William B. Trattler, MD: Genetics and environmental factors have been shown to play a role in the development of keratoconus (KC).1 KC is a polygenic disease, which means that multiple genes may affect its development and progression.2 Genetic data used to be out of reach for clinicians who identify and treat KC. Now, with AvaGen™, The Genetic Eye Test (Avellino), we can include genetic data in our assessment of a patient’s risk for developing KC, which can in turn drive our treatment decisions.
Here, Elizabeth Yeu, MD, and Mile Brujic, OD, FAAO, each share a case of a patient with possible KC whose genetic data proved useful for patient management.
CASE NO. 1: A REFRACTIVE EVALUATION
Elizabeth Yeu, MD: A 29-year-old Asian-American man presented to my office for a refractive surgery consultation. His glasses prescription had been stable for several years, and he was unable to wear soft contact lenses due to discomfort. His medical history was unremarkable. Central corneal thickness was 535 µm OD and 551 µm OS on ultrasound pachymetry. His manifest refraction, which reflected slight against-the-rule astigmatism, was:
- OD: -3.00 + 0.50 x 164
- OS: 3.00 +0.25 x 178
Dr. Trattler: I find that tests such as corneal topography can provide further details in patients such as this one. What did you find?
Dr. Yeu: It was determined that the patient had an average corneal power of 43.5 D in his right eye. Pachymetry on the Orbscan 3 (Bausch + Lomb) detected 496 µm central corneal thickness, thinner than what was seen on ultrasound (Figure 1). The thinnest part of the cornea was displaced approximately 0.7 mm from the center. Placido disc topography showed a bowtie pattern that was against the rule, but did not show anything suggestive of a crab claw pattern.
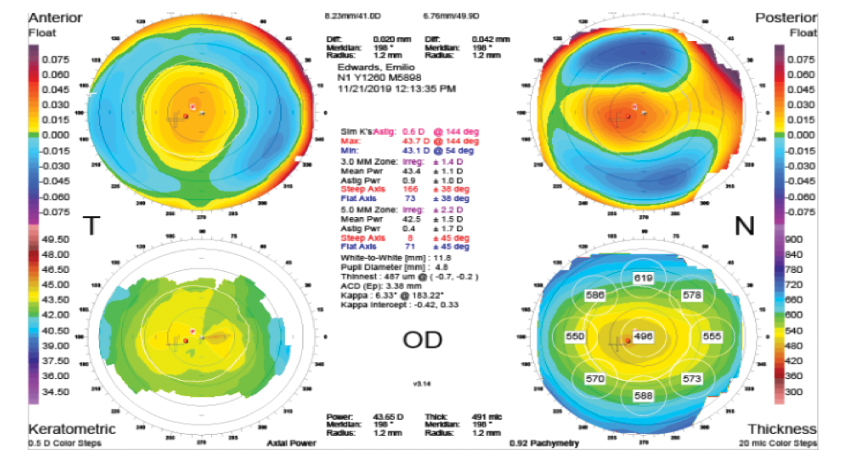
Figure 1. Orbscan 3 (Bausch + Lomb) imaging found slight displacement of the thinnest part of the cornea in the right eye, which had a central corneal thickness of 496 μm.
The left eye showed similar findings to the right eye, with a reduced central corneal thickness of 500 µm on Orbscan pachymetry (compared with 551 µm on ultrasound). In the left eye, the thinnest point was 1.3 mm from the center.
Mile Brujic, OD, FAAO: The detail that sticks out to me in this case is that the thinnest corneal region is so far displaced from the center axis in the left eye. Still, the anterior topography doesn’t suggest any abnormality. The fact that these details don’t all add up makes me suspicious of KC.
Dr. Yeu: Without genetic information, I would likely only recommend PRK surgery for this patient. However, now that we have the AveGen™ test, I elected to gather genetic data to determine this patient’s risk for KC.
This patient’s risk score came back as 99 out of 100, which is the highest risk score I’ve seen in a patient who has undergone a genetic risk assessment. It was determined that he had multiple risk variants in keratoconus-related genes.
Dr. Brujic: If a patient comes back with a moderate or high risk for KC and no aggravating environmental factors such as allergies, I re-educate about the importance of keeping their hands away from their eyes. If they are looking for vision correction options other than glasses or surgery, I might be inclined to fit them with a scleral contact because it actually blocks access to the cornea, preventing the potential risk that eye rubbing can cause. In this case, the patient had no allergies and a relatively normal cornea. However, it should be noted that his genetic risk is very high.
