The surgical management of glaucoma continues to be an attractive option for treatment, especially as an alternative option to medical therapy that may be associated with poor compliance.1 The desire to do so is especially manifest among those with ocular surface concerns or who experience side effects from their drops.2-4 Advancements in the surgical category provide surgeons with more options than ever before that are safe and minimally invasive, especially among procedures meeting the definition of microinvasive glaucoma surgery (MIGS).5 Yet, one limitation of several MIGS options is that they are intended to treat focally. Ab interno canaloplasty (ABiC; Ellex), however, is designed to repair several physiologic mechanisms in the natural aqueous outflow pathway. There is every reason to believe that a holistic, restorative MIGS approach such as this provides maximal long-term benefit while preserving future options (should they become necessary) and avoiding inducing iatrogenic trauma to the ocular tissue.
—Mahmoud A. Khaimi, MD
What is ABiC? How does it differ from other MIGS procedures?
Mark J. Gallardo, MD: ABiC is a MIGS procedure in which Schlemm canal is accessed, cannulated, and viscodilated from inside the eye. Minimally invasive, it requires only a sideport incision and a clear corneal incision—and if it is combined with cataract surgery, no additional corneal wounds are necessary. Yet, unlike other MIGS procedures, which address only focal areas in the outflow mechanism (ie, bypassing trabecular meshwork by means of a stent), ABiC restores the physiologic function of the entire drainage system. This is a concept that may be underdiscussed with respect to MIGS procedures: There is no diagnostic mechanism to understand where outflow obstruction is occurring, and so even the most perfectly placed stent bears the risk of missing or suboptimally treating the blockage. With ABiC, on the other hand, we are treating the trabecular meshwork by separating the lamella, creating microperforations in the wall of Schlemm canal, and, with viscodilation, restoring canal architecture while releasing adhesions in the collector channels. In short, the procedure helps rejuvenate the entire aqueous outflow pathway for 360°, from the trabecular meshwork out to scleral plexus.
Mahmoud A. Khaimi, MD: Unlike other MIGS procedures, with ABiC there is no stent placement, which carries a theoretical risk of erosion (an event that occurred rarely in the iStent premarket clinical trials6). In addition, there is no ablation or removal of angle tissue, thereby reducing the risk of hyphema. If I am performing simultaneous cataract surgery, I am able to use the same temporal clear corneal incision to introduce the probe and access the angle. Then, using a 27-gauge needle, a goniotomy is performed from a radial site 180° from the incision to create an entry for the probe. Because these maneuvers are performed from inside the eye, there is no deep sclerotomy, no conjunctival manipulation, no Descemet window, and no need for suture tensioning to maintain dilation—instead, viscodilation is performed while the probe is extracted, which is sufficient to maintain long-term dilation.
What is iTrack and why is important for ABiC?
Dr. Khaimi: The iTrack System (Ellex), which is used to catheterize, access, and viscodilate Schlemm canal during the ABiC procedure, has several key design features that make it fundamental to the success of the procedure. First, because it is flexible, it will not forge a new pathway in Schlemm canal if it meets with an obstruction; the operator can simply pull back on the microcatheter, reposition it, and continue the procedure or simply advance the microcatheter in the opposite direction. Thus, the risk of unintentional rupture is mitigated. Second, the microcatheter has a lighted beacon on its tip, which aids in visualization as it is advanced for 360° and hence provides peace of mind that the intended target area is being treated appropriately.
Dr. Gallardo: During the ABiC procedure, the microcatheter is threaded through Schlemm canal with micro-forceps, providing real-time tactile feedback of the health and patency of the canal (Figure). Next, as the microcatheter is withdrawn, the precisely controlled delivery of Healon/Healon GV separates the compressed tissue planes of the trabecular meshwork, and also triggers the withdrawal of any herniated inner wall tissue from the collector channels. One of the standout features of this product is its illuminated tip, which allows you to continually monitor its location during canal circumnavigation. Further, a small gauge support wire, which provides both strength and agility, allows you to bypass “tight” areas within the canal and, coupled with focal viscodilation, makes it possible to pass the microcatheter beyond adhesions or other canal abnormalities.
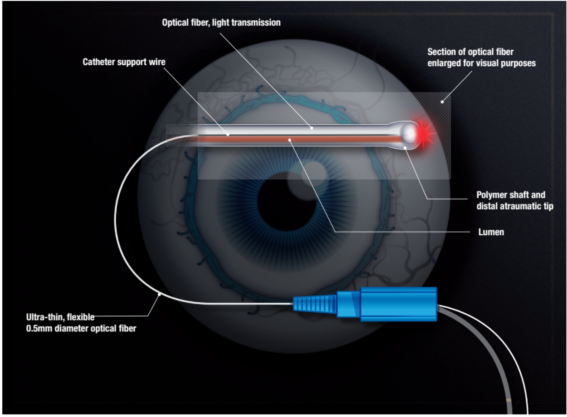
Image courtesy of Ellex
FIGURE. The microcatheter is threaded through Schlemm canal with micro-forceps, providing real-time tactile feedback of the health and patency of the canal.
