Editorially independent content supported with advertising from


Sooner or later, most trabeculectomies fail, usually from episcleral and subconjunctival scarring. The question of what to do next has never been more complicated. In the past, bleb needling, repeat trabeculectomy, and a tube shunt were the primary choices. Now, surgeons have a host of options to consider.
TRADITIONAL APPROACHES
When considering the traditional options, the patient’s history and bleb appearance are key determinants of the next step. Earlier failure with aggressive subconjunctival scarring makes bleb needling and repeat trabeculectomy less attractive, given concerns about similar results after either approach. Late failure, with focal scarring such as so-called ring-of-steel fibrosis around a scleral flap, suggest that bleb needling may provide improved odds of long-term success with a (usually) short and simple intervention (Figure 1).
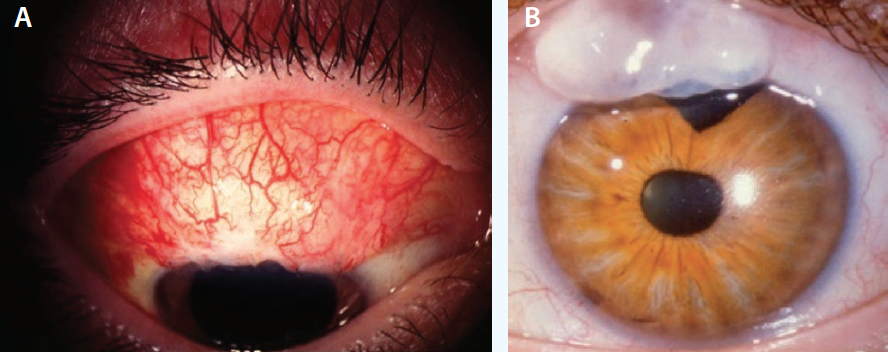
Figure 1. Thick, scarred conjunctiva suggests a lower rate of success with bleb needling (A). Thin, avascular tissue with a ring of steel may yield a successful outcome in terms of pressure, but in this case, the potential for dysesthesia, leaks, and infection may lead to consideration of a more extensive surgical revision (B).
The Tube Versus Trabeculectomy (TVT) study showed greater success at 3 years with tube shunts in patients with a history of glaucoma surgery, including failed trabeculectomies,1 but two considerations still lead many surgeons to try a repeat trabeculectomy first. One is the greater likelihood of achieving very low IOPs without medication after a trabeculectomy, at least initially, than after a tube shunt. The other is that, in younger patients, performing the trabeculectomy first may buy 3 to 5 years and keep one more option open for the future (Figure 2).1
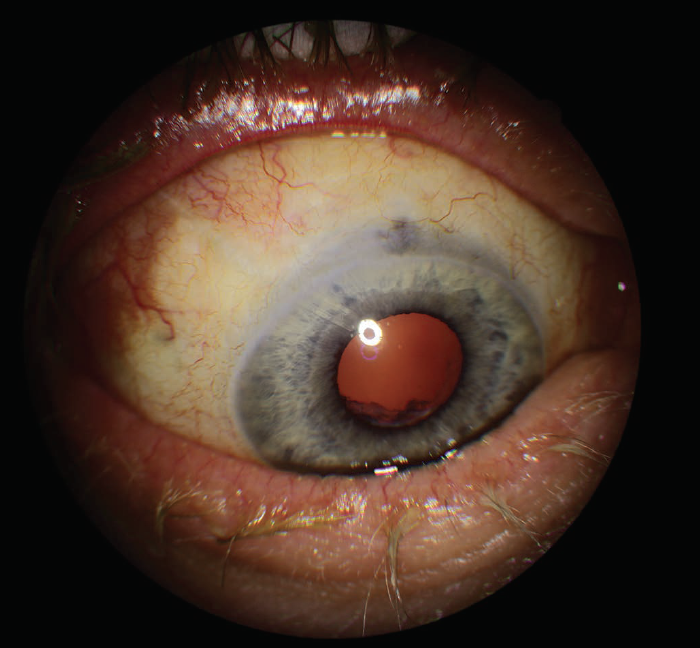
Figure 2. The patient had extensive scarring and a completely flat filtering bleb but has done well after tube shunt surgery.
NEW AVENUES
In patients with prolonged trabeculectomy success, the conventional outflow pathway has presumably been underused for some time, especially on top of the original dysfunction that led to trabeculectomy. This might suggest that trabecular surgeries such as trabeculotomy, goniotomy, or trabecular microbypass would be less likely to prove effective in the short and long term. Despite these concerns, a recent report of ab interno trabeculotomy showed significant success at 24 months after failed trabeculectomy, with an average IOP reduction of almost 8 mm Hg.2 In a small study of 11 patients with failed filtering procedures, four had substantial (> 6 mm Hg) IOP lowering after the injection of multiple trabecular microbypass stents.3
Supraciliary devices would seem appealing for some of these patients after trabeculectomy failure, because these implants function through a separate outflow pathway. Reports to date suggest much lower surgical risks with supraciliary microstents than trabeculectomy and tube shunts.4,5 The published research on supraciliary devices after failed trabeculectomy is limited, although a trial of two trabecular microbypass stents, one supraciliary microstent, and travoprost reported high and prolonged levels of success in a prospective study of Armenian patients with a history of failed trabeculectomy.6 A case report of two trabecular microbypass stents after failed combined cataract surgery and trabeculectomy described an 11-point drop in IOP for 2 years.7 (Trabecular microbypass stents and supraciliary microstents are not FDA approved without concomitant cataract surgery.)
