The utility of a femtosecond laser in cataract surgery remains a subject of debate. Naysayers make a valid point when they note that most experienced cataract surgeons using standard phaco techniques achieve excellent outcomes without incurring the additional expense of a femtosecond laser. Several large-scale studies have compared outcomes with laser cataract surgery and phaco cataract surgery, but none has demonstrated postoperative refractive superiority with the former.1,2
I started performing laser cataract surgery at the same time as many of my colleagues. For a couple of years, I used the three available major platforms in most of my cataract procedures.3 I found the technology’s ability to soften or fragment a dense nucleus and create a perfectly round capsulotomy impressive. I did not find, however, that the technology offers a significant advantage in exchange for the following:
- The increased cost of purchasing and maintaining a laser;
- The greater cost per procedure to the patient;
- The longer surgical time;
- The need for extra space in or near the OR;
- The risk of increased IOP from laser suction; and
- The cosmetically redder eye after laser treatment.
That said, I recognize that laser cataract surgery can offer advantages over phacoemulsification for certain types of cataracts. These include extremely dense nuclear cataracts, posterior polar cataracts associated with a high risk of a torn posterior capsule, cataracts in eyes with fibrous anterior capsules, mildly subluxated cataracts in eyes with weak zonules, and white cataracts, the focus of this article.
THE CHALLENGES PRESENTED BY A WHITE CATARACT
The most feared challenge of operating on a swollen, milky white cataract is the Argentinian flag sign, which is seen when the anterior lens capsule tears diametrically across the lens, with possible extension to the posterior capsule. Several maneuvers have been suggested to mitigate this risk. They include staining the anterior capsule with trypan blue dye to improve visualization of the anterior capsule during the capsulorhexis, immediate aspiration of the lens milk to decompress the capsular bag and lower the intralenticular pressure, and massage of the peripheral lens milk toward the capsulotomy puncture site. These maneuvers can reduce—but not eliminate—the risk that the Argentinian flag sign will develop (Figure).
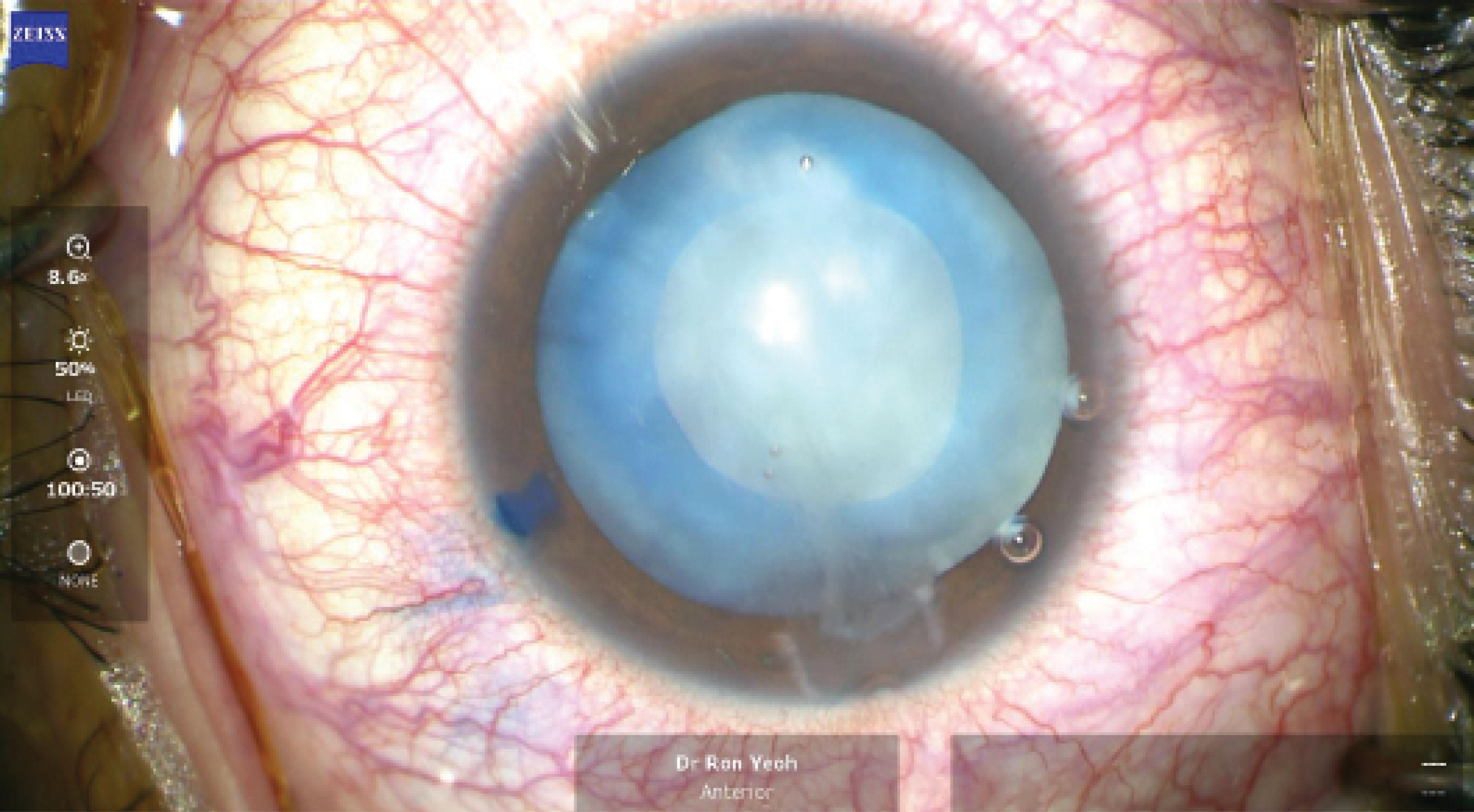
Figure. In an eye with a white cataract, good control of intralenticular pressure after a manual CCC can help to prevent a radial tear.
