My surgical center incorporated the Lensar Laser System into practice in 2013, and we have since performed more than 1,600 laser cataract procedures. Although we are confident in the laser’s ability to help deliver the refractive cataract surgery experience and outcomes, we have been tracking our surgical experience for 2.5 years to gain insight into the success of the procedure from the patient’s perspective.
We have found that patient acceptance of laser cataract surgery is very high, with a 40% conversion rate (Figure 1). The surgical process is also easy on the patient. We surveyed our patients to gauge pain and satisfaction with laser cataract surgery. When asked about the pain level during the procedure, the average score was 1 on a 0 to 10 pain scale, with 0 the lowest and 10 the highest amount of pain. The satisfaction rate was very high (“very satisfied”) with regard to overall experience and outcome (scale: very dissatisfied, dissatisfied, no real opinion, satisfied, very satisfied).
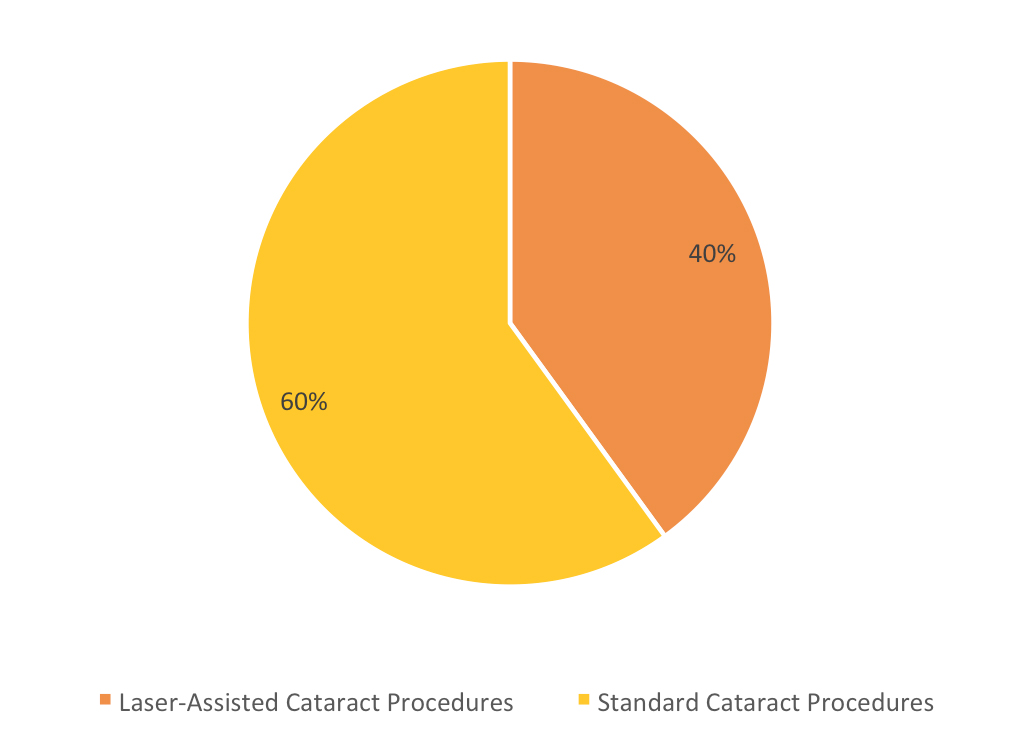
Figure 1 | Patient conversion to laser cataract surgery at Solomon Eye Physicians & Surgeons.