Dr. Trattler: This patient is likely to progress. I think a 6-month follow-up is warranted, at which point I would repeat all measurements. With this high risk score, I would advise against LASIK and have a long discussion as to whether or not we should consider PRK, as this patient is at increased risk for developing progressive corneal steepening with or without PRK.
Dr. Yeu: I agree with that assessment. I told the patient that we would have to defer LASIK or PRK surgery, but that an implantable collamer lens was an option to correct his refractive error.
CASE NO. 2: A CASE OF EXTREME ASTIGMATISM
Dr. Brujic: A 35-year-old man was referred to my practice for a scleral lens consultation. He had no significant medical history, no history of allergies, and was not taking any medications. The referring clinician could provide no history of anatomic change, as this clinician had only examined the patient once before referral. Central corneal thickness measurements were 520 µm OD and 511 µm OS. He wore glasses to correct for refractive error. His manifest refraction was:
- OD: -0.75 -6.75 x 010
- OS: +0.25 -7.25 x 165
Dr. Trattler: This is excessively high astigmatism, which is likely why you’re seeing this patient in the first place.
Dr. Yeu: My instinct is to say that this patient very likely has KC, and I would expect to detect suspicious findings on topographic assessment.
Dr. Brujic: My assumptions were the same as Dr. Yeu’s. The fact that this patient had with-the-rule astigmatism was encouraging, but the other initial data pointed toward possible KC. Topography was unremarkable in both eyes, and corneal thickness mapping and epithelial thickness mapping showed that his minimum corneal thickness deviated slightly from center in his left eye (Figure 2).
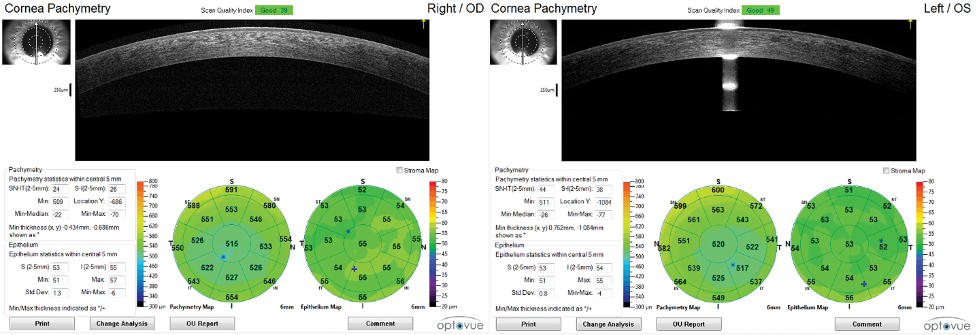
Figure 2. Corneal thickness mapping and epithelial thickness mapping of the right eye (A) was unremarkable. In the left eye, minimum corneal thickness deviated from the center axis (B).
My office calculated his risk of KC based on these clinical findings and determined that he had an above-average risk of KC in the left eye.
Dr. Trattler: The epithelial thickness map of the patient’s left eye does not show significant thinning over the apex—if there is indeed an apex. In a patient with KC, I usually need to see thinning before I diagnose KC.
Dr. Brujic: Given the conflicting nature of this patient’s clinical examination, we administered AvaGen™. The patient demonstrated a risk score of 3 out of 100, which indicates a low risk for KC. During test administration, an interview with the patient revealed no family history of KC and no known cases of extreme astigmatism. Given these new genetic and family history data, it was determined that this patient was at low risk for developing KC. We proceeded with a scleral lens fitting and advised the patient to avoid eye rubbing.
Dr. Yeu: This case demonstrates the value of genetic data in a clinical assessment. This patient’s extraordinarily high with-the-rule astigmatism would raise a red flag for me, but seeing the very low genetic risk score helps provide a more robust data set from which to work and increases the confidence in the patient management decision.
Dr. Trattler: Part of the beauty of the AvaGen™ Genetic Eye Test is that it tests for 75 known genes that are related to KC risk, as well as thousands of variants. Given how thorough the test is, we know that the risk score is a reliable metric to include in our assessments.
CONCLUSION
Dr. Trattler: The more robust the clinical data at our disposal, the more personalized our care can be. In an era when genetic information can be easily gathered and packaged in an easy-to-interpret report, practices that diagnose KC should consider including AvaGen™ in their armamentarium.






