The use of smartphones is ubiquitous in modern society. Most ophthalmologists and trainees own a smartphone. Ironically, most of us probably use the telephone feature of our phones far less than we use the remaining features. With regard to ophthalmology, the smartphone has a number of useful capabilities, but the most commonly utilized are the camera and third-party applications.
Smartphone apps may be used to test patients during the examination, including but not limited to visual acuity, contrast sensitivity, visual field using the Amsler grid, and color vision (Eye Handbook, www.eyehandbook.com; University of Missouri, Kansas City, and Cloud Nine Development). They may be used to show patients model eyes, to explain conditions, to interact with colleagues, to obtain American Academy of Ophthalmology material, or as a reference for the physician to search disease signs, symptoms, required testing, treatment protocols, and medication doses. Moreover, new apps that enable at-home screening of common disorders are becoming popular for patient use.
For photography, a number of third-party apps have also been developed to extend the range of functions of the native camera app that comes preinstalled with most smartphones. Most of my experience has been with the iPhone 3G, 4, and 5S (Apple); however, almost everything discussed in this article is applicable to all versions of the iPhone and to other smartphones by various manufacturers as well. The remainder of this article will focus on using the iPhone to capture high-quality slit-lamp images.
iPhone Photography Techniques
First and foremost, motion artifact is the enemy, and I would highly recommend purchasing a slit-lamp adapter. The technique of holding the iPhone to the slit-lamp ocular can certainly work,1 but an adapter helps greatly. My colleagues and I presented on a technique to build one’s own adapter using things around the clinic; however, this was before the time of commercially available adapters.2 There are now many adapters on the market, as a quick Google search will evidence. Moreover, if you extend your search to microscope and telescope adapters, you will find even more. The main thing to be aware of is which model phone you have and which model slit lamp you will be using. If you will be using numerous slit lamp models at various clinics, more of a “universal” adapter may be best.
Once you have attached your phone to the slit lamp, you may realize that the photos you take are not amazing—if you have a very bright light in almost total darkness, you may need a fill light to capture nice images. Fill lights designed to be placed in the hole for the focusing rod of the slit lamp exist, but a well-placed muscle light or a book light with a rheostat such that the light level can be adjusted (and perhaps diffused with a little paper tape) work just as well. I have used the room lights in a pinch, but strong reflections often ruin the image. Applications exist to control exposure settings of the camera (ProCamera; Cocologics), something that was previously not possible using the factory-installed camera app. Being cognizant of glare is very helpful in obtaining high-quality images, and we find that higher-magnification images generally turn out better.
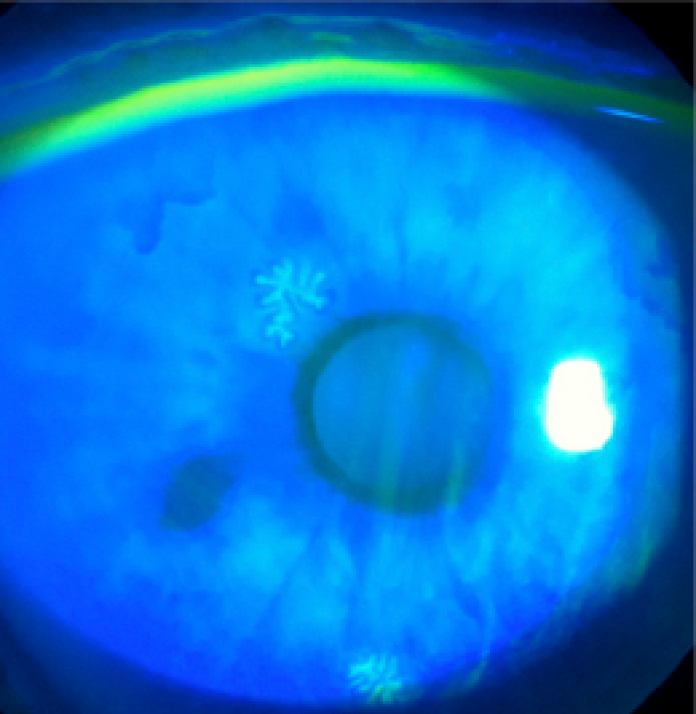
Herpes simplex virus epithelial keratitis imaged using diffuse illumination with cobalt blue and fluorescein.
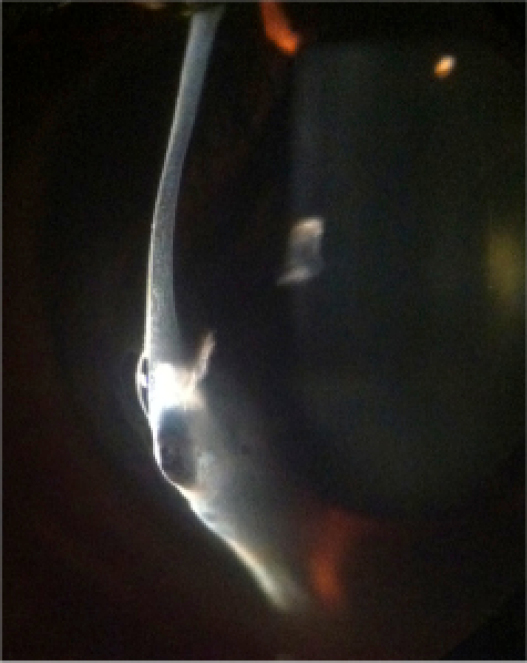
Acute corneal hydrops in keratoconus imaged using an optical section.