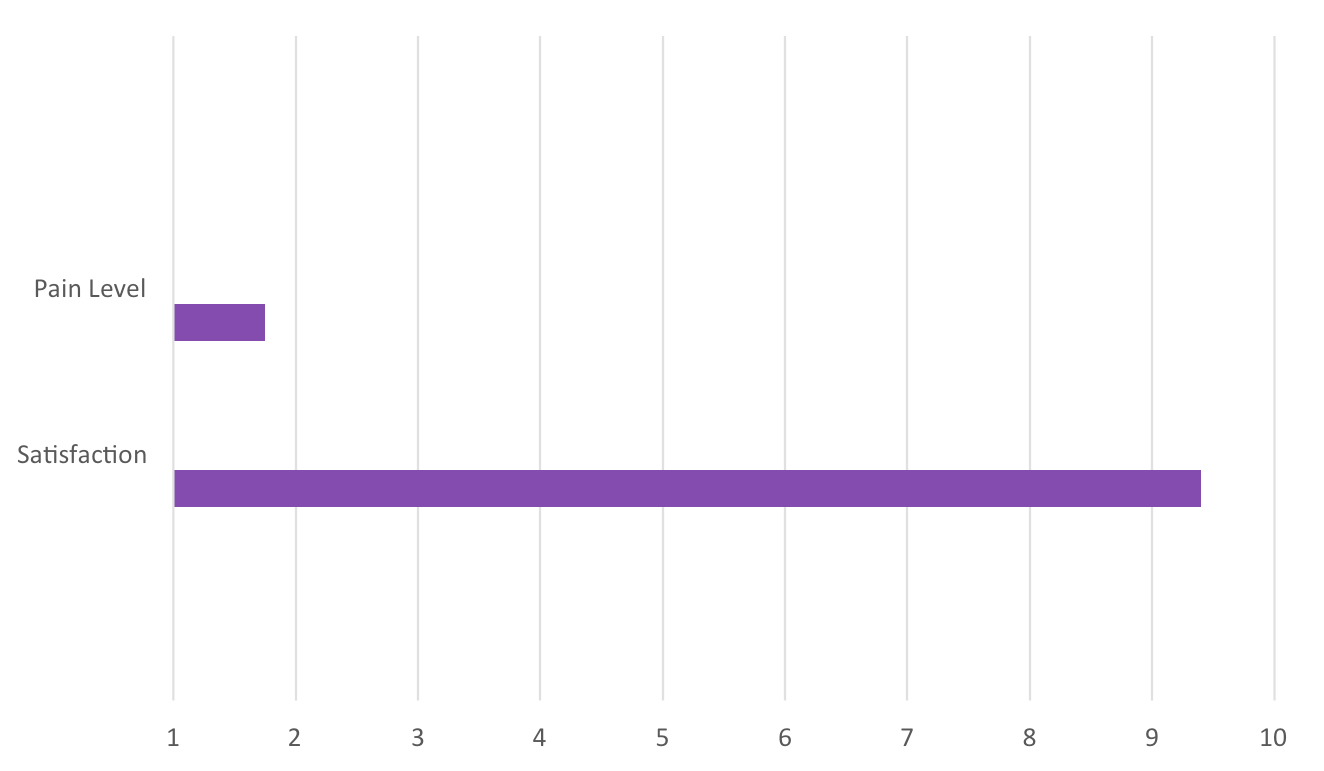
Figure 2 | Patient-reported experience with laser cataract surgery at Solomon Eye Physicians & Surgeons.
NEXT-LEVEL SURGERY
Since implementing the Lensar laser, there are several features I have found to be particularly valuable, including the imaging system and the seamless communication with the Cassini Corneal Analyzer (i-Optics). Specifically, I appreciate the degree of detail of the posterior chamber delivered by the Scheimpflug camera (Figure 3).
This is particularly important in complex cases, such as weak zonules or posterior polar cataracts, and even for hyperreflectivity of the corneal endothelium in cases of Fuchs dystrophy.
