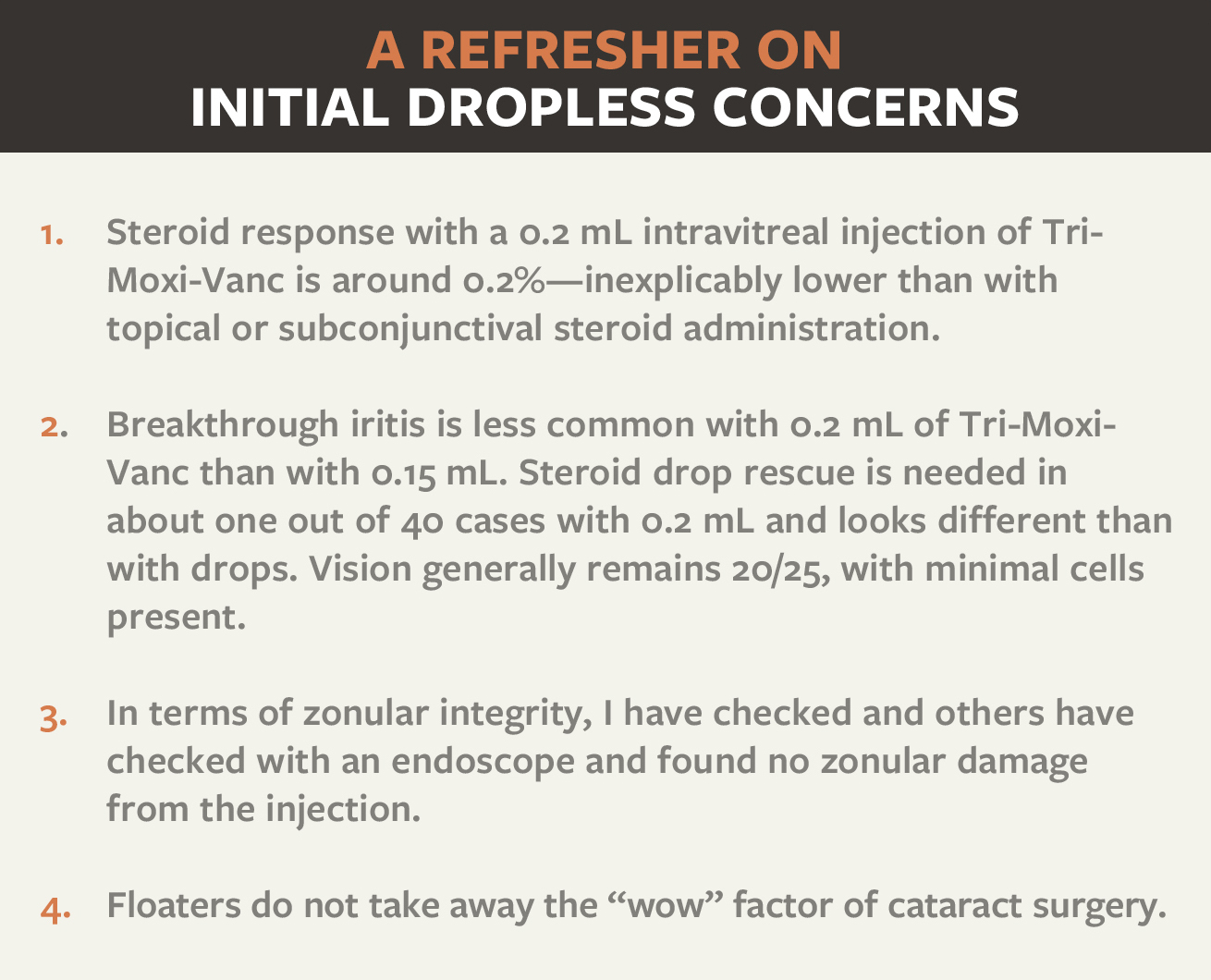
Questions surgeons have prior to transitioning to dropless cataract surgery evolve after their first few cases. Beginning concerns, such as steroid response, breakthrough iritis rates, zonular integrity, and how much to inject, become nonissues as surgeons grow more experienced. However, new uncertainties may take their place. This article details my top five pearls for intermediate-level dropless cataract surgeons.
