Editorially independent content supported with advertising from

If you use a 1.00 D cutoff to decide between a toric IOL and limbal relaxing incision (LRI), like I did for many years, then good news—you can significantly improve your outcomes with four new rules of astigmatism management.
In the past few years, much has changed in our understanding of astigmatism planning during cataract surgery. I call it the Age of Astigmatism Enlightenment (Figure 1). Thanks to Drs. Doug Koch, Graham Barrett, Warren Hill, and others, many longheld practices and beliefs have been debunked or updated. Using these updated guidelines can significantly increase toric IOL accuracy and result in 80% to 90% of patients ending up with less than 0.50 D of residual cylinder.

Figure 1. The Age of Astigmatism Enlightenment.
Let’s take an example case. A 68-year-old woman desires clear uncorrected distance vision after cataract surgery. Her topography (Figure 2) reveals 0.78 D of with-the-rule (WTR) astigmatism at 92°. Automated keratometry reveals 1.00 D at 94°, and the Lenstar (Haag-Streit) keratometry reading is 0.85 D at 97°.
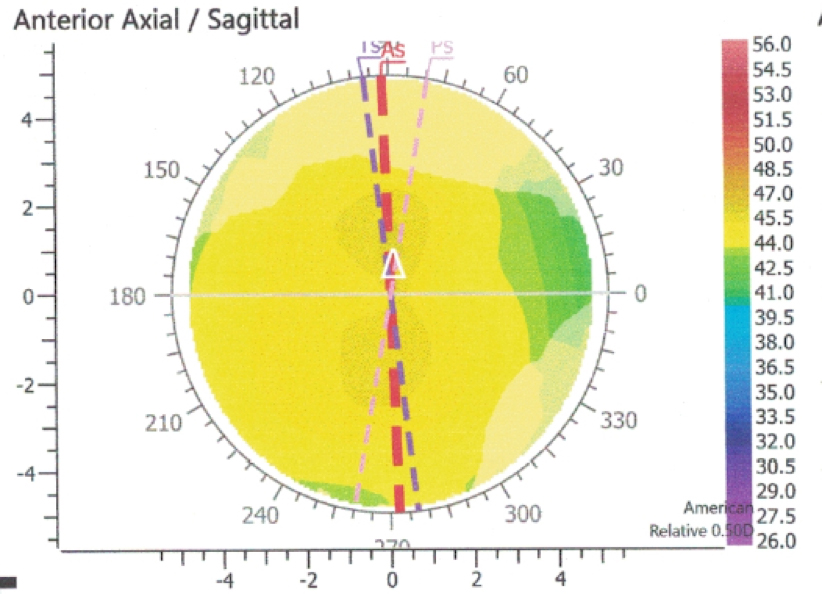
Figure 2. The patient’s topography revealed 0.78 D WTR astigmatism at 92°.
Just a few years ago, I would have entered these figures into either the Alcon or Abbott Medical Optics toric calculator, plugged in 0.40 D for surgically induced astigmatism (SIA) at 180°, and then been recommended a ZCT150 (Figure 3A) or SN6AT3 (Figure 3B) to be placed WTR. And I would have likely been really off. But we’re smarter now.
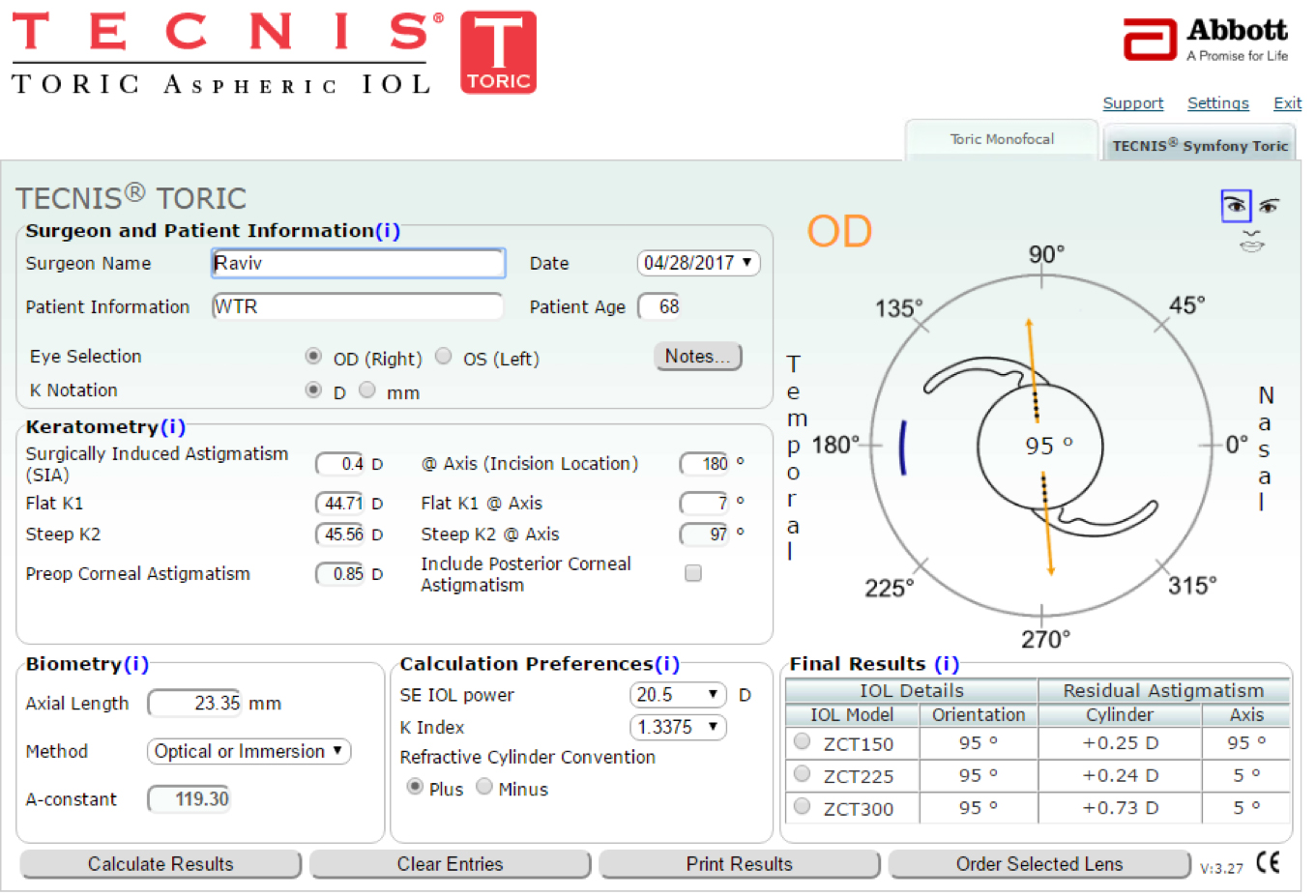
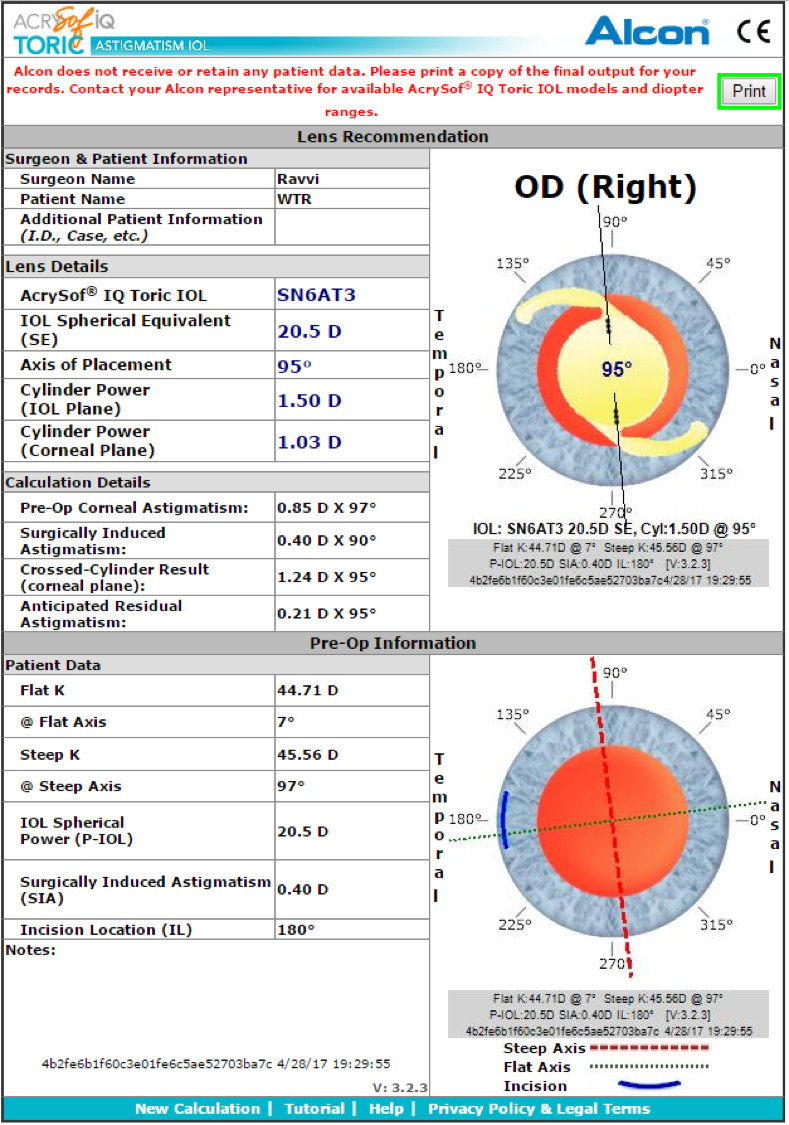
Figure 3. Toric calculators recommending a ZCT150 (top) or SN6AT3 (bottom) to be placed WTR would have been incorrect. For better results, check off the “Include Posterior Corneal Astigmatism” box on the Tecnis IOL calculator, and use the newer Alcon Toric Calculator incorporating Barrett, instead of the older calculator shown here.

