The subspecialty of vitreoretinal surgery has undergone a revolution in the past decade. The opening shot in the retinal revolution can be traced to the 2005 American Society of Retina Specialists meeting in Montreal, when Phil Rosenfeld, MD, presented the first intravitreal bevacizumab (Avastin; Genentech) data in neovascular age-related macular degeneration (AMD).1 Although the amount of research that was invested prior to human bevacizumab injections was substantial,2 translational science in retina accelerated at an exponential rate after molecular medicine moved into routine retina clinics following that seminal presentation. In 2016, retinal medicine and surgery can be described as lightning in a bottle.
INTRAVITREAL THERAPY
The pace of research and discovery in retina gained momentum in subsequent years. Currently, bevacizumab, ranibizumab (Lucentis; Genentech), and aflibercept (Eylea; Regeneron) offer effective, commercially available treatments for a variety of disease states.3-7 These injections have broad applicability to divergent pathology and have revolutionized the treatment of subretinal choroidal neovascular disease and intraretinal vascular disease.
However, we already recognize limitations to these remarkable treatments. In wet AMD, 5-year results of the Comparison of Age-Related Macular Degeneration Treatments Trials (CATT) showed that gains in the first 2 years of anti-VEGF therapy were not maintained at 5 years8 in the study population. In diabetic macular edema (DME), 2-year results of the Diabetic Retinopathy Clinical Research Network (DRCR.net) Protocol T showed that between 41% and 64% of patients required laser despite regular monitoring and treatment with commercially available anti-VEGF medications.9 These results may be due to a variety of factors, including potential under-treatment in these trials. One of the challenges with current intravitreal medications is the burden of care—or number of repeated injections required—to obtain the best possible clinical results.
Fortunately, there are a number of potentially longer-lasting and more efficacious medications advancing through clinical trials. Brolucizumab (RTH-258, Alcon) is a novel anti-VEGF agent currently in phase 3 clinical trials. It is very small, at 26 kDa compared with 50 kDa for ranibizumab and 149 kDa for bevacizumab. The small size allows a molar concentration more than 20 times greater than ranibizumab in the same injection volume, and brolucizumab was shown to be noninferior to aflibercept for wet AMD in a phase 2 study. Extension dosing also maintained efficacy with injections as infrequently as every 12 weeks.10
Another novel molecule being explored are anti-VEGF DARPins, or designed ankyrin repeat proteins, which are an alternative to antibodies for therapeutic delivery. DARPins are novel for their small size, high stability, low-cost production in bacteria, and rapid generation of target-specific DARPins. They can also be “tied” together in multispecific formats that target several receptors with one molecule.11 Abicipar pegol (Allergan) is a 34-kDa anti-VEGF DARPin currently under phase 3 study, with a protocol studying extension between injections out to 12 weeks. The phase 2 REACH study presented in 2014 showed abicipar pegol compared favorably to ranibizumab with less frequent injections.12
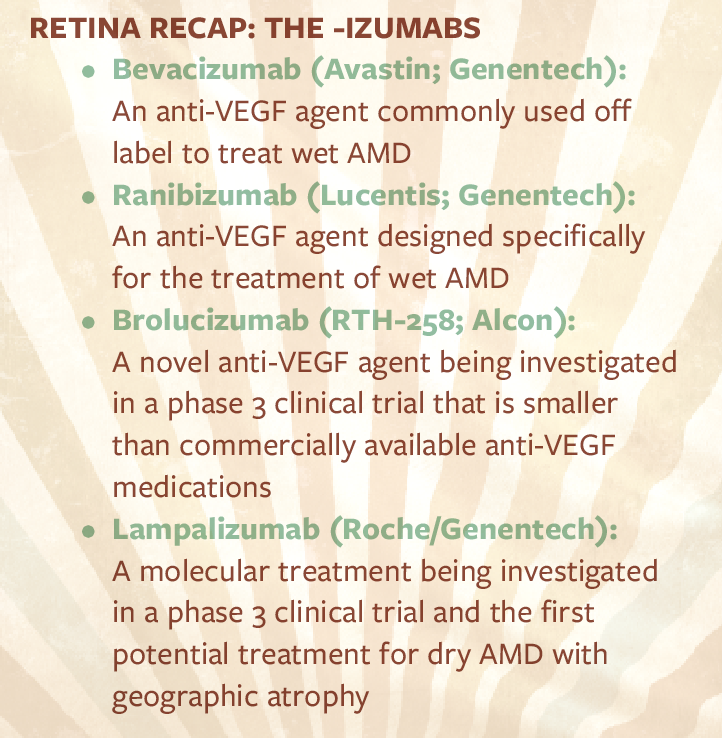
Dry AMD has been vexing to retina specialists. Despite the remarkable advances in treating wet AMD and retinal vascular disease in the past decade, there is still no commercially available treatment for atrophic AMD. However, there has been progress in the understanding of the pathophysiology of dry AMD, and there is one molecular treatment being investigated in a phase 3 study. Lampalizumab (Roche/Genentech) demonstrated favorable phase 2 results in the MAHALO trial, with a reduction in the advancement of geographic atrophy in one group of patients with a specific biomarker.13 The results of the study were unique in that treating to a specific biomarker would enable true individualization of therapy to patients most likely to benefit. If the results are supported in the ongoing pivotal phase 3 trials, lampalizumab will be the first medication with proven safety and efficacy for dry AMD with geographic atrophy.
