The health care landscape is rapidly changing. In order to remain competitive, medical practices must be proactive to stay ahead of these changes. This article highlights three areas worthy of our careful attention and energy: staff training, practice efficiency, and process analysis.
STAFF TRAINING
Staff training is crucial. Today, more and more diagnostic tests are delegated to our technicians. If they do not have the appropriate knowledge and are not empowered to correctly execute their assigned tasks, then we, the surgeons, may be making decisions based on inaccurate information. Consider even a simple task, such as taking a patient’s history. If the staff member asks a patient, “Do you have dry eyes?” what do you think the patient might say? “No, my eyes tear all the time. I walk around with a Kleenex.” Instead, the technician should be trained to ask “Do your eyes feel tired?” or “Does your vision fluctuate?”
Another purpose for technician training is for proper documentation of symptoms, as some insurance carriers require positive answers to validated dry eye questionnaires to reimburse for tests. Further, select tests such as tear osmolarity and InflammaDry (RPS) must be conducted before any drops are instilled; as the ophthalmologist, you need to train your technicians to know when to perform these tests. The same applies to Lipiview (TearScience)—we train our technicians to perform this test if there are any symptoms of dry eye disease. While performing the scan, the technician also educates the patient about meibomian glands in order to shorten the surgeon’s chair time.
Video | Dr. Matossian on her use of Yosi.
Training schedule. At Matossian Eye Associates, we hold 1 hour of training per 40-hour workweek. All of our employees are included: front-desk receptionists, technicians, and billing and marketing staff, as they all must be educated. We have three offices and more than 70 staff members, so we use Skype to ensure that we are all connected and engaged.
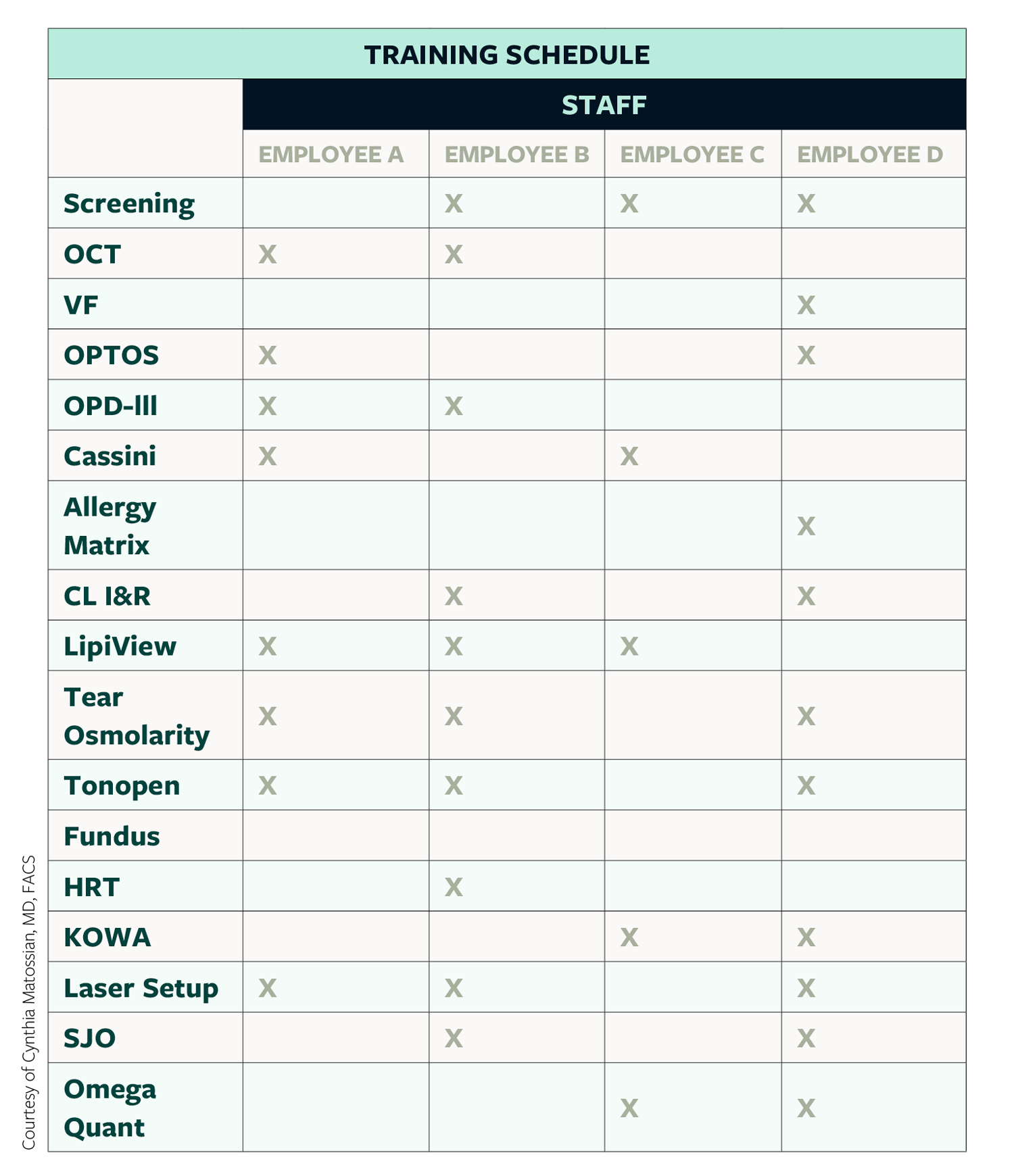
