At the time of cataract surgery, patients have the opportunity to reduce their need for glasses with presbyopia-correcting (extended depth of focus [EDOF] and multifocal) IOLs. Unfortunately, surgeons may not even offer this option to many patients because of concern for side effects. Despite many advances, most surgeons probably still consider multifocal (bifocals, trifocals, or progressive bifocals) glasses to be the standard of care and presbyopia-correcting IOLs to be premium offerings. Although some patients use bifocal or multifocal glasses as a spectacle treatment of presbyopia, they have likely had to overcome the side effects of image jumping, visual distortions, peripheral vision limitations, and contact irritation—as well as the need for regular cleaning, maintenance, and replacement.
PHYSICAL AND FISCAL RISKS
Despite their wide availability and status as an acceptable (perhaps default) alternative to the surgical treatment of presbyopia, do bifocal and multifocal glasses pose a greater health risk than the inconveniences listed above? Could there be morbidity—and even mortality—risks associated with their use? We have known for many years that bifocal and multifocal glasses reduce edge-contrast sensitivity and depth perception in the lower visual field.1 Because of these distortions, patients can miss curbs and steps in the course of their daily lives, leading to trips and falls.
In our elderly cataract-age patients, falls can be devastating.2 Every second of every day, an elderly American falls.3 Around half of these falls result in injury, 10% or 15% of which can be severe. Each year, falls result in 2.8 million ER visits; 800,000 hospital admissions; and more than 27,000 deaths.4 Regardless of physical injury, one in three people develop post-fall anxiety syndrome, leading to functional decline, depression, social isolation, and lower quality of life.5 The economic impact of falls was over $31,000,000,000 (that’s billions with a “b”) in 2014.
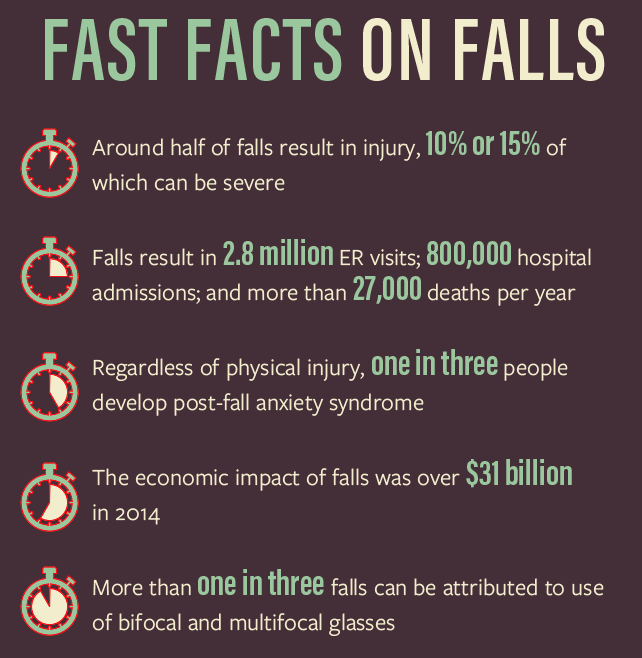
It is well known that first-eye cataract surgery can reduce falls by one-third.6,7 However, not many know that changing from bifocal or multifocal glasses to single-vision glasses can reduce falls by up to 40% in targeted populations.8 This is because bifocal and multifocal glasses increase the risk of falls in the elderly by 2.3-fold. More than one in three falls can be attributed to use of bifocal and multifocal glasses. If we extrapolate the data, nearly 1 million ER visits; 0.25 million hospital admissions; 10,000 deaths; and more than $10 billion of economic impact can be attributed to bifocal and multifocal glasses.9
If the Hippocratic oath calls on us, above all, to do no harm, should we be wary when prescribing bifocal or multifocal glasses to the elderly? What about our next cataract patient? Should we make him or her aware of the potential dangers of bifocal and multifocal glasses and encourage surgical options for presbyopia correction instead? Multifocal and EDOF IOLs may just be the safer option for our patients.
If a patient has problems with a presbyopic IOL, we have to deal with his or her complaints (and sometimes dissatisfaction). However, if a patient trips and falls because of the bifocal or multifocal glasses needed after our surgery, does he or she come to us? No—the patient goes the ER, the hospital, or the morgue. That may be the easier option for my practice and clinic flow, but is that the best thing for our patients?
CONCLUSION
Let’s remember to offer surgical presbyopia-correcting solutions to our patients. If we don’t because we fear the possible side effects of EDOF and multifocal IOL technology, we might just be kicking the can (or the patient might just be kicking the bucket) down the road.
1. Lord SR, Dayhew J, Howland A. Multifocal glasses impair edge-contrast sensitivity and depth perception and increase the risk of falls in older people. J Am Geriatr Soc. 2002;50:1760-1766.
2. Peel NM. Epidemiology of falls in older age. Can J Aging. 2011;30(1):7-19.
3. Falls are leading cause of injury and death in older Americans [news release]. CDC. www.cdc.gov/media/releases/2016/p0922-older-adult-falls.html. Accessed November 10, 2017.
4. Fall prevention facts. National Council on Aging. www.ncoa.org/news/resources-for-reporters/get-the-facts/falls-prevention-facts. Accessed November 10, 2017.
5. Masud T. Epidemiology of falls. Age Ageing. 2001;30:3-7.
6. Harwood RH, Foss AJE, Osborn F, Gregson RM, Zaman A, Masud T. Falls and health status in elderly women following first eye cataract surgery: a randomised controlled trial. Br J Ophthalmol. 2005;89:53-59.
7. Palagyi A, Morlet N, McCluskey P, et al. Visual and refractive associations with falls after first-eye cataract surgery. J Cataract Refract Surg. 2017;43(10):1313-1321.
8. Haran MJ, Ivers RQ, Simpson JM, et al. Effects on falls of providing single lens distance vision glasses to multifocal glasses wearers: VISIBLE randomised controlled trial. Br J Ophthalmol. 2010;340.
9. Value of US ophthalmology market from 2009 to 2014 (in billion US dollars). Statista. www.statista.com/statistics/445654/us-ophthalmology-market-size. Accessed November 10, 2017.