VITREORETINAL SURGERY
Even with all of the excitement in intravitreal therapy, surgical retina has continued to advance. Smaller-gauge surgery has enabled procedures to be performed with shorter surgical times, less ocular surface trauma, and more rapid recovery.14 These benefits have come with the requirement for surgeons to alter their techniques to limit some of the risks of sutureless surgery, such as postoperative hypotony; however, the widespread adoption of small-gauge vitrectomy seems to reflect the benefits outweighing the risks.
Recently, 27-gauge instrumentation has become available, and some surgeons are advocating this smallest-gauge platform for complex cases.15 Vitrectomy probes now cut at speeds that allow greater surgeon control and minimize peripheral retinal traction.16 The future is likely even faster: Ultrasonic probes, first explored in the 1970s but now under renewed development, may enable cut rates of up to 1,000,000 cuts per minute, essentially eliminating vitreous traction and further improving control.17
SUMMARY
It is easy to be excited about the future of the vitreoretinal subspecialty in 2016. With the onslaught of improvements in medical and surgical retina, our next decade promises to be logarithmically more exciting than the last.
1. Rosenfeld PJ. Systemic bevacizumab (Avastin) therapy for neovascular age-related macular degeneration (SANA) study: 12 week outcomes. Paper presented at: American Society of Retina Specialists annual meeting; July 16-20, 2005; Montreal, Canada.
2. Rosenfeld PJ. The path to intravitreal bevacizumab. Retina Today. May/June 2009.
3. Rosenfeld PJ, Brown DM, Heier JS, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355(14):1419-1431.
4. Brown DM, Michels M, Kaiser PK, Heier JS, Sy JP, Ianchulev T. Ranibizumab versus verteporfin photodynamic therapy for neovascular age-related macular degeneration: two-year results of the ANCHOR study. Ophthalmology. 2009;116(1):57-65.
5. Heier JS, Brown DM, Chong V, et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology. 2012;119(12).
6. Nguyen QD, Brown DM, Marcus DM, et al. Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology. 2012;119(4):789-801.
7. Korobelnik JF, Do DV, Schmidt-Erfurth U, et al. Intravitreal aflibercept for diabetic macular edema. Ophthalmology. 2014;121(11):2247-2254.
8. Maguire MG, Martin DF, Ying G, et al. Five-year outcomes with anti-vascular endothelial growth factor treatment of neovascular age-related macular degeneration. Paper presented at: Association for Research in Vision and Ophthalmology annual meeting; May 2016; Seattle, Washington.
9. Wells JA, Glassman AR, Ayala AR, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema: two-year results from a comparative effectiveness randomized clinical trial. Ophthalmology. 2016;123(6):1351-1359.
10. Jaffe G. OSPREY: a multidose randomized study of brolucizumab compared to aflibercept for the treatment of neovascular age-related macular degeneration. Paper presented at: Macula Society annual meeting; February 25, 2016; Miami, Florida.
11. Stumpp MT, Amstutz P. DARPins: a true alternative to antibodies. Curr Opin Drug Discov Devel. 2007;10(2):153-159.
12. Raj M. Abicipar pegol (anti-VEGF DARPin) phase 2 study in patients with neovascular age-related macular degeneration. Paper presented at: American Society of Retina Specialists annual meeting; August 12, 2014; San Diego, California.
13. Williams DF, Li Z, Beres T, Le K, Strauss EC. MAHALO phase II study: safety, tolerability and activity of lampalizumab (anti-factor D) in patients with geographic atrophy. Paper presented at: American Society of Retina Specialists; August 27, 2013; Toronto, Canada.
14. Thompson JT. Advantages and limitations of small gauge vitrectomy. Surv Ophthalmol. 2011;56(2):162-172.
15. Berrocal MH, Williams DF. Smaller gauge instruments are better and safer. Retina Today. January/February 2015.
16. Abulon DJ, Buboltz DC. Performance comparison of high-speed dual-pneumatic vitrectomy cutters during simulated vitrectomy with balanced salt solution. Transl Vis Sci Technol. 2015;4(1):6.
17. Rizzo S, Faraldi F. The future of small-gauge vitectomy. Retina Today. March 2014.