The ab interno gel stent has been studied in patients with a history of failed filtration procedures as part of the device’s phase 3 trials, and the technology gained FDA approval in 2016. In a study of 65 subjects, of whom 85% had failed prior glaucoma procedures, 76% of eyes achieved more than a 20% reduction in IOP 12 months after the ab interno implantation of a gelatin stent with mitomycin C.8 Studies are lacking on how the long-term success of this device will compare to that of tube shunts after failed trabeculectomy, as was tested in the TVT study, but the gel stent seems to have a more favorable side effect profile than trabeculectomy.
Cyclophotocoagulation of the ciliary body has become of greater interest to many practitioners since the introduction of the slow-burn technique (3-4 seconds at lower wattage) and the more recent micropulse option. Some (but not all) reports of micropulse cyclophotocoagulation suggest a more benign side effect profile than a traditional transscleral cyclophotocoagulation setting, perhaps especially with milder treatments earlier in the disease course.9,10 Recent research on refractory glaucoma shows good efficacy but some risk of serious complications, including vision loss.11
DECISIONS, DECISIONS
Currently, there is an incomplete, complicated, and evolving data set to guide clinical decision making in patients who require surgical intervention for IOP control after trabeculectomy has failed. For those in whom trabeculectomy was successful long term and who have favorable conjunctival features, bleb needling with mitomycin C can be an effective option, especially if a low target pressure with less medication is needed. Alternatively, for these patients in whom trabeculectomy has been effective, the new gel stent may be a safer option than repeat trabeculectomy. For patients who can tolerate medications and who are willing to trade some short- and long-term success for greater safety and a quicker recovery, a newer alternative such as trabeculotomy or a supraciliary microstent may be a good option, although FDA and insurance considerations for standalone supraciliary devices may present issues. For elderly patients with more advanced glaucoma who can tolerate medications, a tube shunt remains an excellent option after a failed trabeculectomy and offers good long-term success rates.
1. Gedde SJ, Schiffman JC, Feuer WJ, et al; Tube Versus Trabeculectomy Study Group. Three-year follow-up of the Tube Versus Trabeculectomy study. Am J Ophthalmol. 2009;148(5):670-684.
2. Grover DS, Godfrey DG, Smith O, et al. Outcomes of gonioscopy-assisted transluminal trabeculotomy (GATT) in eyes with prior incisional glaucoma surgery. J Glaucoma. 2017;26(1):41-45.
3. Sandhu S, Rayat J, Benson M, et al. Multiple iStent implantation following glaucoma filtering procedure(s) in patients with refractory glaucoma. Poster presented at: Annual Meeting of the American Glaucoma Society; March 2, 2017; Coronado, CA.
4. García-Feijoo J, Rau M, Grisanti S, et al. Supraciliary micro-stent implantation for open-angle glaucoma failing topical therapy: 1-year results of a multicenter study. Am J Ophthalmol. 2015;159(6):1075-1081.
5. Figus M, Posarelli C, Passani A, et al. The supraciliary space as a suitable pathway for glaucoma surgery: ho-hum or home run? Surv Ophthalmol. 2017;pii:S0039-6257(16)30091-1.
6. Saheb H, Katz LJ, Myers J, Voskanyan L. Long-term outcomes of post-trabeculectomy refractory glaucoma treated with 2 trabecular micro-bypass stents, 1 suprachoroidal stent, and a postoperative prostaglandin. Poster presented at: Annual Meeting of the American Glaucoma Society; March 2, 2017; Coronado, CA.
7. Roelofs K, Arora S, Dorey MW. Implantation of 2 trabecular microbypass stents in a patient with primary open-angle glaucoma refractory to previous glaucoma-filtering surgeries. J Cataract Refract Surg. 2014;40(8):1322-1324.
8. Grover D, Flynn W, Bashford K, et al. Multicenter, single-arm, open-label study of the intraocular pressure-lowering effect and complications of an ab interno implanted gelatin stent in refractory glaucoma: twelve-month results. Poster presented at: Annual Meeting of the American Glaucoma Society; March 2, 2017; Coronado, CA.
9. Amoozgar B, Phan EN, Lin SC, Han Y. Update on ciliary body laser procedures. Curr Opin Ophthalmol. 2017;28(2):181-186.
10. Emanuel ME, Grover DS, Fellman RL, et al. Micropulse cyclophotocoagulation: initial results in refractory glaucoma. J Glaucoma. 2017;26(8):726-729.
11. Emanuel ME, Grover DS, Fellman RL, et al. Micropulse cyclophotocoagulation: initial results in refractory glaucoma. J Glaucoma. 2017;26(8):726-729.



