When it comes to cataract surgery, today’s patient is generally well informed of all the IOL modalities and options available to them. As a result, they tend to have higher expectations when it comes to their postoperative refractive outcomes. Even with the most careful pre- and intraoperative measurements, achieving the visual result that meets a more demanding cataract patient’s needs remains challenging because of imprecision in IOL power calculations, unpredictable effects of wound healing, and IOL rotation in the case of toric IOLs. According to a 2013 Market Scope report, between 5% and 30% of patients require a secondary enhancement procedure to improve visual outcomes after conventional IOL implantation.
Figure 1. The Light Adjustable Lens.
LIGHT ADJUSTABLE LENS
With the development of the Light Adjustable Lens (LAL [Calhoun Vision];Figure 1), surgeons have the option to offer their patients the only postoperatively adjustable IOL designed to provide predictable results and customized vision after implantation. This standard three-piece foldable silicone IOL was designed and developed by Daniel Schwartz, MD, an ophthalmologist at the University of California, San Francisco, and Robert Grubbs, PhD, a professor at the California Institute of Technology (who won the Nobel Prize for Chemistry in 2005).

Figure 2. The Light Delivery Device.
The LAL technology allows the power of the IOL to be adjusted postoperatively in a noninvasive manner to reduce and eliminate residual hyperopic, myopic, and astigmatic corrections of at least 2.00 D and to change the total amount of asphericity in the eye to provide an increased depth of focus. A specially designed ultraviolet (UV) Light Delivery Device (LDD; Figure 2) was developed to deliver the desired spatial irradiance profile (Figures 3 and 4) and the exact amount of light exposure onto the LAL.
A video animation of the LAL.
The LAL is composed of UV-photosensitive materials called macromers that respond to UV light of a certain wavelength. For example, as illustrated in Figure 5, to correct residual hyperopic error, power can be added by irradiating the central portion of the lens with UV light, which causes polymerization of the macromers in the central region. Macromers in the nonirradiated outer portion of the lens diffuse into the centrally irradiated area to maintain equilibrium throughout the lens, causing a swelling and power increase in the irradiated portion of the lens. Conversely, a myopic correction can be accomplished by subtracting power from the LAL by directing the UV light to the outer periphery of the LAL.
The LAL is implanted using standard cataract surgery techniques. After implantation, the eye is allowed to heal and achieve refractive stability over a period of approximately 3 weeks. The patient then returns for up to two power adjustments of the LAL. When patient and surgeon are pleased with the visual outcome, the surgeon will irradiate the entire lens to remove all macromers and permanently lock in the lens power.
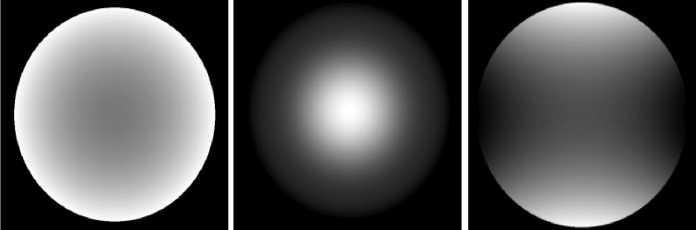
Figure 3.Spatial irradiance profiles.
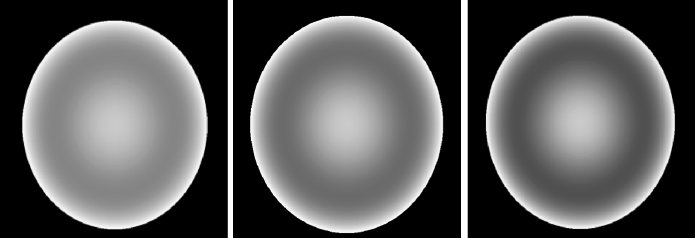
Figure 4.Spatial irradiance profiles for aspheric adjustments.
