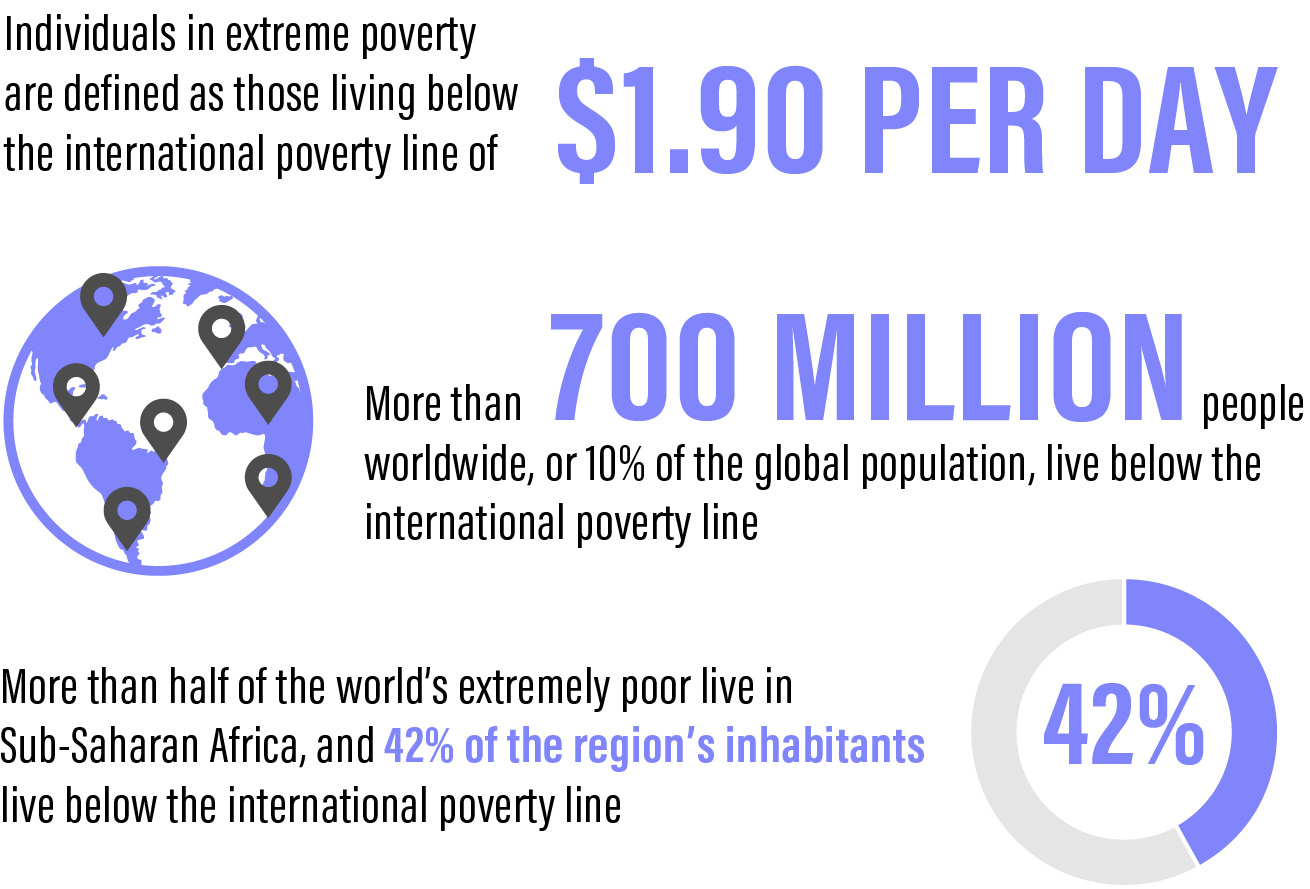
In 2015, the World Bank reset the international poverty line to $1.90 per day. This figure represents a picture of the costs of basic food, clothing, and shelter. Individuals who live on less than this amount are considered to be living in extreme poverty. According to the most recent estimates, this includes more than 702 million people worldwide, or 10% of the global population.1
The percentage of individuals living below the international poverty line has decreased significantly since 1990 (36%); however, a disparity in the distribution of the world’s poor remains. For example, the number of people living in extreme poverty has decreased in most countries within East and Southeast Asia, but it continues to increase in Sub-Saharan Africa. This region is home to more than half of the world’s extremely poor population, and 42% of its inhabitants currently live below the international poverty line.2
The international poverty line is determined by an individual’s purchasing power to fulfill his or her daily needs. Although most of the daily $1.90 is allocated to food, the food that it affords might be low in quality and nutritional value. Shelter, education, and health care must be covered by this amount as well. When an individual is forced to choose between health care and other necessities such as food or housing, health care often takes a back seat.