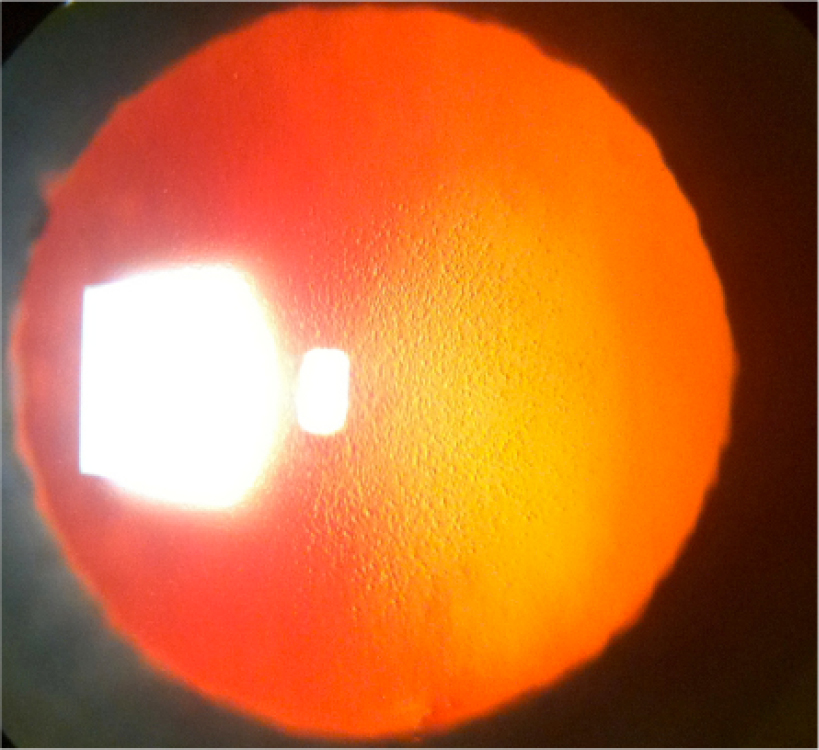
Fuchs endothelial corneal dystrophy imaged in retroillumination.
We have found that all imaging techniques including diffuse illumination (with or without fluorescein and cobalt blue; Figure 1), direct illumination (including optical section; Figure 2), indirect illumination, retroillumination (Figure 3), sclerotic scatter (Figure 4), and even specular microscopy are possible. Fundus imaging is possible, and although imaging with a 90D or 78D lens can be performed, we have found that a contact lens is best, as it stabilizes the image and reduces glare (Figure 5). Moreover, gonioscopy has also been performed with success. We recommend using a three-mirror lens, as a four-mirror lens that requires delicate contact can be difficult, although possible (Figure 6).
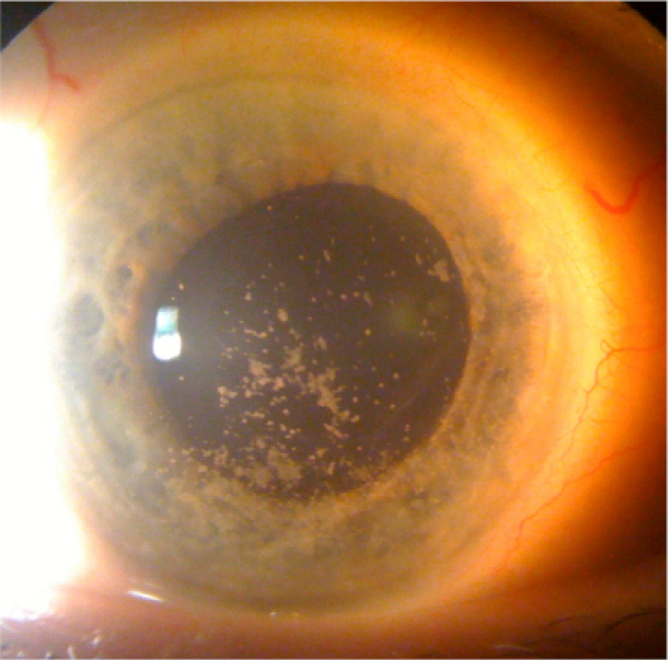
Sclerotic scatter used to highlight corneal lesions.

Fundus photograph of an optic nerve pit.
Gonioscopic image.
One app (Camera Mic; Gamblus) allows a picture to be captured when the decibels of the room reach a certain level, eliminating the need for the user to touch the camera; however, because it is a third-party app, it cannot be used concurrently with another third-party app, which we often use to control exposure. Our preferred method is to dangle the iPhone headphones to have them sit on the joystick of the slit lamp. The button on the headphones can be used to capture the image. Touching the screen may induce subtle motion artifact, so we tend to avoid it.
