If you’ve made the choice to be in ophthalmology, chances are you enjoy using a deft skillset to perform in the operating room (OR). While we’re good at delivering an outpatient procedure that has immense outcomes for our patients’ vision and livelihood, how efficient are we when executing these procedures? To keep your surgical center or hospital productive, efficiency is critical. Our surgical and staffing needs are a bit different than other surgical services. Here are 10 tips to consider to boost your OR efficiency.
1. Speak the same language.
Don’t assume that the circulator understands things the same way you do. Ask the circulator you work with the following questions: “What is your definition of ‘turnover time’?” and “What does ‘start time’ mean to you?” The answers to these questions are likely to differ! There should be a clear understanding that “start time” is “incision time” and does not refer to when the patient enters the room. Everyone should be aware that the scheduled “procedure time” is the “incision time” and work around that—ie, with a 7:30 AM start time, the patient should be prepped and draped and the surgeon ready to make an incision on or before 7:30 AM.
When asking different staff members about their definition of “turnover,” most nursing staff consider this to be the period from when one patient is out of room until the next patient is brought into the room. To optimize efficiency, however, it’s important to recognize that “turnover” really means the period from when the surgeon ends one case until an incision is made in the next case. This allows for accurate assessment of each step of the process. You can’t improve a process until you identify it.
2. Surgical eye beds are crucial preoperatively.
It’s most efficient to have the patient get on the surgical bed in the preoperative area and then move to the OR and subsequently to the post-anesthesia care unit (PACU) on that same bed. Have the patient move to a chair for postop instructions so that you can optimize the use of your surgical beds.3. Incorporate combined dilating drops.
These drops, which are being offered more frequently these days, cut costs and make it easier for your nurses to dilate pupils. There are now even some combination drops that include NSAIDs and tetracaine or lidocaine jelly.4. Universal leads help at all stages of the procedure.
The monitoring machines should use compatible leads in the preop/operating room and PACU. This will save time when moving the patient. Also, most patients only need a saline lock, rather than an IV, unless they are fluid deficient. Teach the preop nurse how to position the patient so that when you get to the OR, the patient is in the right position.
5. Teach your staff to prep and drape.
It’s important to teach your scrub tech to have the patient prepped and draped when you walk into the room. Educate the staff on the way you want this done, and then trust them to do it. At the end of the case, let the team remove the drapes. You should go to the next room or to preop to mark the next patient.
6. Start postop education early.
In the PACU, ophthalmic patients are usually discharged within 15 minutes if they haven’t had heavy sedation. Thus, you should start patients’ postop education in the clinic, prior to the procedure. The nurse in preop should just be reminding patients of their postop instructions, not educating them for the first time. Also, be sure your responsible driver doesn’t leave the building.
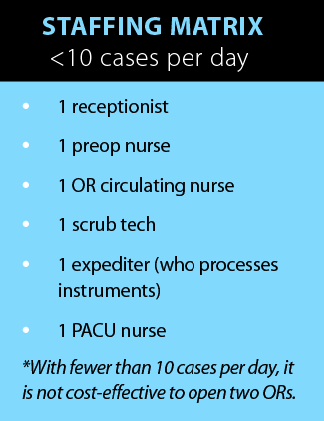
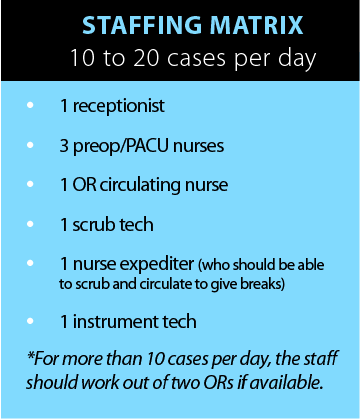
7. Follow the appropriate staffing matrix.
Below are two staffing matrices to consider when deciding whether you should use one or two rooms while operating. Fewer than 10 cases per day can effectively be performed in one OR. If you are doing 10 to 20 cases per day, however, you should consider having two ORs.
8. Evaluate your anesthesia setup.
As far as anesthesia goes, both the CRNA (nurse) anesthesiologist and MD anesthesiologist are quite competent and effective in the outpatient setting. Historically, the CRNA has been the most effective anesthesia provider for high-volume ophthalmology. However, since CMS started requiring an MD assessment immediately prior to the procedure and again prior to discharge, incorporating time or another MD into the mix needs to be considered. If you are using a CRNA, you, the MD, must do these assessments yourself. If you have an MD anesthesiologist, he or she can assume the responsibility and you can focus on the next surgical procedure.
9. Analyze your instrument needs.
The number of instrument sets needed will depend on your surgical time (an 8-minute cataract procedure requires more sets than a 12-minute surgery) and on the number of ORs you have. For example, if you work out of two ORs and do an 8- to 10-minute procedure, you would want to increase the number of instrument sets.
All sets should be complete (phaco handpieces, diamond blades, etc.). Flashing or immediate-use sterilization can be used only if you drop an instrument, but all instruments must go through a dry cycle. You must wrap your instruments for sterilization, but the procedure should never be delayed because you’re waiting on instruments. It’s worth purchasing another set.
10. Assess bottleneck.
Everything should be working around the surgeon’s actual surgical procedure. If he or she is delayed for any reason, you will need to evaluate the cause. Experience says it’s one of the following reasons: (1) the patient did not arrive on time, (2) preop doesn’t have enough time to admit, (3) you are waiting on instruments, or (4) the PACU is full.
If delays are occurring, it’s also important to look for potential issues with patient scheduling. Be sure to assess how long it takes the preop staff to admit and prepare the patient for surgery. If it’s taking 30 minutes, then the patient should be admitted earlier to accommodate. If you have a procedure time of 10 minutes or less, you should have three to four patients arrive before you start your first case. (You would assess/mark these patients prior to doing your first case.) There would always be one patient in the OR and one ready to assess/mark.
If that’s not the problem, then assess your admitting times. Do you have an 8-minute procedure and admit one patient every 30 minutes? Do you have too many patients in the PACU, delaying your procedure until some are discharged?
What is the process in the PACU? Are you giving them hot coffee and a snack? Your objective should be to discharge patients within 15 minutes of being admitted to the PACU. Remember, these are patients that have had local/topical anesthesia with minimum sedation! If you find a routine delay in the start of your next procedure, you will need to assess all the above.
Everything related to surgical efficiency always comes back to evaluating what is happening from the time the surgeon puts the last “stitch” in until the incision is made in the next case. When you identify that time, it will lead you to identify what’s going on in each step of the process in between.
If you want to be efficient, you have to be involved. You can’t be making calls between cases or waiting for the team to call you back to the OR.
SUMMARY
Overall, you should always get back to the OR as quickly as possible. Gown and glove. The scrub tech may not be ready initially, but he or she wants to please you and will eventually get ahead of you. Do all of your cataract cases FIRST. Don’t do YAGs/blephs between cataract procedures; it slows the momentum, and you will lose the team if they have to wait for you.
These are just a few tips to consider for maximizing your efficiency in the OR. I hope you find the right balance to remain productive.