1. Prevent CME: Consider Keeping the NSAID
Cystoid macular edema (CME) is still a leading cause of diminished vision after cataract surgery.1 Studies conducted by Jeffrey T. Liegner, MD,2 and M. Stewart Galloway, MD,3 have shown that using Imprimis Pharmaceuticals’ injectable compounds, Tri-Moxi (triamcinolone acetonide and moxifloxacin hydrochloride) and Tri-Moxi-Vanc (includes vancomycin), during cataract surgery yields essentially the same CME rates as using steroid drops.
In reviewing the past 10 years of patient results, I found my CME rate was 1.9% when using a nonsteroidal, an antibiotic, and steroid drops. Initially, when I switched to dropless therapy, I did not want give up all my drops. So, I kept the steroid drops post procedure. My CME rate remained at 1.9%. I concluded that using Tri-Moxi-Vanc is equivalent to using a steroid and a nonsteroidal drop. Using a steroid drop with Tri-Moxi-Vanc doesn’t really add value.
I now use Tri-Moxi-Vanc along with a nonsteroidal and have had no incidence of CME in the first 3 postoperative months for more than a year. Adding NSAID drops after injecting Tri-Moxi-Vanc is setting a new bar for avoiding CME. It isn’t equal to steroid and NSAID drops postoperatively; it’s better.
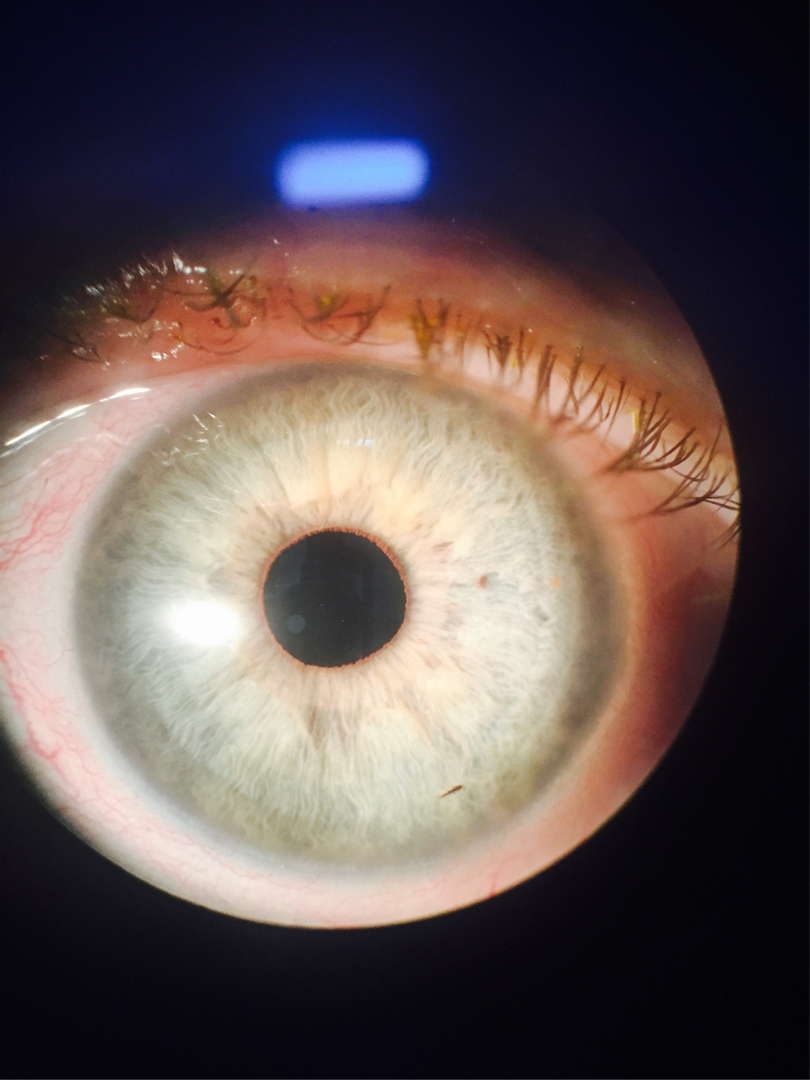
Figure 1 | The worst case of iritis Dr. Mahootchi has seen from Tri-Moxi-Vanc—and it is barely noticeable.
