A capsular tension segment (CTS) may be used in eyes with profound zonular instability. The curved shape of the PMMA device supports approximately 90º of the capsular equator. Whereas a capsular tension ring (CTR) redistributes tension from areas of intact zonules to strengthen areas of weakened zonules, a CTS directly supports the defective area and recenters the capsular bag in eyes with significant lens subluxation.
An anterior offset fixation curl allows a CTS to sit over the anterior capsule. The curl has a central eyelet that enables fixation of the CTS–capsular bag complex to the sclera (Figure 1). Capsular support with scleral fixation is generally recommended for eyes with a large zonular defect (> 4 clock hours).
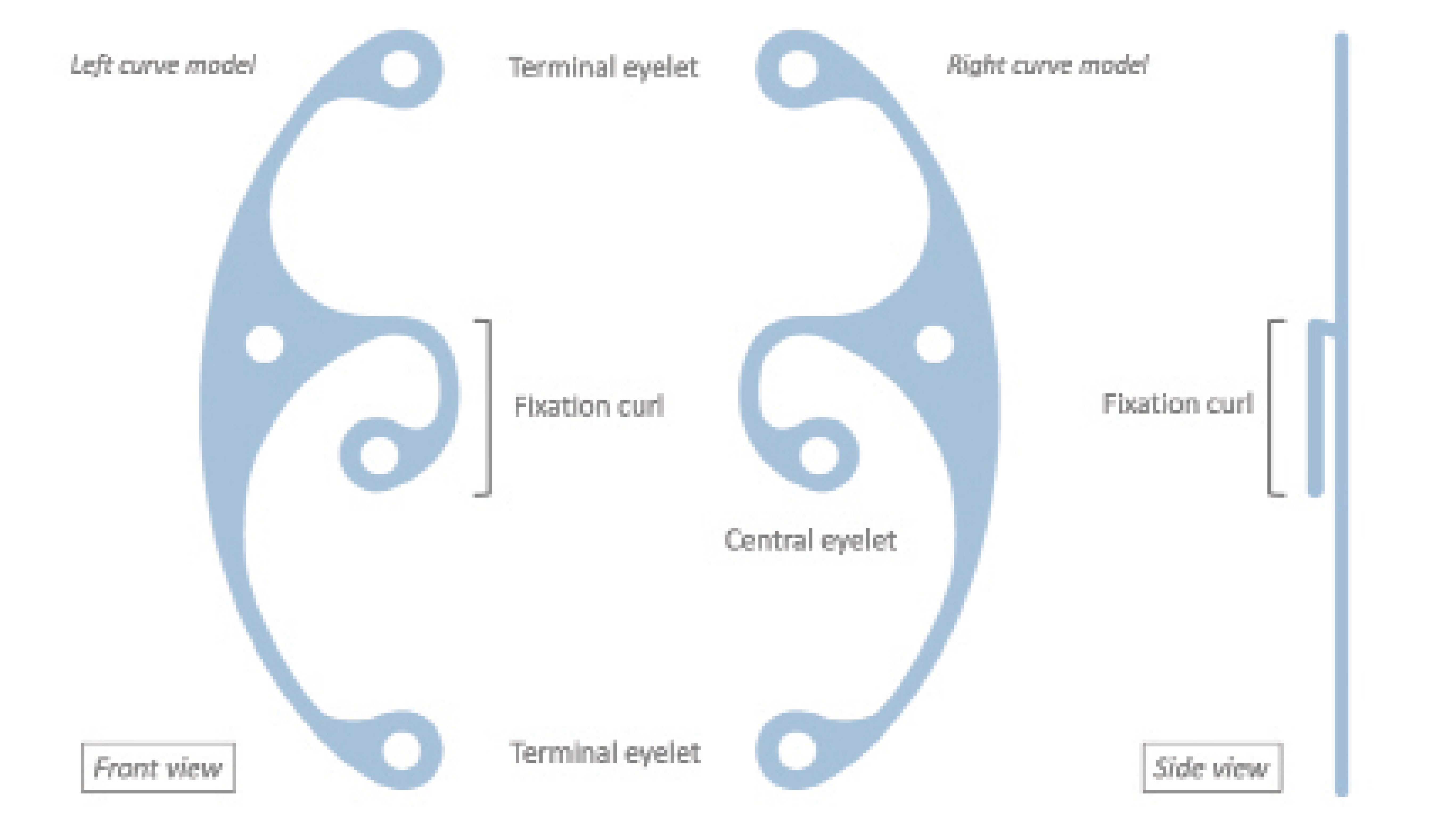
Figure 1. Components of the Aurolab CTS.