UTILITY OF A FEMTOSECOND LASER
It generally is not possible to perform laser fragmentation of the nucleus of a white cataract, and many cataract surgeons do not use a femtosecond laser to create incisions. The main utility, therefore, of a femtosecond laser in these eyes is its ability to create a more predictably sized and round capsulotomy.
Each laser platform completes the steps of the laser cataract procedure at a different speed, and the duration of each step therefore varies.3 In an eye with a white cataract, the only parameter that matters is the speed of the capsulotomy. If this step takes 5 seconds to perform, a lot of time elapses between the first puncture of the anterior capsule by the laser (when the intralenticular pressure is at its highest) and completion of the capsulotomy (when radial extension of any perforation of the anterior capsule is possible). This, of course, means that lens milk may obstruct completion of the laser capsulotomy.
What if the laser capsulotomy takes less than a second to complete and decompression of the capsular bag occurs almost simultaneously over the entire circumference of the capsulotomy? I believe that rapidly performing a laser capsulotomy may offer the following advantages:
- A lower risk of the Argentinian flag sign;
- A better-sized (4.5–5 mm) capsulotomy, which would allow a one-piece IOL to be implanted in the bag with reverse optic capture or a three-piece IOL to be implanted in the sulcus if a posterior radial extension of the tear occurs; and
- The lysis of unseen fibrous bands in the anterior lens capsule.
SAFETY
An incomplete tear. There is little evidence that a laser capsulotomy is safer than a manual continuous curvilinear capsulorhexis (CCC) in an eye with a white cataract. A study conducted in Singapore found that the laser capsulotomy was incomplete in 10 of 58 (17.2%) eyes.4 Surgeons must therefore pay close attention to the steps of cataract removal following the laser capsulotomy.
The anterior lens capsule should be scrutinized under the operating microscope to detect whether a round, completely free anterior capsular flap was created. Staining the capsule can facilitate inspection. Often, one or two areas can be detected where the capsulotomy is incomplete. In this situation, an OVD may be injected to tamponade the anterior capsule, the edge of the CCC where incomplete perforation is suspected may be teased out, and the tear may be gently completed with either a cystotome or a pair of capsule forceps. Once a free capsular flap has been confirmed, the nucleus, epinucleus, and cortex may be removed and an IOL implanted.
Complication rates. A prospective comparative study of 80 eyes found no difference in complication rates between a laser capsulotomy and conventional manual CCC in eyes with a white cataract.5 This observation, however, holds true only if proper technique for a multistepped or two-stepped manual CCC is used on an eye with a swollen lens to reduce the risk of a radialized tear. For a laser capsulotomy to offer advantages over a CCC, the former would have to be a better size, more centrally located, and more uniform in shape.
CONCLUSION
Laser technology has matured and can now offer advantages for surgery on certain challenging cataracts. To my mind, this is where the utility of a femtosecond laser is greatest.
1. Manning S, Barry P, Henry Y, et al. Femtosecond laser-assisted cataract surgery versus standard phacoemulsification cataract surgery: study from the European Registry of Quality Outcomes for Cataract and Refractive Surgery. J Cataract Refract Surg. 2016;42(12):1779-1790.
2. Day AC, Burr JM, Bennett K, et al; FACT trial group. Femtosecond laser-assisted cataract surgery compared with phacoemulsification cataract surgery: randomized noninferiority trial with 1-year outcomes. J Cataract Refract Surg. 2020;46(10):1360-1367.
3. Yeoh R. Practical differences between 3 femtosecond phaco laser platforms. J Cataract Refract Surg. 2014;40(3):510.
4. Chee SP, Chan NS, Yang Y, Ti SE. Femtosecond laser-assisted cataract surgery for the white cataract. Br J Ophthalmol. 2019;103(4):544-550.
5. Titiyal JS, Kaur M, Singh A, Arora T, Sharma N. Comparative evaluation of femtosecond laser-assisted cataract surgery and conventional phacoemulsification in white cataract. Clin Ophthalmol. 2016;10:1357-1364.