flew to Refocus’ training facility in Jamaica to examine 10 patients who had received the VisAbility Micro-Inserts. All of the patients could read fine print without the aid of reading glasses, whereas before they could not.
I was so impressed with the results that I agreed to participate in the clinical trial. My center operated on 14 patients, and, similar to my experience in Jamaica, I found that patients were seeing well at near postoperatively and were able to read without glasses. Moreover, their near vision continued to improve over time.
As an add-on to the study, my site performed various tests with a dynamic wavefront analyzer, and I was able to document that there was mechanism dynamic change in the refractive wavefront as objects moved closer to the eye. Analysis of the wavefront changes demonstrated a slight myopic shift as well as an enhanced depth of focus of the optical system that was secondary to dynamic induction of spherical aberration as the patient focused at near. None of my patients had any change in distance vision or common side effects associated with other presbyopia treatment options, such as glare, halos, or dysphotopsia.
According to a patient satisfaction survey from an earlier FDA developmental study, 90.3% of patients reported that their near vision was better or significantly better after the procedure. At 12 months postoperatively, 95% of these patients were seeing J3 or better, with many seeing far better than J3. About 18 months ago, a pivotal trial was initiated. This pivotal study enrolled a total of 360 patients between the ages of 45 and 60 at 13 clinical sites across the United States. I implanted the VisAbility Micro-Insert in 35 eyes in the pivotal study. All of my patients, except one, absolutely love the outcome they experienced with VisAbility. The one patient who was not completely satisfied chose to go back to reading glasses, which was possible due to another major benefit of this procedure: It is reversible. If desired, the inserts can be removed, leaving the shape of the cornea unaffected and the crystalline lens intact.
CONCLUSION
VisAbility causes both eyes to work together, so there is no need to adapt to monovision. Although corneal inlays appear to work well for some patients, they all focus at near in only one eye, much like monovision LASIK. VisAbility is the only binocular presbyopia treatment that restores near vision without compromising vision at other distances or depth perception, and I think it is the one procedure that will best stand the test of time.
Refocus Scleral Implant Surgery for Presbyopia
Ken Beckman, MD
I began implanting the VisAbility Micro-Insert System (Refocus Group) in 2015. Below are the surgical steps that I take to ensure a successful procedure and optimal patient outcomes.
The first step in implanting the VisAbility Micro-Insert System involves checking the alignment of the superior and inferior rectus muscles. It is essential to locate the position of the muscles to ensure the scleral implants are placed in between the four rectus muscles, so as not to compromise anterior ciliary circulation. The 12 o’clock and 6 o’clock marks are identified prior to surgery, and then the location of the superior and inferior rectus muscles are identified to confirm these positions.
Next, the axes are marked, and a conjunctival peritomy is initiated with Westcott scissors. Once the conjunctiva is opened into the sub-Tenon space, 2% lidocaine without epinephrine is instilled subconjunctivally. The Westcott scissors are then used to create a 360° peritomy. Once the conjuctiva is recessed, hemostasis is maintained with a sponge. There is no cautery used, again, so as not to compromise the anterior segment circulation.
The docking station is then fixed to the sclera with screw-like connections. Once the docking station is well positioned, an actuator instrument is used to turn the screws 180° to allow firm adhesion to the sclera. The eye is rotated initially to expose the inferior nasal quadrant, which is typically done first. The conjunctiva and Tenons are pulled posteriorly.
A sclerotome creates a uniform 4-mm scleral tunnel, and the scleral implant is attached to a plastic tube and pulled though the scleral tunnel. Once the implant reaches the end of the tunnel, the tube is pulled out, and the back end of the scleral implant holds the implant in place. The open side of the tunnel is then closed with an insert, which snaps into position and secures the implant.
The procedure is repeated in the remaining three quadrants. Once all are completed, the docking station is removed. The eye is then irrigated, and hemostasis is maintained with a sponge, followed by Tisseel fibrin glue (Baxter). After the glue is applied, the conjunctiva is repositioned, and the procedure is completed.