The LAL has been commercially available in Europe since 2008 and in Mexico since 2012. Calhoun Vision is currently conducting a phase 3 FDA clinical trial, which involves the treatment of 400 eyes implanted with the LAL and 200 receiving a control (previously approved monofocal IOL) at 18 sites across the United States. Participating investigators, including myself, have seen excellent outcomes thus far for phase 3 subjects implanted with the LAL.
ADJUSTABLE BLENDED VISION
While Calhoun Vision works toward completing the phase 3 study in the United States, the company continues to bring LAL enhancements to the international marketplace. Currently, Calhoun Vision is finalizing its new presbyopia-correcting solution called adjustable blended vision (ABV). ABV is an innovative LAL treatment designed to provide patients with excellent binocular distance, intermediate, and near vision without the need for glasses. The approach involves precise, controlled changes of the spherical aberration in the eye to increase the depth of focus.
Clinical data from trials run in Murcia, Spain (Pablo Artal, PhD), and Tijuana, Mexico (Arturo Chayet, MD), have resulted in excellent spectacle-free vision of high quality at all distances. Clinical results from Mexico showed that at 1 week after final lock-in for 40 eyes (20 patients), 90% of patients achieved a binocular uncorrected near visual acuity of 20/32 (J2) or better, while 95% achieved 20/25 or better uncorrected distance visual acuity. Ten percent of patients were reported to have achieved 20/32 or better uncorrected intermediate visual acuity. The company is working to bring this exciting near vision solution to the international marketplace later this year.
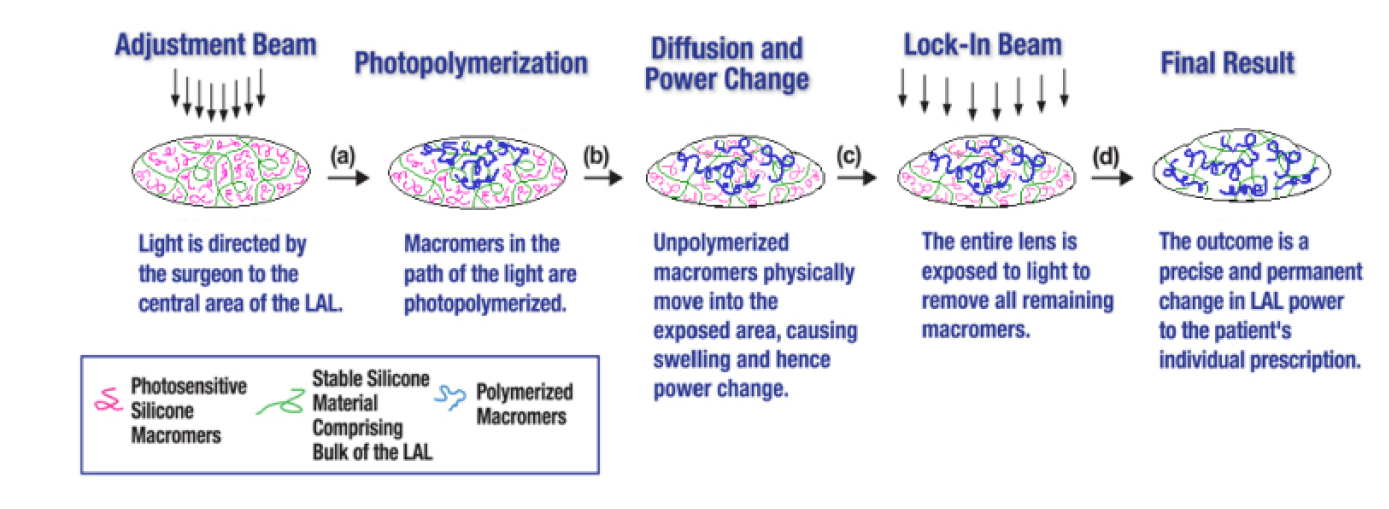
Figure 5.Mechanism of action: adding power to the LAL.
CONCLUSION
By providing customization and predictability at the fingertips of ophthalmic surgeons, as demonstrated in the new developments to be released outside the United States, the LAL will certainly represent a major step forward in cataract surgery.