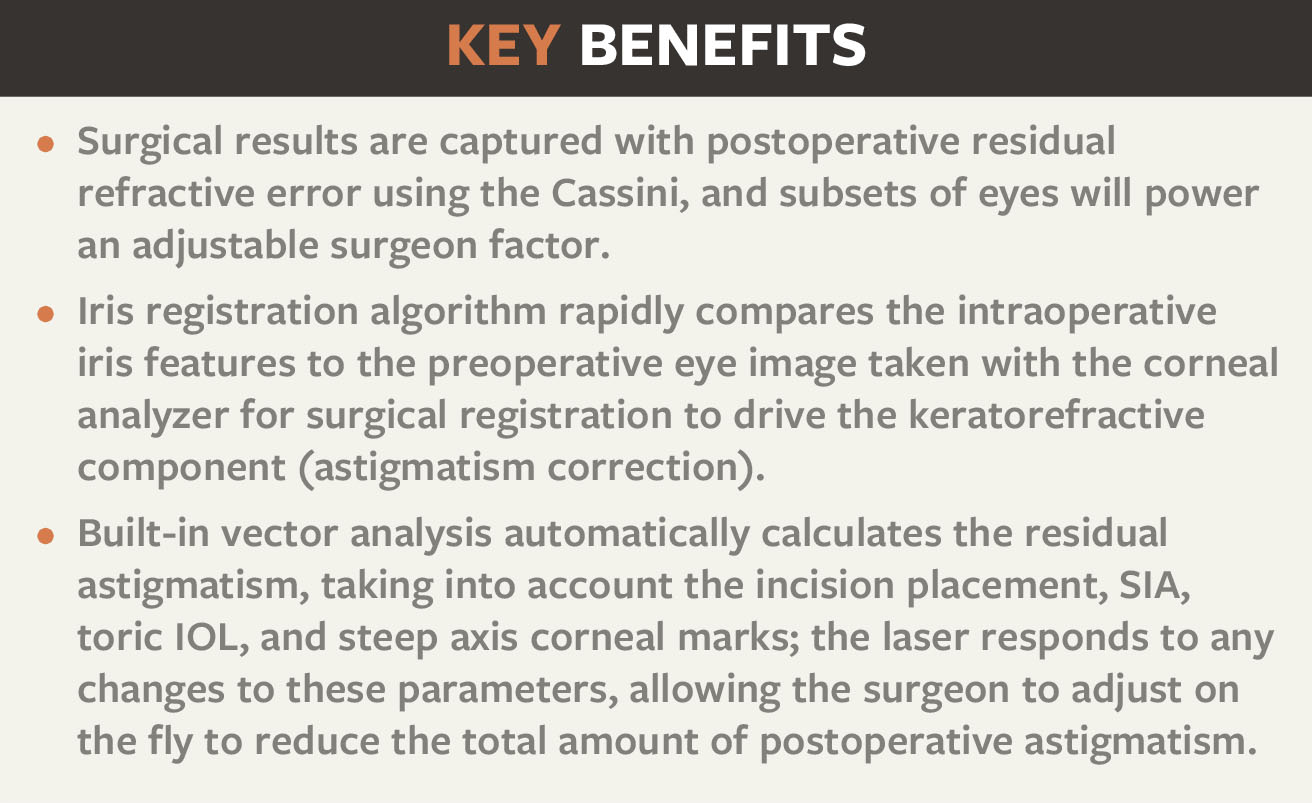
Streamline. Last year, Lensar introduced a package of upgrades to the laser known as Streamline. As part of Lensar’s beta team for the development and rollout of these performance applications, I will share my overall impressions as well as a few tips and takeaways for those who are either new to the platform or to laser cataract surgery altogether.
