Ocular surface disease (OSD) can be caused by a multitude of etiologies and, when severe, can lead to debilitating symptoms. Treatments for the various causes can be as varied as the disease process itself. Specialized contact lenses have proven to be a potential and cost-effective treatment for a wide variety of conditions, including OSD and corneal ectasia.
WHAT IS A SCLERAL CONTACT LENS?
Scleral contact lenses are large-diameter gas permeable contact lenses specially designed to vault the corneal surface while resting on the sclera. These specialized lenses thus replace the irregular cornea with a smooth optical surface while also acting as a fluid reservoir to provide comfort to patients with severe dry eye disease (DED).1

Figure 1 | The PROSE lens can provide visual rehabilitation and offer relief for patients suffering from ocular surface discomfort.
(Courtesy of Deborah Jacobs, MD)
The prosthetic replacement of the ocular surface ecosystem (PROSE) treatment (Boston Foundation for Sight; Figure 1) uses an FDA-approved, custom computer-aided designed and manufactured prosthetic device to replace or support impaired ocular surface functions2 and is a leader in the scleral lens field. The fitting process allows for the use of machine-lathed rigid gas permeable fluorosilicone acrylate polymer that rests on the bulbar conjunctiva, allowing for positional stability on the eye. This customization is one of the factors that differentiate the PROSE lens from general scleral lenses. Diameters range from 17.5 mm to 23.0 mm, and vaults to accommodate for no apical or peripheral corneal contact are independent from the base curve.3 Residual spherical and cylindrical refractive error and asphericity are incorporated into the front optical surface of the device to optimize subjective correction of vision.3
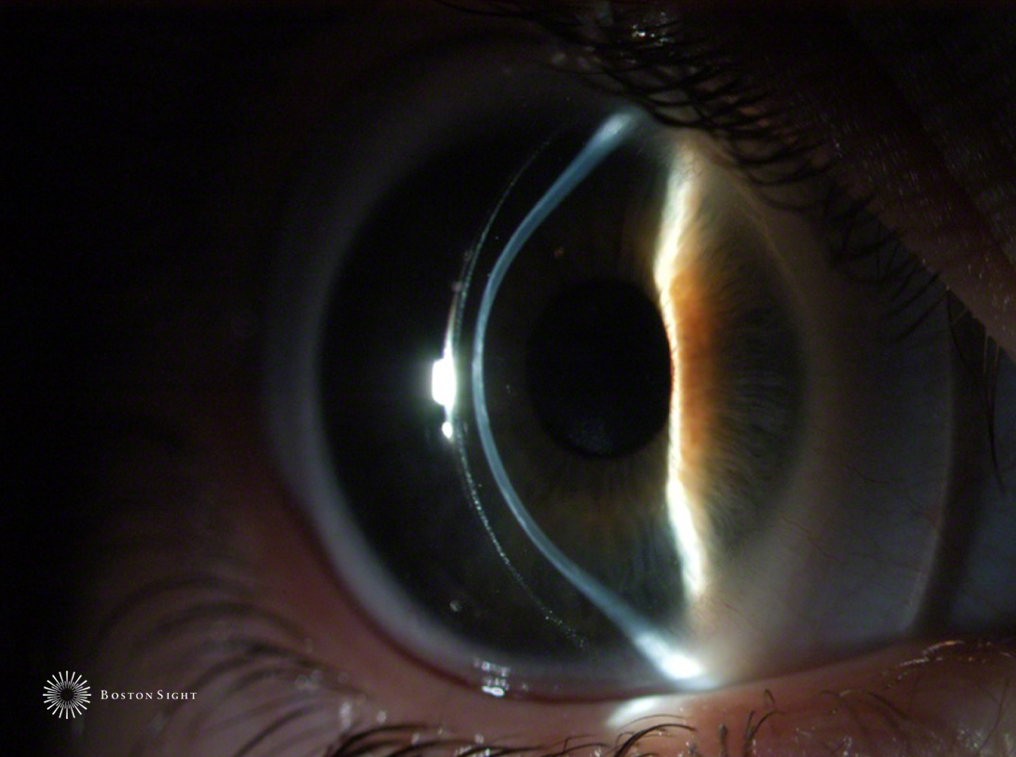
Figure 2 | A slit-lamp photo of the PROSE device worn by a patient with keratoglobus.