2. Reduce Breakthrough Iritis
In my experience, the incidence of breakthrough iritis since starting dropless therapy is about 2% to 5%. I have found that injecting a slightly higher dosage of Tri-Moxi-Vanc—2 mL rather than 1.5 mL—seems to reduce this number even further, perhaps to one in 40 patients at the 3-week postoperative mark, and most incidences are 20/25 with trace cell iritis. If I prescribe an NSAID, the number drops to less than 2%. If you have reflux of the drug into the anterior chamber, then reinject up to .1 cc or put some in the sub-Tenon space.
3. Don’t Sweat a Shallow Chamber
If the anterior chamber is crowded after surgery, or if you do not have quite enough viscoelastic to create space under the iris for a transzonular injection, this is not an issue. Simply finish the case as usual. Close the wounds and inject transsclerally 3.5 mm posterior to the limbus. Then burp the paracentesis to lower the intraocular pressure.
4. Avoid Capsular Block
Occasionally, if a very low-power lens or flexible lens such as the Crystalens (Bausch + Lomb) is used, the vitreous can swell and push the lens forward, sometimes abutting the anterior capsule and causing a myopic outcome or capsular block. To avoid this, tap down on the lens with the I/A handpiece after injecting the drug. This maneuver ensures that the lens is not sticking to the inside of the anterior capsule. If the lens is not tapped down, the paracentesis can be opened in order to tap the lens down, but this problem is easily avoided with care and attention.
VIDEO | Zonular integrity is much like the process demonstrated here.
5. Make Floaters a Nonissue
Some surgeons worry about the loss of the “wow” factor after surgery caused by the drug floating in the vitreous. Here is a simple pearl to make that a nonissue: Simply tell patients to spend the rest of the day sitting up. I tell them if they want “extra credit,” they can sleep in a reclining chair or with an extra pillow. Using this trick, the drug is not visible without looking way beneath the arcades. Half the time, the drug is minimally visible even by an Optos camera.
I tell patients about possible floaters, but most are willing to deal with them in order to avoid the cost and inconvenience of multiple drops throughout the postoperative period. In practice, most patients are 20/25 or so the first day, and floaters do not diminish the experience or “wow” factor.
Video | Optos photos from a Tri-Moxi-Vanc patient on postoperative day 1.
An Added Bonus
With dropless therapy, I used to think I was saving the patient money and driving down the cost of care. Although patients are thankful for the cost savings, the economic advantage I didn’t anticipate is that the $350-plus that the patient does not have to spend at the pharmacy is now available to spend on things I can offer to improve his or her life in the long term. Toric or presbyopia-correcting IOLs are now more affordable to the patient, so that money saved by going dropless can be spent in your practice. A premium lens has longer benefit than any postoperative drop!
As physicians, our goal is always to offer patients the best care possible and to strive to improve outcomes. With the dropless approach, we can not only save the patient money and reduce infection but also offer improved and more convenient outcomes.
1. Loewenstein A, Zur D. Postsurgical cystoid macular edema. Dev Ophthalmol. 2010;47:148-159.
2. Liegner J. Better surgery through chemicals. Paper presented at: the American Society for Cataract and Refractive Surgeons Annual Meeting; April 25-29; Boston, MA.
3. Galloway MS. Intravitreal placement of antibiotic/steroid as a substitute for post-operative drops following cataract surgery. Paper presented at: the American Society for Cataract and Refractive Surgeons Annual Meeting; April 25-29; Boston, MA.