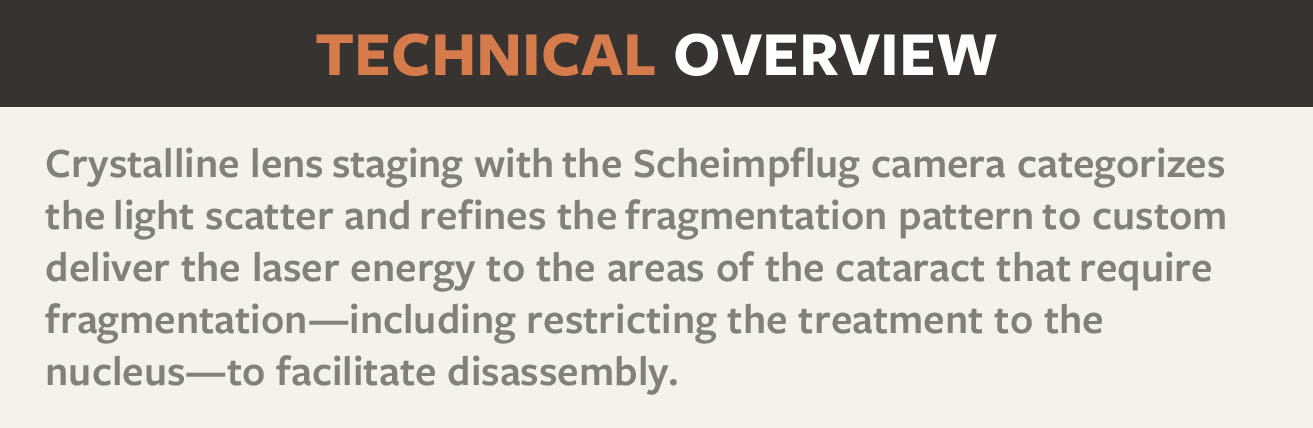
First off is an enhancement to the Lensar laser’s Scheimpflug-based imaging that enables the system to categorize the density of the cataract. The custom settings, based on my parameters per cataract density, work to deliver the laser to areas of interest within the cataract. This is designed to reduce the overall energy load into the eye, resulting in a gentler procedure with minimal postoperative inflammation. These are aspects of the platform that are significant, particularly from a patient perspective, but often get overlooked.
Customization of incisions is a big part of the improvements delivered by the Streamline upgrades. The ability to input my treatment nomograms and know that my preferences are dialed in makes for an efficient procedure. Most surgeon-specific features of the Lensar laser with Streamline are customizable, including the laser patterns, the nomograms for arcuate incisions, and surgically induced astigmatism (SIA).
Personally, I appreciate the nomogram modifiers such as patient age and white-to-white measurement. The Lensar laser enables surgeons to input their SIA as part of preset vector calculations of residual astigmatism—considering the radius of incision, axis, size, and architecture of the primary and secondary incisions—based on preoperative corneal analysis as part of the Streamline software. I anticipate this specific functionality will enable greater refinement of treatments by allowing the surgeon to incorporate and address additional patient-specific variables for each procedure.
With the use of toric IOLs, we tend to do well with correction of high degrees of astigmatism. However, smaller amounts of astigmatism present more of a challenge. A high-quality corneal analysis is wirelessly integrated into the Lensar laser via the Cassini, and then the software establishes registration of the iris after docking. This results in precise arcuate incisions delivered with a depth, radius, and arc length on the incident steep axis. `
In an analysis of 31 eyes treated with the Lensar laser with Streamline, mean preoperative cylinder was reduced from the topographic astigmatism of 1.25 D to 0.40 D postoperatively (P<.001). One hundred percent of eyes achieved a postoperative refractive astigmatism of
≤0.50 D. In my experience, precise and reproducible partial arcuate incisions can be made with the laser without the inherent risk associated with breaching Bowman membrane.
GETTING STARTED
For our clinic, the adoption process was relatively rapid, as I was highly motivated to incorporate the femtosecond laser technology. However, there is a learning curve, and it is a steep one. I recommend focusing on one skill at a time before moving on to the next. Get comfortable with the capsulotomy size, next consider the fragmentation pattern, and then move on to your arcuate nomograms. I highly recommend considering one of the preset nomograms or modifying your own based on bladed limbal incisions. Finally, refine your incision architecture to facilitate wound healing and generate a reliable SIA.



