Refinements in technique and technology have made cataract surgery a highly rewarding procedure. The presence of residual and mitotically active lens epithelial cells (LECs), however, can lead to visually disabling posterior capsular opacification (PCO)1,2 and anterior capsular fibrosis/opacification,3-6 both of which can negatively affect outcomes. The role of hydrodissection in enhancing cortical cleanup and reducing or retarding the formation of PCO is well established.7-10 Yet, cortex removal is often not given enough attention.
This article describes our simple method for thoroughly removing cortical fibers and equatorial LECs. The POPS technique takes its name from its four basic steps: positioning, occlusion, posterior displacement, and swiping.
THE POPS TECHNIQUE IN DETAIL
Scan the QR code to see the POPS technique executed.
Positioning
In the first step, the aspiration probe is positioned so that the aspiration port is located under the anterior capsular fibers beyond the capsulorhexis margin (Figure 1A). Care must be taken to keep the probe a safe distance from the capsulorhexis edge and posterior capsule and to ensure that the aspiration port faces the corneal endothelium.
Occlusion
Next, the footpedal is depressed to occlude the anterior fibers with minimal vacuum.
Posterior displacement
With the port occluded, the aspiration probe is then directed posteriorly to detach the cortical fibers from the undersurface of the anterior capsule (Figure 1B).
Swiping
Gentle swiping movements of the probe in a circumferential arc then detach these fibers from the capsular fornices (Figure 1C). The vacuum level is increased, the aspiration port is brought to the center, and the fibers are aspirated completely using linear vacuum (Figure 1D). Aspiration starts within the capsular fornices after the swiping movements are performed to separate the cortex from the capsule. The vacuum level is increased as occluded fibers are brought to the center and aspirated.
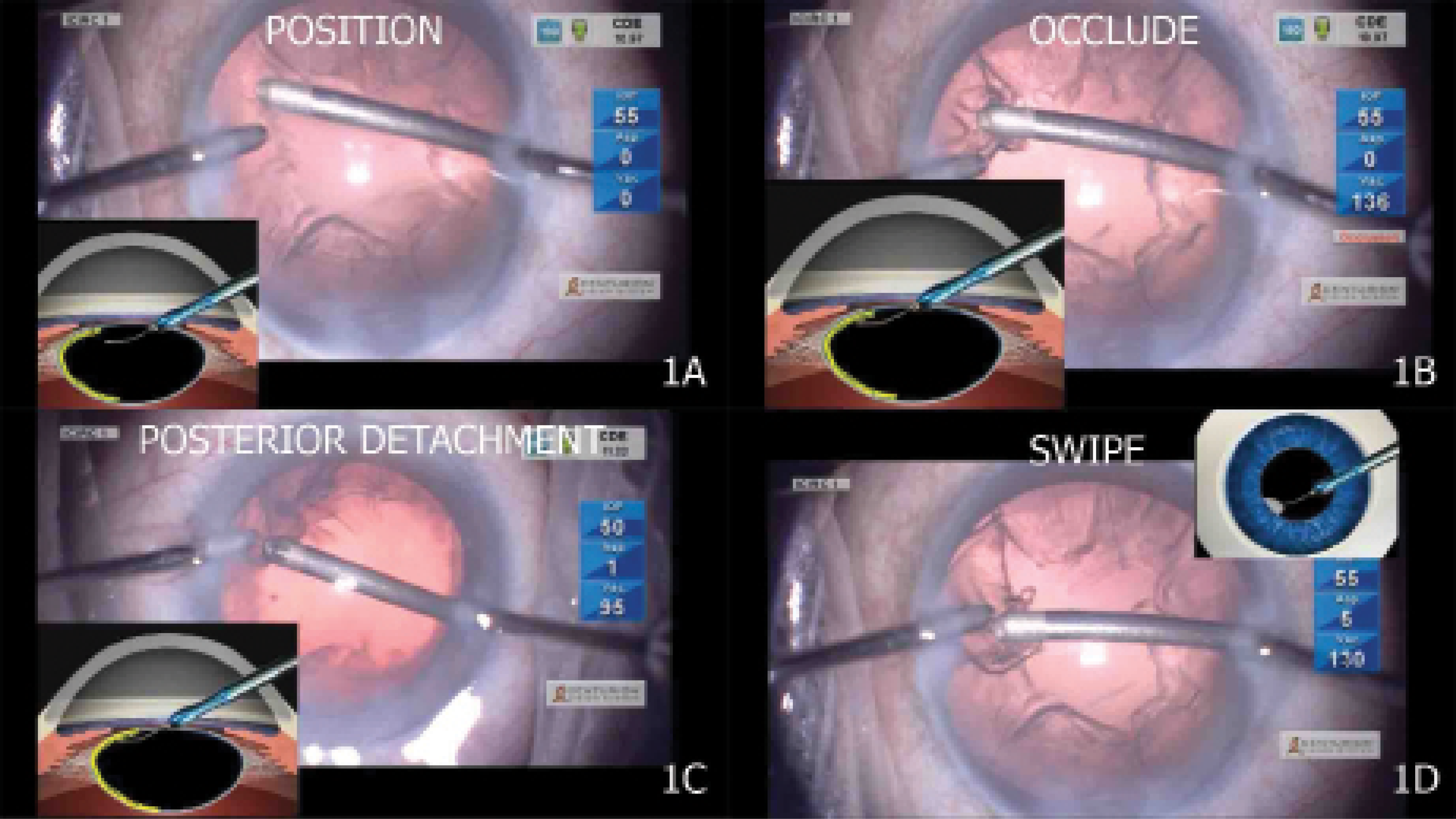
Figure 1. The aspiration port is positioned beneath the cortical fibers well beyond the anterior capsulorhexis margin (A). Vacuum is built up by depressing the footpedal to achieve occlusion at the aspiration port (B). The entire aspiration probe, with the occluded fibers, is depressed posteriorly with the port still facing upward (C). With the aspiration port occluded, side-to-side movements of the entire probe are performed to free the equatorial cortical fibers from the capsular attachments in the fornix (D).
OTHER CONSIDERATIONS
The capsule is vacuumed if doing so is deemed necessary by the surgeon, but this is not a part of the POPS technique.