To monitor training, we have compiled a list of all the procedures that our technicians perform, from allergy testing, to topography, to biometry, to omega index (see Training Schedule Grid). Our senior technicians have to sign off on the junior technicians once the appropriate skill level has been achieved. We have a grid and a timeline to track technician training.
In addition, we have a physician observation grid, where our front desk, billing, and marketing teams come to “the back” to spend time with the physicians to help them better understand the science. We also invite all of our staff, including our billers, to come to the operating room so that they can see what eyelid surgery looks like or what cataract surgery entails. Again, this empowers the staff and improves their communication with patients.
Mentor grid. One area that is challenging for most practices is hiring and retaining staff. As a result, we implemented a mentor grid. This is a mentorship program where a new hire is partnered with a senior, more well-trained person in the same department. Through this mentor-mentee relationship, the mentor shepherds the new hire and becomes his or her go-to person to prevent the newbie from feeling lost or intimidated. Because we are asking our mentors to do two jobs—their own and the mentorship—we compensate them for their participation in our mentor program. We pay them every 3 months; by the end of the year, they earn their full mentor bonus if the mentee is still working in the practice.
Monthly chapter club. I realized that our mid-level managers were not receiving adequate training in leadership skills. So, we instituted a monthly chapter club, where we read one chapter on leadership topics and then come together to discuss. We also encourage certification in all departments—not just for ophthalmic assistants, but also for front-desk staff, billers, etc. Lastly, in terms of technician training, I am a cofounder of a company called Progressive Tech Training that offers modular training online, which will launch next year.