CAUSES OF GLOBAL POVERTY
A multitude of diverse factors contribute to global poverty, and the lines between cause and effect are often blurred. Historically, the poorest nations in the world are former colonies, where resources were systematically removed and conditions were created to prevent people from accessing capital, land, and education. War and political upheaval continue to strain the stability, safety, and security of these regions, thereby preventing inhabitants from harnessing basic resources such as clean water and nutritious food. In addition to a lack of stable infrastructure, conflict zones such as these provide little to no access to formal education or employment.
Additionally, in some low-income areas, recurrent catastrophic natural disasters pose significant obstacles to eradicating poverty. Flooding in Bangladesh, drought in Africa, and earthquakes and hurricanes in Haiti are just some examples of the destructive natural disasters that affect impoverished regions.
POVERTY AND HEALTH
Poverty and poor health are interwoven.3 Poverty is a major cause of poor health as well as a barrier to health care access. Conversely, poor health is a major cause of poverty. The costs associated with consultations, medications, and tests—as well as transportation and missed work—can make accessing health care burdensome for those living in poverty. These inequalities further lead to disparities in education, literacy, health, nutrition, sanitation, and mortality.4 Such disparities result in a lack of health equity.
Health equity occurs when every individual has a fair and just opportunity to be healthy. Its achievement requires the removal of several obstacles, including discrimination and socioeconomic barriers to education, employment, housing, and food. Health disparity is, in actuality, health inequality, and it results in differences in health between various groups.
PICTURES OF GLOBAL POVERTY
The concept of global poverty may, for some, conjure up images of malnourished children living on a roadside or multigenerational families living in one room and sharing a bowl of porridge. However, poverty presents in many ways. Even in the United States, one of the wealthiest nations in the world, examples of health disparities can be seen. In my under- and uninsured patient population in Dayton, Ohio, I frequently see patients who must choose between undergoing vision-saving treatments and paying their monthly rent.
Health inequality can look like Mr. Hendrix, an elderly underinsured patient who decided it was so important for him to get his glaucoma drops that he resorted to eating canned cat food in order to afford them. When the technician asked him why he didn’t call our practice once he found out his copay charge, she heartbreakingly realized he hadn’t considered that we could change his class of medication or find him a drug assistance program; he assumed his doctor knew best and that he had no other option.
Health inequality can look like Mrs. Noor, a refugee who sleeps with the lights on, flinches at loud noises, has lost family members in war-torn Syria, and refuses to attend a health and wellness workshop because she believes doing so implies she has a mental disease. Or health inequality can look like the people of Vanua Levu, the second largest island in Fiji, where, despite a population of more than 135,000, not a single ophthalmologist exists. Here, all I can offer as a visiting ophthalmologist is 40 cataract cases per week, leaving the remaining patients untreated until the next group of volunteers comes through.
ENDING GLOBAL POVERTY
The World Bank and the United Nations have set a lofty goal of ending extreme poverty by 2030.1 With only a decade left, it is unclear whether this can be achieved.
There is no single solution to ending global poverty. Reaching this goal requires cross-collaboration between governments and communities. By working with nonprofits and governmental aid organizations to increase food security, promote child survival, strengthen health systems, and improve education, we can reach this goal.5 Innovations in economic development, health care access, job growth, and pay equity all contribute to inclusive economic growth and health equity.
For physicians, acquiring knowledge of the problem is the first step. The second step is to become involved in advocacy efforts. Our involvement in health care delivery and advocacy can have a significant impact on communities. Of course, making donations to reputable organizations is a step that all people can take. But, as physicians, we have the skill set to work directly with those in need and provide on-the-ground services, training, and mobilization both locally and abroad. Our local inner-city and rural communities often face socioeconomic barriers to health care that mirror what is seen in developing countries.
Globally, building self-sustaining health care systems is crucial to allow communities to develop and thrive instead of relying on one-time efforts of volunteers. One way to create a longer-term impact is to invest in the community’s economy by procuring medicine and equipment locally. Most US medical groups partner with country-specific nongovernmental organizations to provide humanitarian trips and intra-country specialty training. Skills transfer, therapeutic indications, procedure training, and community development projects are all means through which physicians can help make a difference. In addition, physician mentorship (via webinar, for example) is important for providing ongoing education of local staff.
CONCLUSION
Global poverty is a complex and multifactorial challenge, and a great deal of work must still be done to combat it. Although progress has been made, in some nations it has been slow, and in others poverty has only worsened. As 2030 nears, we must strive to identify solutions to alleviate global poverty and all of its consequences, including health inequality. When communities and governments around the world begin to treat health care as a human right and commit to improving access to health care for everyone, we will be much closer to breaking the cycle of global poverty.