FOUR NEW RULES OF ASTIGMATISM MANAGEMENT
Account for Posterior Corneal Astigmatism
We now know that our keratometry measurements only measure the anterior corneal curvature and that we need to account for hidden posterior corneal astigmatism. To be accurate with toric IOLs, we need to under-treat anterior WTR and overtreat ATR astigmatism.
Posterior corneal astigmatism can either be measured directly or estimated by theoretical formulas. Preoperatively, we can attempt to measure the posterior cornea (and hence total corneal astigmatism) by some Scheimpflug topographers such as the Pentacam (Oculus) and Galilei (Ziemer), LED topography such as the Cassini (i-Optics), and soon swept-source OCT.
Posterior corneal astigmatism can also be theoretically accounted for with the Baylor nomogram or the Barrett Toric Calculator. Finally, intraoperative aberrometry can also measure the eye’s total astigmatism when done in the aphakic state, helping with toric IOL magnitude selection. To date, the most accurate methods appear to be the theoretical models such as the Barrett Toric Calculator.
Until recently, we had always been advised to ignore the refractive cylinder and only use keratometry to calculate for torics. However, it turns out that if a patient has significant refractive against-the-rule (ATR) cylinder and only, say, 0.40 D of keratometric ATR cylinder, then we should expect extra posterior corneal cylinder and chose a higher toric IOL power to treat it.

Use a Centroid Value of 0.10 D for SIA
In the past, when entering SIA into our toric calculators, we usually estimated 0.30 D to 0.50 D based on calculations assessing the mean change in absolute keratometry. Some of us dutifully calculated our own mean SIA. And for years, many of us operated on the steep axis.
It turns out that our most consistent results are with a temporal clear corneal incision. We have learned that entering a centroid value of 0.10 D, which takes into account the vector of astigmatism, gives the best results to all surgeons operating temporally—surprisingly with little significant variance for incisions between 2.20 D and 2.75 D.


Consider Long-Term Astigmatic Drift
Hayashi1 has studied and reported on the long-term drift of astigmatism. In most people, WTR will drift to ATR at an average rate of 0.34 D per decade. So, if one targets 0.35 D of WTR residual astigmatism, the patient should be in great shape for at least 20 years or more.

Axis Flipping Is Perfectly OK
When prescribing glasses, the common wisdom is to proceed with extreme caution if flipping an axis. This led earlier calculators to recommend IOLs that left more residual cylinder, to avoid axis flipping. We now know, however, that flipping a small amount of cylinder is tolerable and actually preferable when treating ATR astigmatism. On the other hand, we shouldn’t have to flip for WTR cylinder, as we want to leave some residual WTR.
LRI VS TORIC IOL
Existing studies2,3 show that toric IOLs are more accurate and stable than LRIs, so we should use torics whenever we can. In the United States, we have access to the T3 (Alcon) and ZCT150 (Johnson & Johnson Vision) and their presbyopia-correcting cousins; both the T3 and ZCT150 treat approximately 1.00 D of corneal cylinder, depending on IOL power.
Applying the rules above, I generally place a toric IOL for WTR astigmatism greater than 1.50 D and ATR greater than 0.40 D. I use femtosecond laser LRIs for the rest. Today, I personally calculate and refine my toric selection using the Barrett toric calculator and LED topography measurements, peeking at the refraction, and I utilize ORA (Alcon).
CONCLUSION
In the case described above, the new Barrett Toric Calculator with an SIA of 0.10 D recommends against a toric IOL. My Cassini total corneal astigmatism measurements also revealed only 0.61 D of WTR cylinder. I therefore applied paired penetrating femtosecond LRIs at 90°. ORA guidance was then used to refine by opening up the LRIs (with a Sinskey hook) to further reduce the cylinder to about 0.40 D. The patient ended up with 20/20 uncorrected vision and a plano -0.50 X 180 refraction.
With good use of our astigmatism enlightenment tools, best practices have reported more than 90% of eyes within ±0.50 D of residual cylinder. Also, I’ve noticed that since the cataract patient demographic is older, I tend to have much more ATR cylinder to treat; most of those patients get a toric IOL, so the toric eligible rate can approach 50% in many cataract practices.
1. Hayashi K, Hirata A, Manabe S, Hayashi H. Long-term change in corneal astigmatism after sutureless cataract surgery. Am J Ophthalmol. 2011;151(5):858-865.
2. Leon P, Pastore MR, Zanei A, et al. Correction of low corneal astigmatism in cataract surgery. Int J Ophthalmol. 2015;8(4):719-724.
3. Lee J, Lee H, Kang DSY, Choi JY, Kim EK, Kim T. Comparison of toric foldable iris-fixated phakic intraocular lens implantation and limbal relaxing incisions for moderate-to-high myopic astigmatism. Yonsei Med J. 2016;57(6):1475-1481.



