Most days, I’m not only a physician but a comedian and a magician as well. Just putting eye drops in becomes a game of, “Hands on your belly so the drops don’t come out your belly button!” (Note: This usually only works for the first drop.) Checking eye pressure becomes a game of, “Count the beeps.” And just getting a view of the fundus often involves the old “I bet I can see what you had for breakfast if I look in your eyes.” (Pancakes? No … yogurt? No … oh, I see it now: pepperoni pizza!—that one usually gets a giggle.) If you haven’t already guessed: I’m a pediatric ophthalmologist.
My favorite part about my job is the variety of conditions I see and treat. One day in the operating room can include a congenital cataract, secondary IOL, nasolacrimal duct intubation, goniotomy, and strabismus surgery. And if you’re thinking my job couldn’t get any more fun, I also see adults with complex strabismus and diplopia (as if the squirmy kiddos weren’t enough to keep me on my toes).
Many of the treatments and surgical techniques we use as pediatric ophthalmologists have been around for decades, but there are also new and exciting things happening in our field. This article details just a few.
ATROPINE FOR THE TREATMENT OF MYOPIA
Even if you primarily treat adults, you’ve probably heard about the use of atropine in slowing myopia progression in children. The mechanism of action is unknown, but it’s thought that atropine inhibits stretching of the sclera and therefore eye growth. Studies comparing atropine 0.5%, 0.1%, and 0.01% found that, while the higher doses were initially more effective, patients had a greater rebound after discontinuing the drop, resulting in the 0.01% group having significantly lower myopic progression.1 It was estimated that atropine 0.01% slowed myopia progression by 50%. There was minimal pupil dilation or loss of accommodation and no decrease in near vision. Because the drop has to be compounded, cost and availability are the biggest challenges in implementing this treatment in my practice; however, many families are happy to have something to try when their child’s myopia is progressing rapidly or there is a strong family history of high myopia.
ANTI-VEGF FOR THE TREATMENT OF ROP
When the results of the BEAT-ROP study were published in 2011,2 many clinicians became excited about the possibility of using bevacizumab (Avastin; Genentech) for the treatment of retinopathy of prematurity (ROP). The advantages of bevacizumab over laser include its ease of administration, no need for general anesthesia, rapid response, and significantly lower degree of myopia. However, the disadvantages are significant and include delayed vascularization and therefore possibly late recurrence. Recurrence has been reported up to 7 months post-menstrual age, and long-term frequent exams are required. This may mean confirmatory exams under anesthesia, as these older infants are difficult to adequately examine in the clinic. Furthermore, it is unknown what the long-term side effects of this treatment may be, as some of the drug is absorbed systemically. Although there is still much to be learned about the use of bevacizumab for ROP, it continues to be used by many physicians for zone 1 ROP and in countries where access to laser may be limited.
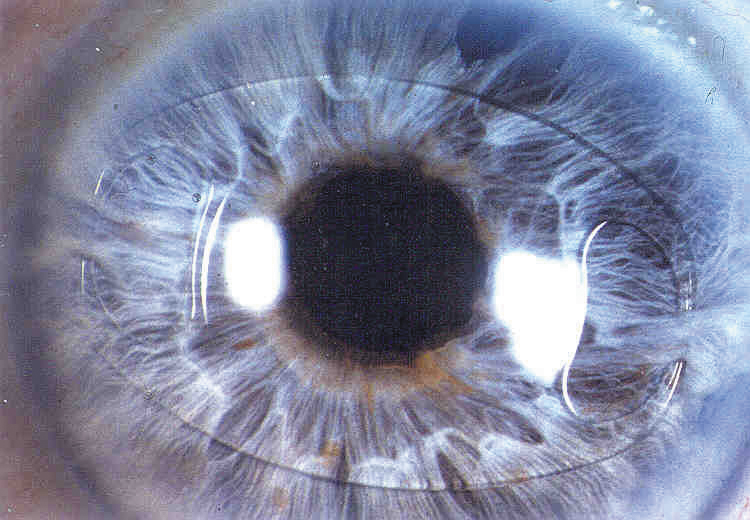
Figure 1 | The Artisan IOL (Ophtec) is an iris-clip lens being studied for use in pediatric patients with aphakia.
the ARTISAN IRIS-CLIP LENS
The Artisan IOL (Ophtec; Figure 1) is an iris-clip lens that is being studied in an FDA clinical trial for use in pediatric patients with aphakia. This lens is designed for primary or secondary implantation in patients in whom a standard posterior chamber IOL is contraindicated, such as in eyes with poor or no capsular support. This lens has unique advantages in children because it can be unclipped from the iris and replaced as the refractive error changes. In patients with Marfan syndrome already at a high risk of retinal detachment, a particular advantage may be that no manipulation of the posterior segment or vitreous is required, as would be with a scleral-fixated IOL. The prospective ongoing trial in the United States will help to determine the safety and efficacy of the Artisan IOL in children with aphakia.