What is the learning curve with ABiC and what surgical steps will help ensure success?
Dr. Khaimi: The learning curve with ABiC is relatively low, especially for any surgeon with experience performing angle-based surgery. The steps of the procedure are sequential, so they are not that difficult to learn, nor are they overly confusing.
When performed as a stand-alone procedure or combined with cataract surgery, Schlemm canal is accessed via a 1.8-mm, temporal, clear corneal incision (the same incision used for cataract surgery can be used). One should be careful to ensure the wound is not too far posterior, where there is risk of breaching the conjunctival vessels, which, in turn, heightens the risk for bleeding. Because a goniotomy is later used to access Schlemm canal, maintaining a clear surgical field devoid of blood aids in visualization.
Next, an ophthalmic viscosurgical device is injected into the anterior chamber to maintain stability, after which the microcatheter probe tip is introduced to the anterior chamber through the 1.0-mm corneal incision. A goniotomy incision is made at a site 180° from the clear corneal wound (I use a 27-gauge, 0.5-inch needle with bevel facing up for this step, minimizing the trauma to the tissue). The tip of the probe is grasped using intraocular forceps (introduced through a sideport) and gently guided into Schlemm canal and carefully advanced for 360°—the lighted tip on the end of the probe guides visualization of this step. The probe is then retracted along the same path while viscodilation is performed.
What outcomes can be expected with ABiC?
Drs. Gallardo and Khaimi: We recently completed a review of 228 eyes that underwent treatment with ABiC (unpublished data). Overall, average IOP reduction was 30% and there was a 50% reduction in the number of medications postoperatively. Mean IOP was lowered from 19.0 ±6.5 mm Hg at baseline to 14.7 ±3.9 mm Hg, 14.5 ±3.8 mm Hg, and 13.3 ±2.0 mm Hg, respectively, at 3, 6, and 12 months after treatment. Within this population 130 patients underwent combined ABiC and phacoemulsification; in this cohort, mean preoperative IOP was 17.1 ±5.0 mm Hg, which was reduced to 13.1 ±2.1 mm Hg at 12 months (n = 34), for an overall reduction in mean IOP of 23.39%. The number of medications was reduced by 50% from 2.0 ±1.0 to 1.0 ±1.0 by 12 months postoperatively. Results were equally as substantial among eyes undergoing a stand-alone procedure (n = 98), with a reduction in mean IOP from 21.5 ±7.4 mm Hg preoperatively to 13.6 ±1.9 mm Hg at 12 months (n = 14). The mean number of medications used was reduced 66.66% from 3.0 ±1.0 preoperatively to 1.0. ±1.0.
1. Okeke CO, Quigley HA, Jampel HD, et al. Adherence with topical glaucoma medication monitored electronically the Travatan Dosing Aid study. Ophthalmology. 2009;116(2):191-199.
2. Kramer TR, Noecker RJ. Comparison of the morphologic changes after selective laser trabeculoplasty and argon laser trabeculoplasty in human eye bank eyes. Ophthalmology. 2001;108:773-779.
3. Osborne SA, Montgomery DM, Morris D, et al. Alphagan allergy may increase the propensity for multiple eye-drop allergy. Eye. 2005;19:129–137.
4. Nelson WL, Fraunfelder FT, Sills JM, et al. Adverse respiratory and cardiovascular events attributed to timolol ophthalmic solution, 1978–1985. Am J Ophthalmol. 1986;102:606–611.
5. Brandão LM, Grieshaber MC. Update on minimally invasive glaucoma surgery (MIGS) and new implants. J Ophthalmol. 2013:705915.
6. iStent Package Insert. http://www.accessdata.fda.gov/cdrh_docs/pdf8/p080030c.pdf. Accessed January 31, 2017.
7. Ellex iScience, Inc. Data on File.
Mark J. Gallardo, MD, is in private practice at El Paso Eye Surgeons in Texas. Dr. Gallardo serves as a consultant to Ellex and served as a clinical investigator for the ABiC procedure.
Mahmoud A. Khaimi, MD, is clinical associate professor at the Dean McGee Eye Institute,University of Oklahoma, Oklahoma City. Dr. Khaimi serves as a consultant to Ellex and served as a clinical investigator for the ABiC procedure.