Several cases of dislocated capsular bags containing an IOL and CTR have been reported. A case series of IOL-CTR dislocations found that the complication occurred approximately 6.8 years after implantation.1 Pseudoexfoliation was the most frequently associated ocular condition. These findings suggest that the use of a CTR alone may not provide adequate long-term stability and that a scleral-fixation device such as a CTS or a modified CTR (Cionni CTR, FCI Ophthalmics) should be considered when extensive or progressive zonulopathy is present. The use of a CTR in combination with a CTS can provide support comparable to that of a Cionni CTR, but the former is technically simpler and more versatile.
The flanged Yamane technique for intrascleral IOL fixation has been widely adopted and modified in various ophthalmic procedures.2,3 Like a PMMA haptic, polypropylene suture material can be cauterized to create a flange.4,5 This article describes a technique for CTS fixation using a double-flanged 6-0 polypropylene suture. Unlike traditional techniques that involve tying a PTFE (Gore-Tex, W.L. Gore & Associates; off-label use) or polypropylene suture to the sclera, our novel method does not require opening the conjunctiva or creating a scleral flap or corneoscleral pocket. Surgical time is also reduced.
SURGICAL TECHNIQUE
A CTS can be placed before the nucleus is removed, but this timing can present difficulties, especially in eyes with anterior lens subluxation that typically have limited anterior chamber space. We prefer to use capsular hooks (with or without a CTR) to stabilize the capsular bag during phacoemulsification. If a CTR has not been implanted at some point during lens removal, the device is inserted into the capsular bag before IOL implantation. A CTS is placed as the final step. It is important to note that an intact and complete capsulorhexis is required for the procedure.
Step No. 1: Thread the polypropylene suture through the ciliary sulcus. A surgical mark is made to locate a scleral fixation point 1.5 mm posterior to the limbus over the area of zonular weakness. A dispersive OVD is injected to widen the ciliary sulcus. A 0.5-inch 27- or 30-gauge needle is bent 90º bevel up at two-thirds of its length. The bent needle—its bevel kept upward—pierces the conjunctiva and sclera at the marked site into the ciliary sulcus. A 6-0 polypropylene suture is introduced through the temporal corneal incision and fed into the lumen of the needle, which is then pulled out to externalize the polypropylene thread.
Step No. 2: Create the first flange connected to the CTS. A corneal end of the 6-0 polypropylene suture is passed from front to back through the central eyelet of the CTS. Handheld cautery is used to create a flange that is larger than the central eyelet. An excessively large flange, however, can rip the anterior capsule. In our experience, cauterizing 2 mm of the suture is sufficient to make a flange of appropriate size for our CTS of choice (Aurolab CTS), whose central eyelet has a diameter of 0.34 mm.
The length of the suture that is being cauterized and the diameter of its flange based on our study are listed in the Table (unpublished data, 2022). The study was performed using a 6-0 Prolene suture (Ethicon) and an ophthalmic cautery device (AA00, Bovie Medical).
