A 39-year-old white man with a past medical history of premature birth and amblyopia of the right eye presented with a 3-week history of ocular pain and redness. His review of systems was positive for chronic joint pain and negative for ocular trauma, infection, and ocular surgery. He eventually admitted to recent intravenous drug use. There was a family history of autoimmune disease. Initial exam showed a red, tender, nonfluctuant nodule (Figure 1), and the patient was empirically treated with oral steroids (1 mg/kg per day). Within 1 week, he returned with worsening pain, enlargement of the nodule, and an associated delle (Figure 2). This clinical course was suspicious for an infectious etiology; therefore, a rapid steroid taper was initiated, and he was started on oral acyclovir and sulfadiazine/trimethoprim.

Figure 1 | A red, tender, nonfluctuant nodule located inferotemporally on the right eye
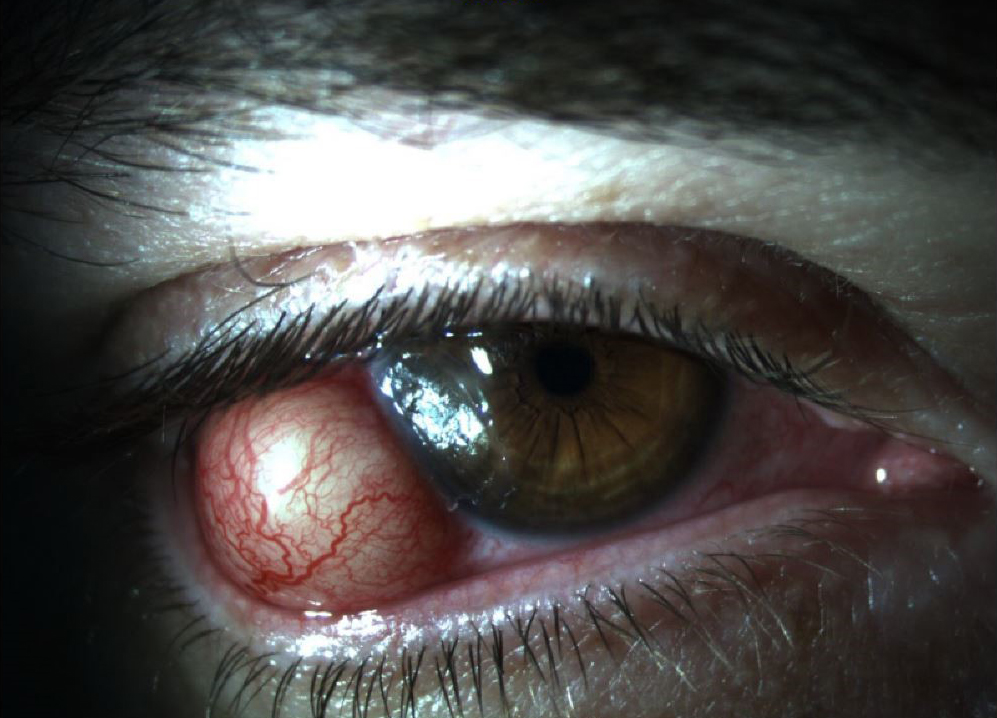
Figure 2 | After 1 week of steroid treatment for presumed nodular scleritis, there was an increase in size, redness, and pain associated with the nodule.
Two days later, the patient returned with purulent drainage from the nodule, which was sent for culture and identified as methicillin-resistant Staphylococcus aureus (MRSA). Acyclovir was discontinued, and topical tobramycin was added. After failing to improve clinically after 1 week, the patient was admitted for intravenous, subconjunctival, and intralesional vancomycin instillation as well as possible surgical debridement. He was admitted for 4 days with an uneventful hospital course and clinical improvement within that time period. Complete resolution slowly took place over 1 month, resulting in localized scleral thinning (Figure 3).

Figure 3 | After resolution of the scleral abscess, a well-circumscribed, flat, colored lesion, consistent with scleral thinning, remained.
A CLOSER LOOK: SCLERITIS
Scleritis typically affects older patients and women more often than men. Infectious scleritis is seen in approximately 5% to 10% of cases.1 Known risk factors include ocular surgery,2 mitomycin C treatment,2 compromised immune system,3 beta irradiation,2 and organic foreign bodies.4 When bacterial scleritis is encountered, the most common organism is Pseudomonas aerugenosa.1 Other infectious etiologies have been reported, including Nocardia,5 Klebsiella,5 fungal agents,5 varicella zoster,6 and herpes simplex virus.7 Otherwise, the majority of cases are associated with systemic autoimmune disorders, rheumatologic disorders, or immunologic processes secondary to infections elsewhere.4
Although exceedingly rare, spontaneous bacterial scleral abscesses can occur, and at least one other case has been reported. In that case, reported by Kiratli et al, the patient was initially diagnosed with nodular scleritis and treated accordingly but was later found to have methicillin-susceptible staphylococcus aureus.8 Furthermore, although they did not report a case of scleral abscess caused by MRSA, Amato et al have suggested that the incidence of ocular MRSA infections in general are increasing.9
SUMMARY
These observations, in conjunction with the case report presented here, should prompt practitioners to consider bacterial causes of scleral nodules when patients have a new diagnosis of nodular scleritis, particularly if the patient is refractory to standard treatment or has an atypical history. We believe that a high suspicion for infectious causes could improve outcomes in cases similar to ours because standard treatment for nodular scleritis may exacerbate the severity of scleral infections.
1. Jain V, Garg P, Sharma S. Microbial scleritis-experience from a developing country. Eye (Lond). 2009;23:255-261.
2. Hodson KL, Galor A, Karp CL, et al. Epidemiology and visual outcomes in patients with infectious scleritis. Cornea. 2013;32:466-472.
3. Moreno Honrado M, del Campo Z, Buil JA. A case of necrotizing scleritis resulting from Pseudomonas aeruginosa. Cornea. 2009;28:1065-1066.
4. Ramenaden ER, Raiji VR. Clinical characteristics and visual outcomes in infectious scleritis: a review. Clin Ophthalmol. 2013;7:2113-2122.
5. Pradhan ZS, Jacob P. Infectious scleritis: clinical spectrum and management outcomes in India. Indian J Ophthalmol. 2013;61:590-593.
6. Loureiro M, Rothwell R, Fonseca S. Nodular Scleritis Associated with Herpes Zoster Virus: An Infectious and Immune-Mediated Process. Case Rep Ophthalmol Med. 2016;2016:8519394.
7. Gonzalez-Gonzalez LA, Molina-Prat N, Doctor P, Tauber J, Sainz de la Maza MT, Foster CS. Clinical features and presentation of infectious scleritis from herpes viruses: a report of 35 cases. Ophthalmology. 2012;119:1460-1464.
8. Kiratli H, Shields JA, Shields CL, Eagle RC Jr, De Potter PC, Friedberg H. Localized transscleral staphylococcal abscess simulating a neoplasm. Ger J Ophthalmol. 1995;4:302-305.
9. Amato M, Pershing S, Walvick M, Tanaka S. Trends in ophthalmic manifestations of methicillin-resistant Staphylococcus aureus (MRSA) in a northern California pediatric population. J AAPOS. 2013;17:243-247.