(Courtesy of Deborah Jacobs, MD)
PROSE IN CORNEAL ECTASIA
Baran et al3 demonstrated success in fitting and improving vision with PROSE devices in the treatment of corneal ectasia. The authors found that all eyes with corneal ectasia referred during the study could be fitted with the PROSE device. Of eyes for which PROSE devices were dispensed, there was a mean habitual corrected visual acuity of 0.56 ±0.44 logMAR (20/70) and a BCVA with the device of 0.09 ±0.15 logMAR (20/25; P < .001). The study had significant findings related to penetrating keratoplasty, including patients with prior corneal transplantation in at least one eye achieved similar results of improvement in visual acuity and functioning as non-transplant ectatic eyes. Visual acuity in the post-keratoplasty subgroup was similar, with mean habitual corrected visual acuity of 0.65 ±0.53 logMAR (20/100) and mean BCVA with the device of 0.10 ±0.17 logMAR (20/25; P < .001).
Similarly, DeLoss et al4 set out to compare the ocular characteristics and visual outcomes of eyes with corneal ectasia that were fitted with the PROSE lens. The authors concluded that eyes with advanced corneal ectasia can be successfully fitted with PROSE, demonstrating the visual acuity outcomes for severe keratoconus to be better and achievement of visual acuity more rapid compared with keratoplasty. Of eyes in the most severe category of ectasia fitted with PROSE, 100% achieved 20/40 vision, and 80% achieved 20/25 or better. More eyes with the most severe form of ectasia by the study criteria achieved 20/25 visual acuity after PROSE than after keratoplasty (P = .003). At 1-year follow-up in the PROSE cohort, Snellen acuity was 20/28 (P = .108 vs keratoplasty), improving to 20/25 with over-refraction (P = .006 vs keratoplasty). This was despite the fact that eyes in the keratoplasty group had more severe ectasia than eyes in the PROSE group (P = 0.38).
Scleral lenses utilize their large fluid reservoir to tackle myopia, irregular astigmatism, and corneal scarring—all important considerations for optical correction in the treatment of ectasia.5-7 The lens also removes many of the potential surgical-associated complications with keratoplasty and potentially difficult postoperative period. Using this evidence, PROSE lens evaluation, for those who can afford it, can delay the need for transplantation in patients with advanced corneal ectasia while providing great vision.
PROSE FOR SEVERE DED, STEVENS-JOHNSON SYNDROME, AND GRAFT-VERSUS-HOST DISEASE
Ocular surface rehabilitation remains a challenge in patients with severe ocular surface disorders, such as ocular cicatricial pemphigoid, Stevens-Johnson syndrome (SJS), and extreme DED.8 In these cases, scleral contact lenses are well suited to provide relief.
SJS, a form of toxic epidermal necrolysis (TEN), is an acute, potentially life-threatening, blistering disease of the skin that can affect the eyes if not treated promptly.8 Drugs are the most common etiologic factor. A multitude of conservative treatments have been used in the management of chronic sequelae, including lubrication, topical steroids, cyclosporine, autologous tears, and amniotic membrane transplantation; however, results have been found to be variable,9 and there is no consensus on best management.10
Papakostas et al11 reported on PROSE treatment in patients with OSD related to SJS/TEN. Based on a standardized dry eye questionnaire, the researchers found that there was a significant improvement in the visual function without the risks and uncertain outcomes of surgery, the cosmetic and visual limitations of tarsorrhaphy, and the difficulties in preparation and storage of autologous serum tears. Objective measurements confirmed that the median visual acuity at the initial study visit was 20/60 (range, 20/400–20/25), and the visual acuity at the end of the lens fitting customization was 20/25 (range, 20/200–20/20; P < .001). This improvement was maintained over the median 16-month follow-up period. Other studies by Tougeron-Brousseau et al12 and Heur et al13 reported similar findings.
Similarly, management of severe DED associated with chronic graft-versus-host-disease (cGvHD) is difficult given the severity of dry eye and associated keratoconjunctival inflammation. Jacobs and Rosenthal14 showed that PROSE mitigates symptoms and improves the quality of life in these patients. The authors found that PROSE wear specifically resulted in improvement in pain (52%) and photophobia (63%). More than two-thirds (73%) of patients reported the highest improvement level for quality of life. The study did not compare objective visual acuity outcomes.
Other studies have looked into the success of limbal stem cell transplantation15,16 and the Boston keratoprosthesis17; however, these surgical interventions have demonstrated multiple added comorbidities without evidence of improved results over scleral lenses.