Smartphone videography is another technique that can be performed. If it is difficult for the patient to remain still, one can film and then later extract the still frames; however, it must be stressed that the image quality is less than that of still photographs. Moreover, videos may be taken intentionally to show motion of the patient, for example in pseudophacodonesis, or to show procedures performed at the slit lamp or at the operating microscope.
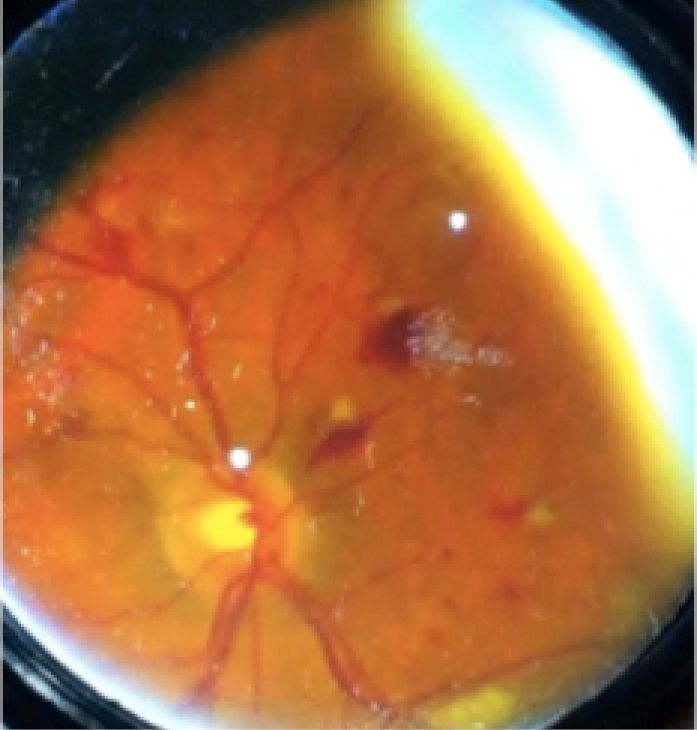
Diabetic retinopathy imaged using a 20D lens and smartphone indirect ophthalmoscopy.
Smartphone indirect ophthalmoscopy has been described and is an excellent way to image the fundus in scenarios where fundus imaging is not available, such as for ICU consults (Figure 7).3
Mirroring apps, where one can mirror the screen of the iPhone on an Apple TV-enabled television or a computer monitor, are useful to show the patient, the patient’s family members, or learners in the room ocular pathology.4 Also, any procedure being performed at the slit lamp can be mirrored for learners. Ideally, for a slit-lamp procedure, the iPhone is mounted to a side scope so that the person performing the procedure retains his or her stereopsis. This technique can also be used with the laser.
TORIC IOL ALIGNMENT
In our most recent publication on smartphone photography,5 we investigated the use of smartphones to measure toric IOL alignment. Third-party photography apps for the iPhone that use the internal accelerometer to display a level are available, and, in our study, we used Camera Awesome (SmugMug). Without a level, one cannot be sure that that photographs are taken properly. Once the phone is leveled and the patient’s head is straight in the slit lamp, the axis of the IOL can be measured. There are numerous apps discussed in the article that may be used; however, our preferred technique is to transfer the images to a laptop and use ImageJ6 to easily and accurately read the IOL position from the screen.
SUMMARY
Numerous apps exist to extend the camera function of smartphones to enable level photographs to be taken as well as to ensure good exposure and lighting. Adapters to decrease motion artifact and to free one’s hand from holding the phone are also available. Headphones can be dangled from the phone so that images can be captured without one’s hand leaving the joystick. The smartphone can be set up on a side scope so that the examiner can retain binocularity, and applications exist to mirror the smartphone display onto a television or computer monitor. The uses of smartphones in ophthalmology are countless, and as the technology continues to evolve, their utility will only increase.
1. Teichman JC, Sher JH, Ahmed IK. From iPhone to eyePhone: a technique for photodocumentation. Can J Ophthalmol. 2011;46:284-286.
2. Teichman JC, Sher JH, Sabri K, Ahmed IK. Technique for attaching a cellphone to a slit-lamp biomicroscope ocular for anterior segment photography. Paper presented at: The Association for Research in Vision and Ophthalmology Imaging Conference; April 30, 2011; Fort Lauderdale, FL.
3. Bastawrous A. Smartphone fundoscopy. Ophthalmology. 2012;2:432-433.
4. Teichman JC, Sher JH, Sabri K, Ahmed IK. Development of slit lamp camera-phone adapter and technique for digital photography and live streaming of pathology and procedures. Paper presented at: the American Society of Cataract and Refractive Surgery Symposium and Congress; April 21-24, 2012; Chicago, IL.
5. Teichman JC, Baig K, Ahmed II. Simple technique to measure toric intraocular lens alignment and stability using a smartphone. J Cataract Refract Surg. 2014;40(12):1949-1952.
6. Rasband W. ImageJ; Image Processing and Analysis in Java. Research Services Branch, National Institute of Mental Health. Available at: https://rsb.info.nih.gov/ij/. Accessed November 3, 2014.




