Over the past 20 years, I have participated in an average of six or seven trips per year to developing parts of the world to perform cataract surgery and to teach local physicians sustainable surgical techniques (Figures 1 through 4). The ultimate goal of these missions—and the reason we travel to the same place multiple times—is to transfer surgical skills in a way that the doctors on the ground can treat their local cataract patients in a safe, effective, and efficient manner.

Figures 1 to 4 | Dr. Crandall on various mission trips. The ultimate goal, he says, is to transfer surgical skills in a way that the doctors on the ground can treat their local cataract patients in a safe, effective, and efficient manner.
Cataracts seen the developing world are almost always bilaterally white. In the United States, a cataract surgeon might see such a case once every 6 months. Without experience and the proper skill set, these cases can be quite challenging. In our humanitarian efforts, we perform and teach small-incision extracapsular cataract extraction and phacoemulsification when appropriate. These skills, with accompanying chopping maneuvers and techniques, are difficult to transfer. A standard extracapsular surgery requires a rather large incision, about 7.0 mm externally and 10.0 mm internally.
AN EASIER WAY
In a setting of high volume and low technology, I have found the miLoop (Carl Zeiss Meditec, formerly IanTech) to be an advantageous tool. This device—in essence, a modernized snare—allows the surgeon to more easily and efficiently grab the lens and crack it in half. By teaching extracapsular surgery that employs the miLoop, we enable local physicians to perform a small-incision technique safely and with confidence. A seemingly simple technology transfer via the miLoop provides a big teaching advantage and helps build a sustainable method of providing sight-saving cataract surgery to the local population.
Although phacoemulsification may be common in advanced societies, it is far too expensive in most developing areas. The handheld miLoop device has a nitinol filament snare that is maneuvered to allow for zero-energy lens fragmentation on any grade cataract. By relying on centripetal forces, the device can perform gentle, controlled nuclear breakup (Figure 5). In contrast, the centrifugal forces employed through standard phaco chop dissection create outward forces on the capsular bag and zonules.
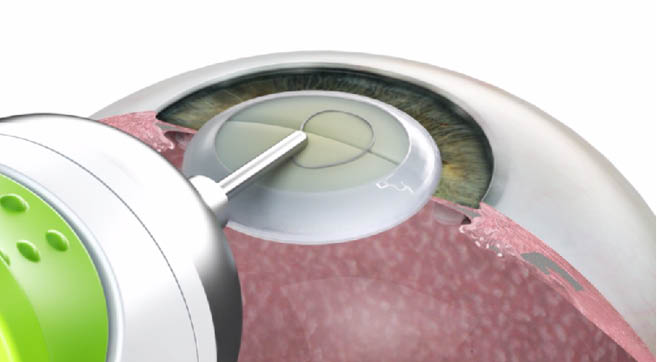
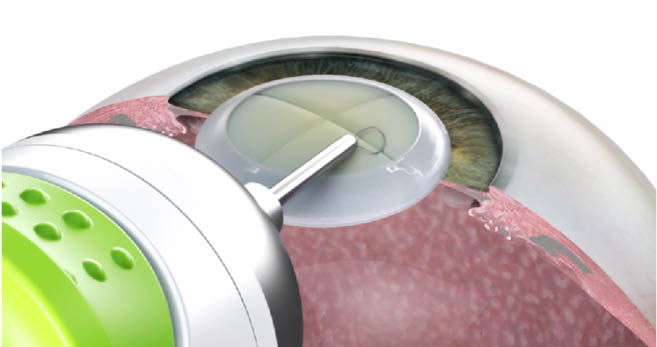
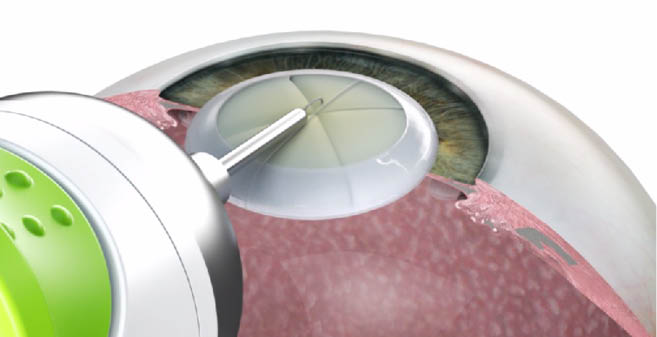
Figure 5 | The miLoop device has a nitinol filament snare that is maneuvered to perform gentle, controlled nuclear breakup.
A less-traumatic approach is crucial for patients with a wide variety of conditions such as dense lenses, endothelial disease, zonular instability, and small pupils, all of which are more common in the developing world. In these areas, many cataract patients also have coexisting glaucoma and thus often have dense cataracts, narrow angles, and pseudoexfoliation.
THE EVIDENCE
A randomized study was conducted to compare torsional phacoemulsification with adjunctive endocapsular nuclear fragmentation using the miLoop with torsional phacoemulsification alone in 101 eyes (101 patients). The investigators found that use of the miLoop device was associated with a 40% reduction in cumulative dissipated energy in the eye.1 It should be noted that only high-grade advanced cataracts were enrolled, with more than 85% of eyes having baseline BCVA of 20/200 or worse in either group.
Additionally, my colleagues and I investigated the surgical performance of the miLoop in cases of pseudoexfoliation and capsular instability. We evaluated six patients with pseudoexfoliation and visually significant cataracts who had phacoemulsification with the miLoop. Full-thickness endocapsular lens fragmentation was performed in patients to minimize capsular stretch and destabilization. We found that full-thickness nucleus disassembly was successfully achieved in all cases. Centripetal fragmentation of the lens with the superelastic microthin filament showed capsular stability during phaco surgery and seemed to minimize additional capsular stress.
We also found that the miLoop helped the surgeon bring up the nuclear pieces without having to rotate the lens, and the device was able to loosen the epinucleus and cortex. This can help decrease the chances of disrupting the capsule by reducing the manipulation of the lens and, in turn, causing less potential stress on the zonules.
In developing countries, cost recovery is an important aspect of sustainability. Our group, Moran Outreach, has been working with ASCRS International and the Aravind Centers in India to teach the use of miLoop to reduce wound size in small-incision cataract surgery. Commonly, wounds measure 7.0 to 8.0 mm externally and 10.5 to 11.0 mm internally. Using the miLoop to bisect the nucleus, we can reduce the size of both incisions to enable reduced surgical trauma and implantation of foldable lenses. A local surgeon could bill for both advantages, helping with cost recovery.
Reducing wound size can also help local surgeons’ transition to phaco techniques for cataract surgery. Sculpting and chopping techniques to divide the nucleus are the most difficult to learn and, when incorrectly performed, can lead to complications. Once the nucleus is bisected or broken into quadrants with the miLoop, an instructor can teach fluidics and phaco techniques more quickly and more safely.
CONCLUSION
In my experience, the miLoop is easy to use and easy to teach. It does not require specialized training, and users often feel comfortable and confident with the procedure after about five cases. Further, miLoop costs about $150, making it an affordable option for resource-poor countries.
1. Ianchulev T, Chang DF, Koo E, et al. Microinterventional endocapsular nucleus disassembly: novel technique and results of first-in-human randomised controlled study. Br J Ophthalmol. 2019;103(2):176-180.
2. Singh IP, Crandall AS, MacDonald SM, Ianchulev T. Micro-interventional nucleus disassembly with self-expanding nitinol filament in pseudoexfoliation cases. Poster presented at: the ASCRS annual meeting; April 13-17, 2018; Washington, DC.