Dimit et al18 reviewed 51 charts of patients fitted with the PROSE lens and found that the most common reason for fitting (at nearly 50% in their practice) was relief of moderate to severe DED from a variety of causes. The DED group demonstrated a 17 letter (logMAR) improvement in BCVA (P = .091). Rosenthal and Croteau1conversely found that vision improvement (501 eyes) was a more prevalent reason for fitting than management of severe OSD (374 eyes), but they did not look into visual outcomes.
PROSE IN OTHER OCULAR DISEASES
The possible utility of scleral lenses can seem endless, and outcomes for multiple causes of dry eye syndrome all seem similarly favorable.19 Multiple studies have demonstrated success with the use of PROSE in persistent epithelial defects,1,20,21 finding that the lens constitutes an effective and safe option for refractory cases. Exposure keratopathy has also been studied in several reports with favorable results.22,23 There is even a case report on the successful use of scleral lenses in a patient with Graves’ ophthalmopathy who had failed conservative treatments24 and a case series on use in Salzmann nodular degeneration noting improvements in visual acuity and symptoms.25
COST
Shepard et al26 calculated the cost-effectiveness of the PROSE treatment in patients with corneal ectasia, irregular astigmatism, and OSD. The authors concluded that, according to their cost benefit analysis, the overall benefit-cost ratio was highly favorable. In 2009, the average cost of each fitted patient was $12,300 (approximately half for clinical services and half to produce the prosthesis) for a patient fitted with two lenses.27 This decreased to approximately $8,000 for a single prosthesis. For comparison, according to the actuarial and consulting firm Milliman, in 2011 the typical cost for a corneal transplant was $24,400.28
POTENTIAL COMPLICATIONS
A 1995 review of scleral lens wearers (not specific to PROSE) found that the most common complications include corneal neovascularization (13.3%), corneal abrasion (3.1%) and giant papillary conjunctivitis (1.7%)29; however, these are likely overstated today given improved lens design and fitting procedures.30 Infectious keratitis associated with scleral lens use is rare, but cases have been reported.31 In retrospective reviews of the PROSE lens, ophthalmic complications were uncommon. The most common reasons for discontinuation of wear included discomfort, limited improvement, difficulty of insertion/removal, and ophthalmic complications including redness.2
CONCLUSION
Use of scleral contact lenses, especially the PROSE lens with its custom-designed vault, is an effective treatment option for a variety of severe corneal conditions. A multitude of studies have demonstrated a level of efficacy, cost effectiveness, and success that is comparable to more invasive procedures but without significant associated risk.
1. Rosenthal P, Croteau A. Fluid-ventilated, gas-permeable scleral contact lens is an effective option for managing severe ocular surface disease and many corneal disorders that would otherwise require penetrating keratoplasty. Eye Contact Lens. 2005;31:130-134.
2. Agranat JS, Kitos NR, Jacobs DS. Prosthetic replacement of the ocular surface ecosystem: impact at 5 years. Br J Ophthalmol. 2016;100(9):1171-1175.
3. Baran I, Bradley JA, Alipour F, et al. PROSE treatment of corneal ectasia. Cont Lens Anterior Eye. 2012;35:222-227.
4. DeLoss KS, Fatteh NH, Hood CT. Prosthetic Replacement of the Ocular Surface Ecosystem (PROSE) scleral device compared to keratoplasty for the treatment of corneal ectasia. Am J Ophthalmol. 2014;158:974-982.
5. Schornack MM, Patel SV. Scleral lenses in the management of keratoconus. Eye Contact Lens. 2010;36(1):39-44.
6. Lee JC, Chiu GB, Bach D, Bababeygy SR, Irvine J, Heur M. Functional and visual improvement with prosthetic replacement of the ocular surface ecosystem scleral lenses for irregular corneas. Cornea. 2013;32(12):1540-1543.
7. Gumus K, Gire A, Pflugfelder SC. The impact of the Boston ocular surface prosthesis on wavefront higher-order aberrations. Am J Ophthalmol. 2011;151(4):682-690.e682.
8. Power WJ, Ghoraishi M, Merayo-Lloves J, et al. Analysis of the acute ophthalmic manifestations of the erythema multiforme/Stevens-Johnson syndrome/toxic epidermal necrolysis disease spectrum. Ophthalmology. 1995;102:1669-1676.
9. Iyer G, Srinivasan B, Agarwal S, et al. Comprehensive approach to ocular consequences of Stevens Johnson Syndrome - the aftermath of a systemic condition. Graefes Arch Clin Exp Ophthalmol. 2014;252:457-467.