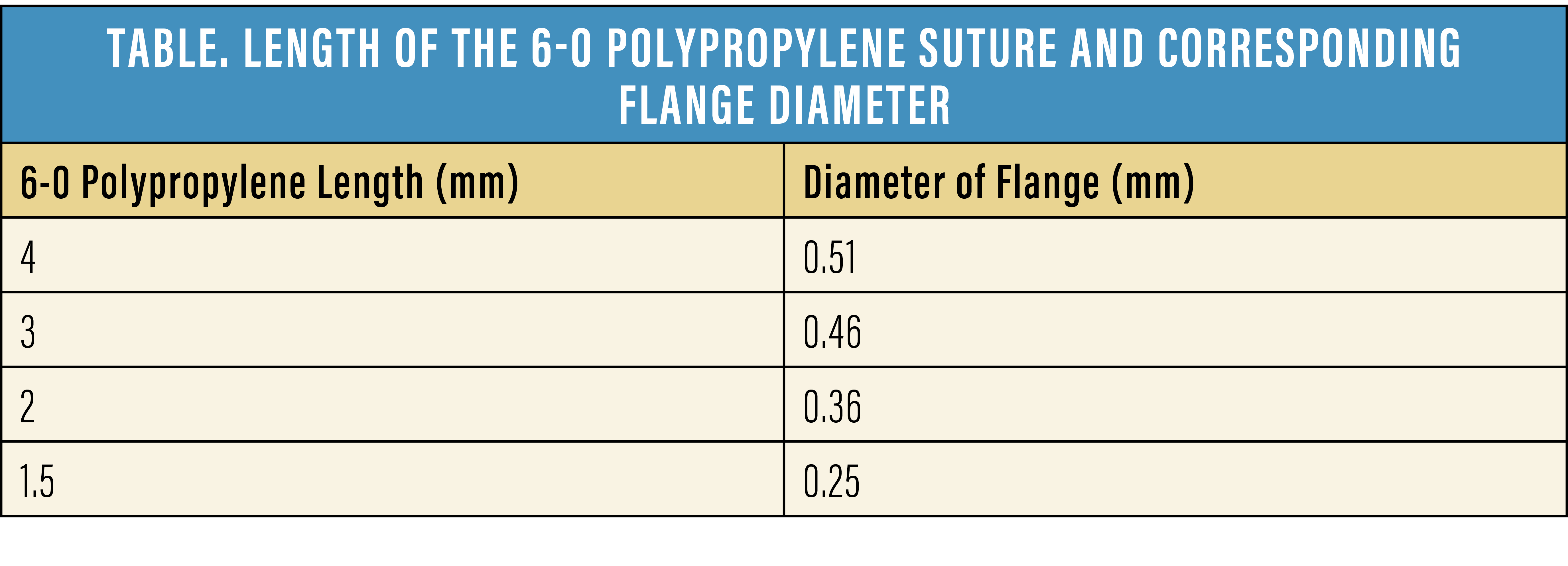
The suture must be dry, and there must be space between the cautery and suture to create a smooth dome-shaped flange.
Step No. 3: Position the CTS. The flange-CTS complex is inserted into the eye through a temporal corneal incision. The curve of the CTS should point away from the equator of the area of dialysis. The leading end of the CTS is advanced into the bag adjacent to the area of zonular weakness. The CTS is then dialed into the bag instead of directly placing it into the area of zonular weakness so that it can facilitate positioning of the fixation curl over the edge of the capsulorhexis and help prevent the CTS from flipping vertically.
Once the fixation curl is in place, the rest of the CTS can be rotated farther into the bag. The central eyelet is aligned with the scleral fixation point (Figure 2). When this maneuver is complete, the fixation curl and flange should be located above the anterior capsule. The CTS curve provides support along the capsular equator.