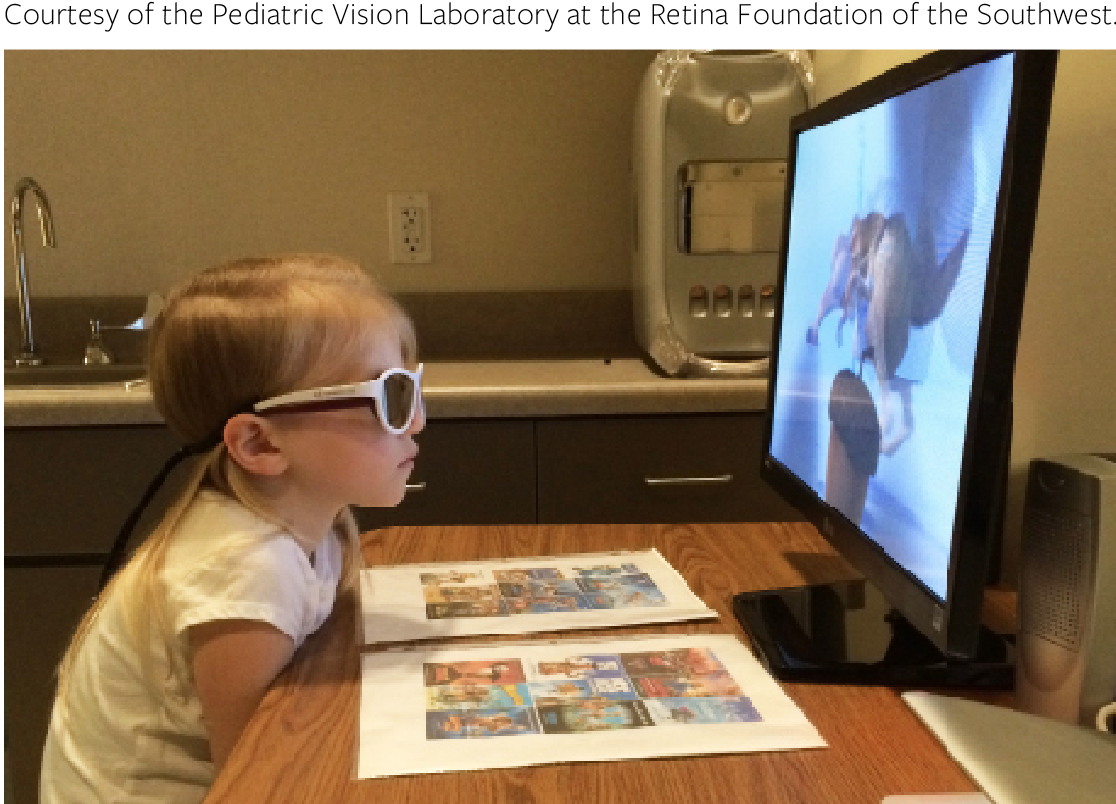
Figure 2 | A child with amblyopia watches a dichoptic movie on a passive 3-D display while wearing 3-D cinema glasses.
DICHOPTIC THERAPY FOR AMBLYOPIA
Traditionally, amblyopia has been thought of as a unilateral problem, with patching being the mainstay of treatment. However, as we are learning that amblyopia is actually a binocular disorder, new research is focusing on treatments that include using both eyes together, called dichoptic therapy (Figure 2). Studies are using an iPad game with stereovision glasses, allowing each eye to view a separate image.
Contrast imbalance is induced to overcome suppression of the amblyopic eye and allow binocular vision. This form of treatment was initially created as a Tetris video game, but now the passive viewing of movies is being studied, which could help with compliance. The results have been encouraging, but this new treatment option is not widely available yet. It is also exciting that this technology has shown some promise in the treatment of adults with amblyopia.
SUMMARY
These are just a few of the exciting things happening in the field of pediatric ophthalmology. I am grateful for a career that is both fun and rewarding, and I hope to spark an interest in our future generation of ophthalmologists.
1. Chia A, Chua WH, Li W, et al. Atropine for the treatment of childhood myopia: changes after stopping atropine 0.01%, 0.1% and 0.5% (ATOM2). Am J Ophthalmol. 2014; 157:451-7.
2. Mintz-Hittner HA, Kennedy KA, Chuang AZ; BEAT-ROP Cooperative Group. Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med. 2011;364(7):603-15.