EFFICIENCY
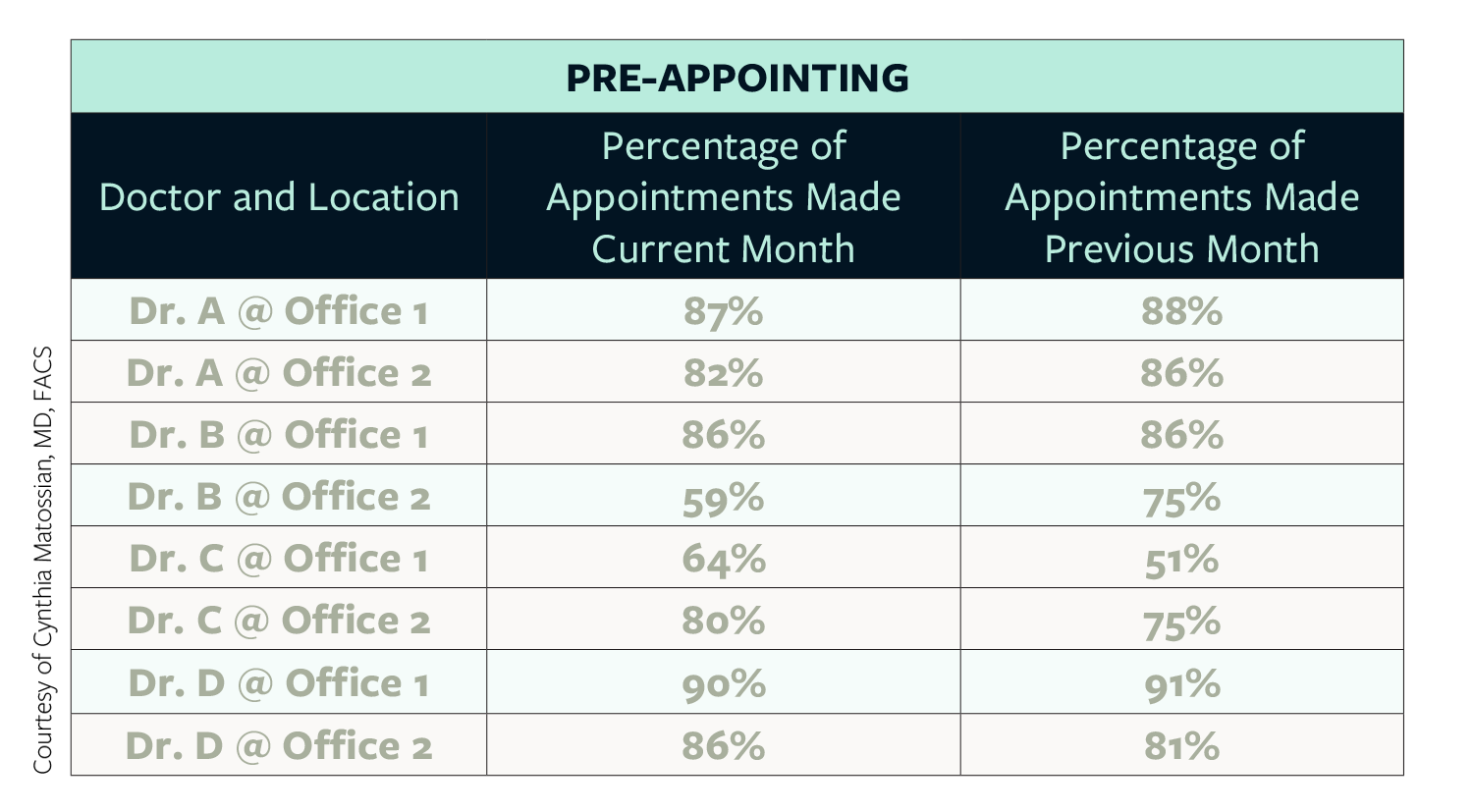
We are all in business. We run small to medium to large businesses. The term pre-appointing refers to the percentage of patients who, at checkout, schedule a return appointment, whether in a week, a month, or a year. We started tracking this per doctor, per office and share this information with our staff (see Pre-Appointing Grid). Since we began following this, our pre-appointing numbers have reached close to 90%.
We also began analyzing the out-of-pocket moneys collected from patients at the time of checkout and now pay close attention to these numbers. When we first looked at this, we found that 9% of cash payments were not being collected at checkout. Now, we are down to 2% not being collected. Another change we instituted was doing cash reconciliation not solely at the end of the day, but at the end of each morning, afternoon, and evening session.
Additionally, we ask our patients how they prefer to be reminded about their future appointments: Is it through text? Email? A human phone call? Or a combination of these options? We use Yosi and SolutionReach.
PRACTICE PROCESS ANALYSIS
When it comes to the success of your practice, it is vital to have your finger on the pulse and to track your benchmarks. We calculate monthly benchmarks and use Market Scope to compare our data against national averages for IOL adoption and conversion rates. We conduct internal chart audits to measure our success in coding and billing. We also analyze our performance on social media. It is important to look at all of these parameters and make adjustments to your processes when necessary.
SUMMARY
A successful practice is a proactive practice. Take steps to train and empower your staff, measure and enhance your efficiency, and evaluate and update your practice processes.




