At present, Vance Thompson Vision employs three surgeons, one surgical fellow, five optometrists, and 87 other staff members. The practice, which started with 14 employees, has continued to grow over the past 10 years, and we are extremely proud of our program today. In addition to our internal efforts, members of our team work with between 15 and 20 practices per year, helping them grow in the eye care space.
Our program is rural in nature. Many facets of care, such as where patients want to spend their time pre- and postoperatively, are the patients’ choice. But, overall, what we have found in our program and in programs across the country is that there are some challenging numbers staring us in the face as we look at the next couple of decades of how we plan our care.
We offer a full range of procedures—laser cataract surgery, LASIK, MIGS, corneal inlays, and so on. However, whatever the marketplace might be, the metrics that are challenging us are not steered by consumer confidence. Instead, they are rooted in fundamental access issues. So, the first question to ask before delving into the numbers is: Is your center filled with the right types of patients?
GETTING OUTPACED
The number of Americans over the age of 60 is projected to top
112 million by 2050—just 34 years from now. That is up from an estimated 62 million people today. The good news is that those who are in a business that has an age-related offering—as we are—will be very, very busy.
The not-so-good news is that while patient populations are growing, well-trained doctors are not keeping pace. In the optometric world, the number of practitioners remains relatively static at roughly 41,000. That is expected to rise about 27% by 2024, so there is a glimmer of hope there.
Ophthalmology, however, is flat, with approximately 18,000 ophthalmologists currently in practice and 18,000 ophthalmologists estimated to be in practice in 2024. Meanwhile, residency positions for incoming ophthalmologists are on the decline, down 11% over the past few years. The total number of ophthalmology residency slots is just over 1,000. To bat, reimbursement in both optometry and ophthalmology will continue to decline.
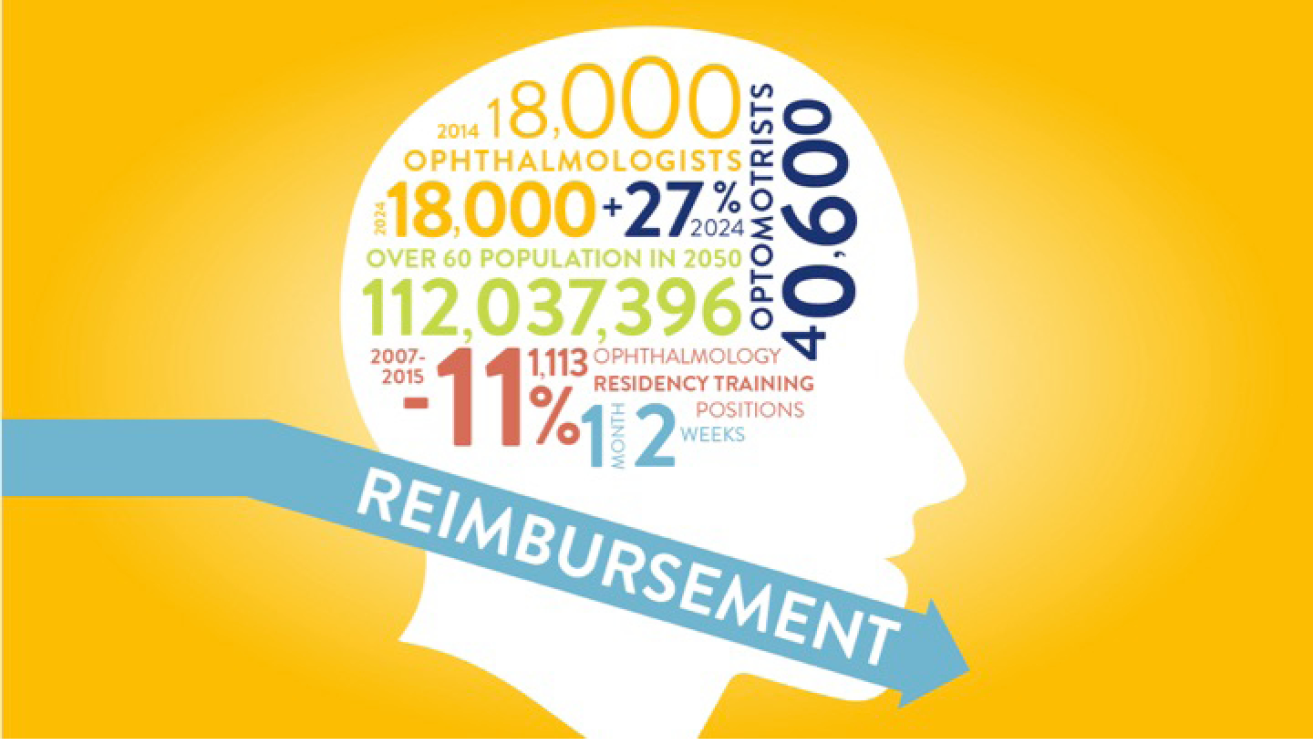
In short, the aging population is spiking, access is decreasing, reimbursement is declining—and we have a conundrum.
TRANSITIONING CARE
Meanwhile, in typical surgical programs around the United States, clinics are full of contact lens re-checks and monthly intraocular pressure checks. These appointments are taking the spots of our valuable surgical consultations and offerings. The question then is: Is the best hope for a bright future in ophthalmology to collaborate more with optometry and find ways to get routine diagnostic pre- and postoperative refractive and cataract care back into optometry offices?
Optometrists already have long-standing relationships with patients, and they have invested in advanced diagnostics as we have invested in advanced surgical options. Transitioning some care to optometric offices will, in turn, create greater capacity to take referrals for advanced surgical procedures in the future.
Until a few years ago, our patients were scheduled out a long time because of the challenging statistics mentioned above. We decided to issue an edict requiring any new consultation to get in to see us within 2 weeks. From there, any new consultation has surgery within 2 weeks of that. Ultimately, if a patient is coming in as a new consultation, he or she will have surgery within 1 month. That is how we measure our performance with access.
SUMMARY
According to CNN Chief Medical Correspondent Sanjay Gupta, MD, one of America’s 9 biggest health issues today is access.1 In an effort to cope with the impending aging population and doctor shortage, Dr. Gupta notes that the following questions must be considered:
• Is there any way to increase the number of residency training slots?
• Are there any other health care professionals who can reasonably fill in the gaps?
If we can take some of the components of our clinics and transition them to primary care, we can likely open up capacity opportunities for the increasing surgical volume that is headed our way.
1. Gupta S. America’s 9 biggest health issues. CNN. January 5, 2015. https://www.cnn.com/2015/01/02/opinion/gupta-health-challenges-2015/. Accessed June 8, 2016.