10. Ciralsky JB, Sippel KC, Gregory DG. Current ophthalmologic treatment strategies for acute and chronic Stevens-Johnson syndrome and toxic epidermal necrolysis. Curr Opin Ophthalmol. 2013;24:321-328.
11. Papakostas TD, Le HG, Chodosh J, et al. Ophthalmology. 2015;122(2):248-253.
12. Tougeron-Brousseau B, Delcampe A, Gueudry J, et al. Vision- related function after scleral lens fitting in ocular complications of Stevens-Johnson syndrome and toxic epidermal necrolysis. Am J Ophthalmol. 2009;148:852-859.
13. Heur M, Bach D, Theophanous C, Chiu GB. Prosthetic replacement of the ocular surface ecosystem scleral lens therapy for patients with ocular symptoms of chronic Stevens- Johnson syndrome. Am J Ophthalmol. 2014;158:49-54.
14. Jacobs DS, Rosenthal P. Boston scleral lens prosthetic device for treatment of severe dry eye in chronic graft-versus-host disease. Cornea. 2007;26:1195-1199.
15. Sotozono C, Inatomi T, Nakamura T, et al. Visual improvement after cultivated oral mucosal epithelial transplantation. Ophthalmology. 2013;120:193-200.
16. Biber JM, Skeens HM, Neff KD, et al. The Cincinnati procedure: technique and outcomes of combined living-related conjunctival limbal allografts and keratolimbal allografts in severe ocular surface failure. Cornea. 2011;30:765-771.
17. Sayegh RR, Ang LP, Foster CS et al. The Boston keratoprosthesis in Stevens-Johnson syndrome. Am J Ophthalmol. 2008;145:438-444.
18. Dimit R, Gire A, Pflugfelder SC, et al. Patient ocular conditions and clinical outcomes using a PROSE scleral device. Cont Lens Anterior Eye. 2013;36(4):159-163.
19. Grey F, Carley F, Biswas S, Tromans C. Scleral contact lens management of bilateral exposure and neurotrophic keratopathy. Cont Lens Anterior Eye. 2012;35:288-291.
20. Ciralsky JB, Chapman KO, Rosenblatt MI, et al. Treatment of refractory persistent corneal epithelial defects: a standardized approach using continuous wear PROSE therapy. Ocul Immunol Inflamm. 2015;23(3):219-224.
21. Lim P, Ridges R, Jacobs DS, et al. Treatment of persistent corneal epithelial defect with overnight wear of a prosthetic device for the ocular surface. Am J Ophthalmol. 2013;156(6):1095-1101.
22. Weyns M, Koppen C, Tassignon MJ. Scleral contact lenses as an alternative to tarsorrhaphy for the long-term management of combined exposure and neurotrophic keratopathy. Cornea. 2013;32:359-361.
23. Gire A, Kwok A, Marx DP. PROSE treatment for lagophthalmos and exposure keratopathy. Ophthal Plast Reconstr Surg. 2013;29:e38-e40.
24. Harthan JS. Therapeutic use of mini-scleral lenses in a patient with Graves ophthalmopathy. J Optom. 2014;7:62-66.
25. Chiu GB, Bach D, Theophanous C, Heur M. Prosthetic replacement of the & ocular surface ecosystem (PROSE) scleral lens for Salzmann’s nodular degeneration. Saudi J Ophthalmol. 2014;28:203-206.
26. Shepard DS, Razavi M, Stason WB, et al. Economic appraisal of the Boston Ocular Surface Prosthesis. Am J Ophthalmol. 2009;148:860-868.
27. Ament JD, Stryjewski TP, Ciolino JB, et al. Cost-effectiveness of the Boston keratoprosthesis. Am J Ophthalmol. 2010;149:221-228.
28. Bentley TS, Hanson SG. 2011 US Organ and Tissue Transplant Cost Estimates and Discussion. https://us.milliman.com/uploadedFiles/insight/research/health-rr/2011-usorgan-tissue.pdf. Accessed November 28, 2016.
29. Tan DT, Pullum KW, Buckley RJ. Medical applications of scleral contact lenses. A restrospective analysis of 343 cases. Cornea. 1995;14:121-129.
30. Caroline PJ, Andre MP. Conjunctival prolapse, hooding, chalasis. Contact Lens Spectrum. 2012;27:56.
31. Fernandes M, Sharma S. Polymicrobial and microsporidial keratitis in a patient using Boston scleral contact lens for Sjogren’s syndrome and ocular cicatricial pemphigoid. Cont Lens Anterior Eye. 2013;36:95-97.




