CASE PRESENTATION
A 70-year-old woman underwent phaco cataract surgery on her right eye 3 years ago, and postoperative UCVA was 20/20. Although this visual acuity was satisfactory, the patient reported seeing rainbows around lights, around most objects, and when looking through glass. Upon examination, the refraction in the right eye was plano, and the Tecnis one-piece IOL (model ZCBOO, Johnson & Johnson Vision) was clear and centered in the bag. A wide-diameter Nd:YAG laser posterior capsulotomy failed to improve the rainbow glare, as did a trial of miotic drops.
The patient presents for a second opinion on a visually significant cataract in her left eye. She states that she noticed the rainbow glare immediately after cataract surgery on her right eye. She adds that the phenomenon was not present beforehand and is not present in her left eye.
On examination, subtle peripheral epithelial basement membrane dystrophy (EBMD) is evident in both eyes, but corneal astigmatism is mostly regular on topography (Figure). The irides are light blue. The pupils maximally dilate to 6.5 mm without evidence of pseudoexfoliation, and the patient does not administer systemic medications.
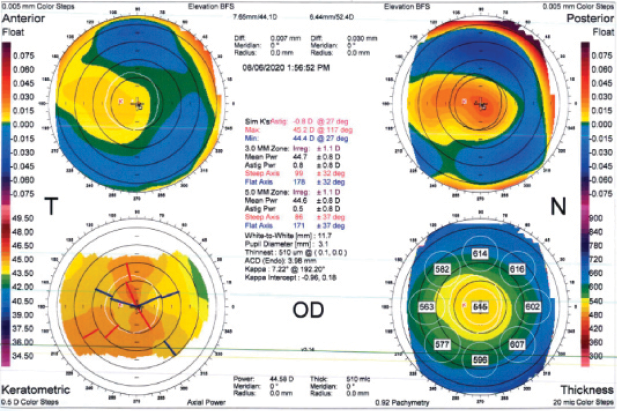
Figure | Topography of the right eye.
A 3+ nuclear sclerotic cataract is evident in the left eye. The patient is an artist. She states that “yellow vision” is interfering with her daily activities, including painting. She desires cataract surgery on the left eye but has delayed out of concern that she will experience the same highly disturbing postoperative dysphotopsia in this eye as well. She asks that all measures be taken to prevent this and inquires if anything can be done to fix the rainbows in her right eye. The patient has a history of success with monovision using soft contact lenses. She is willing to consider all strategies to improve her vision and minimize the chance of postoperative rainbow glare.
How would you proceed? Which IOL material and type would you use, and why? Would you change your standard technique in any way? Would laser cataract surgery be advantageous in this case? What size capsulotomy would you create? Would you treat the EBMD in either eye? Would you offer to treat the rainbow artifact in the right eye? If so, how, and would you address the right or left eye first?
—Case prepared by Christopher E. Starr, MD
Damien Gatinel, MD, PhD
The occurrence of rainbow-like visual phenomena after cataract surgery is rare in my experience. The undesirable phenomenon can almost certainly be attributed in this case to the IOL implant. This chromatic dispersion may be linked to defective material or to machining that caused, for example, microscratches on the surface that are diffracting light. It could be interesting to inspect the surface of the implant at very high magnification to look for marks or evenly spaced striations whose orientation correlates with the orientation of the chromatic dispersion observed by the patient. If this type of abnormality is noted and implicated in the occurrence of rainbow glare, an IOL exchange can be discussed, but surgery could be difficult 3 years after implantation.
If the aforementioned mechanism is present in the right eye, I would select a different type of IOL for the left eye. My preference would be an IOL without a blue-light filter (no yellow implant) so as not to cause a difference in color perception. I would not change my surgical technique, and I do not think that laser cataract surgery would be of particular benefit here. Specific treatment of EBMD is not warranted, in my opinion, if it has been clinically quiescent.
Samuel Masket, MD
This patient appears to have an uncommon form of dysphotopsia, chromatic positive dysphotopsia, likely due to the acrylic IOL and her particular central nervous system sensitivity. Because symptoms began immediately after cataract surgery, no benefit was to be expected from a laser capsulotomy. Surgeons should be mindful that an unnecessary posterior capsulotomy serves only to make an IOL exchange, perhaps needed here, more challenging. Based on my experience, exchanging the current IOL for one with optic material that has a lower index of refraction and lower surface reflectivity would have roughly an 85% likelihood of success.1,2 This patient should be approached with empathy, explanation, and assurance that her surgery was perfect, although she is experiencing an undesired optical phenomenon.
The best way to evaluate EBMD is with Placido disc imaging. Assuming normalcy, EBMD would be addressed with careful attention to the ocular surface during surgery, and a bandage contact lens would be placed at the end of the case. Otherwise, a superficial keratectomy is indicated before surgery. Given the right eye’s excellent visual acuity, I would prefer to begin with cataract surgery on the left eye, and I would avoid the use of a femtosecond laser interface in an effort to protect the cornea.
If it avoids problems similar to those encountered in the first eye, cataract surgery on the second eye often eliminates the need to perform an IOL exchange in the first eye. Based on this patient’s successful history with monovision, I would opt for a monovision approach and target a refractive outcome of -1.00 D. I would expect her, as an artist, to prefer the color perception of her right eye. If that proves true, I would recommend a silicone IOL (LI61AO, Bausch + Lomb) for the left eye. The same IOL could be used if an IOL exchange is performed in the right eye.
What I Did: Christopher E. Starr, MD
I sighed with relief after reading the preceding expert commentary. This patient was the first in my career with this particular complaint, and I was not quite sure that my management strategy would work.
Despite her concern about rainbow glare, we agreed that the advanced cataract in the left eye was a bigger issue, so we opted to tackle that first. Central topography was normal, and the EBMD was peripheral and subtle. A superficial keratectomy was therefore not deemed necessary before cataract surgery.
Cataract surgery was performed with a standard (5.5-mm) capsulorhexis and traditional phacoemulsification; a femtosecond laser was not used. Like the panelists, the patient and I decided that a different IOL model should be implanted. Although an LI61AO is a reasonable choice here, we chose to target monovision with an AcrySof IQ aspheric, monofocal, nontoric, preloaded IOL without a blue-light filter (model ACU0T0, Alcon).
As mentioned by Dr. Gatinel, microscratches and subtle defects on the surface of an IOL optic can have long-lasting negative visual consequences, and they were ultimately the likely cause of this patient’s dysphotopsias. A preloaded IOL was selected for the left eye in order to minimize potential scuffs from extra manipulation and handling.
Rainbow aberrations were not present 1 day after surgery and are still not present 1 year postoperatively. The patient is so happy with her binocular UCVA that she has gradually become less bothered by the unilateral rainbow aberrations in the first eye and has, thankfully, opted not to pursue further intervention to address them.
1. Masket S, Fram NR. Pseudophakic dysphotopsia: review of incidence, cause, and treatment of positive and negative dysphotopsia. Ophthalmology. 2020:S0161-6420(20)30787-9.
2. Masket S, Rupnick Z, Fram NR, Kwong S, McLachlan J. Surgical management of positive dysphotopsia: U.S. perspective. J Cataract Refract Surg. 2020;46(11):1474-1479.