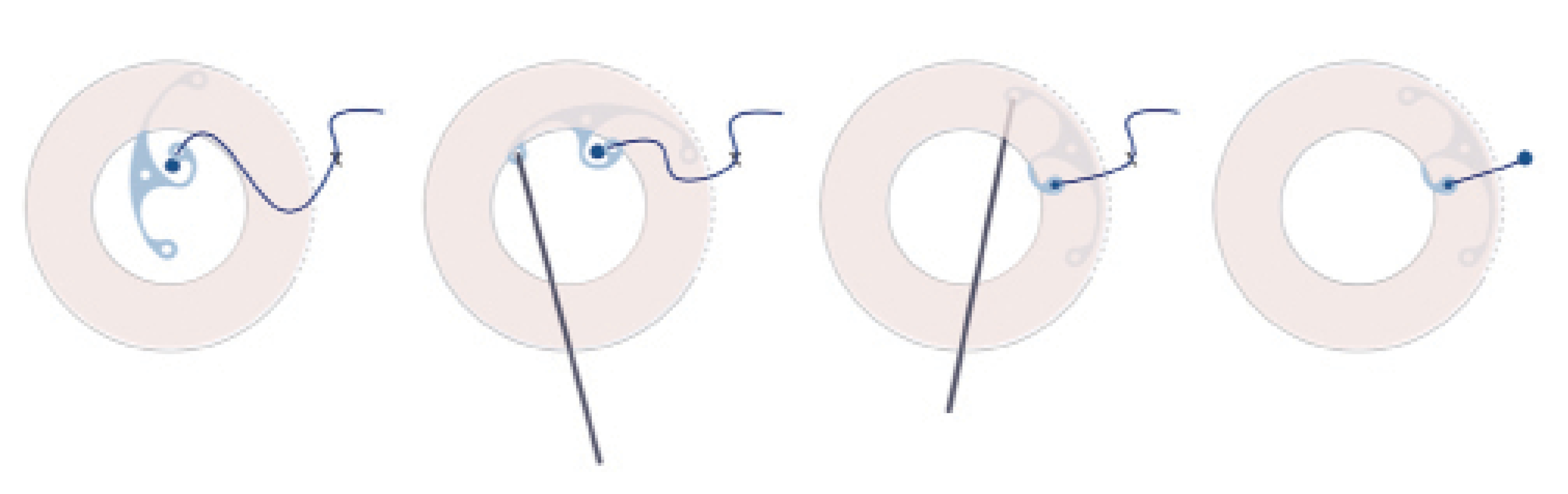
Figure 2. Steps for the placement of a CTS in the capsular bag. Dashed lines indicate the area of zonular weakness. Pink areas represent the anterior capsule. An X mark indicates the scleral fixation point. An IOL and CTR are omitted from the images.
Step No. 4: Create the external flange. Once the bag has been centered by pulling the exterior part of the suture, the outer end of the suture is tightened slightly and held proximally level with the sclera with tying forceps. The outer end of the suture is cut 2 mm above the sclera. Handheld cautery is used to create another terminal bulb. The flange is embedded in the entrance of the scleral track and covered by conjunctiva. (Scan the QR code for a demonstration of the technique.)
CONCLUSION
Scleral fixation of a CTS can improve the long-term stability of an IOL. Our technique using a double-flanged 6-0 polypropylene suture is a simpler and faster method for securing the capsular bag in eyes with extensive or progressive zonulopathy.
1. Werner L, Zaugg B, Neuhann T, Burrow M, Tetz M. In-the-bag capsular tension ring and intraocular lens subluxation or dislocation: a series of 23 cases. Ophthalmology. 2012;119(2):266-271.
2. Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124(8):1136-1142.
3. Canabrava S, Bernardino L, Batisteli T, Lopes G, Diniz-Filho A. Double-flanged-haptic and capsular tension ring or segment for sutureless fixation in zonular instability. Int Ophthalmol. 2018;38(6):2653-2662.
4. Kusaka M, Miyamoto N, Akimoto M. Repairing iridodialysis by riveting with a double-flanged polypropylene suture. J Cataract Refract Surg. 2019;45(11):1531-1534.
5. Hostovsky A, Mandelcorn M, Mandelcorn ED. Secondary posterior chamber intraocular lens fixation using flanged Prolene sutures as an alternative to an anterior chamber intraocular lens implantation. Clin Ophthalmol. 2020;14:3481-3486.