An I/A tip of any style and material may be used. The POPS technique can be performed using bimanual or coaxial irrigation and aspiration. We use this technique with bimanual irrigation and aspiration for all cases, including eyes with small pupils, pseudoexfoliation syndrome, and zonular weakness.
Our parameters for cortical aspiration are as follows: a vacuum level of 300 to 400 mm Hg, an aspiration flow rate of 20 mL/min, and a bottle height of 80 to 90 cm.
PCO AND LECS
Comparisons
Polishing of the anterior and posterior capsules cannot prevent PCO if mitotically active equatorial LECs are left behind after cataract surgery.1-4 The best way to minimize PCO formation is to remove the equatorial cortical fibers containing the germinative B-type LECs as thoroughly as possible. Good cortical cleaving hydrodissection7 and subsequent meticulous cortical cleanup are well-recognized steps to remove cortex effectively and thereby reduce the incidence of PCO.8,9
During conventional cortical aspiration, the aspiration port is placed just under the capsulorhexis margin, and the anterior cortical fibers are occluded. These fibers are then aspirated by pulling the instrument radially toward the center in a single motion. This centripetal pull can detach the anterior subcapsular fibers; it can also, however, break the attachment of these fibers in the equatorial region, leaving cortical fibers and LECs behind in the capsular fornices, where the material may be invisible to the surgeon. A radial pull of the fibers can also place stress on the zonular apparatus and cause localized zonular dehiscence. This is of particular concern in eyes with conditions like preexisting zonular pathology from trauma, pseudoexfoliation syndrome, and Marfan syndrome.
In response to these issues, Nakano and colleagues developed the hurricane technique for cortical removal.11 Tangential traction is applied circumferentially around the capsular bag. This has been shown11,12 to place less stress on the zonules than do the radial pulling forces exerted during conventional irrigation and aspiration. Like the hurricane technique, the POPS technique involves a circumferential swiping motion, but it also involves the posterior displacement of the aspiration probe, which we find removes cortical fibers more completely and with a relatively lower level of vacuum.
Results
We have used the POPS technique during cataract surgery on more than 500 eyes and have encountered no complications such as zonular dialysis or posterior capsular rupture during cortical aspiration. We obtained digital retroillumination images of 500 of these eyes and found no evidence of PCO in any of them at 1 or 12 months after cataract surgery. In our experience, the POPS technique promotes thorough and complete removal of the cortical fibers, and it seems to be effective at LEC removal from the capsular fornices (Figure 2).
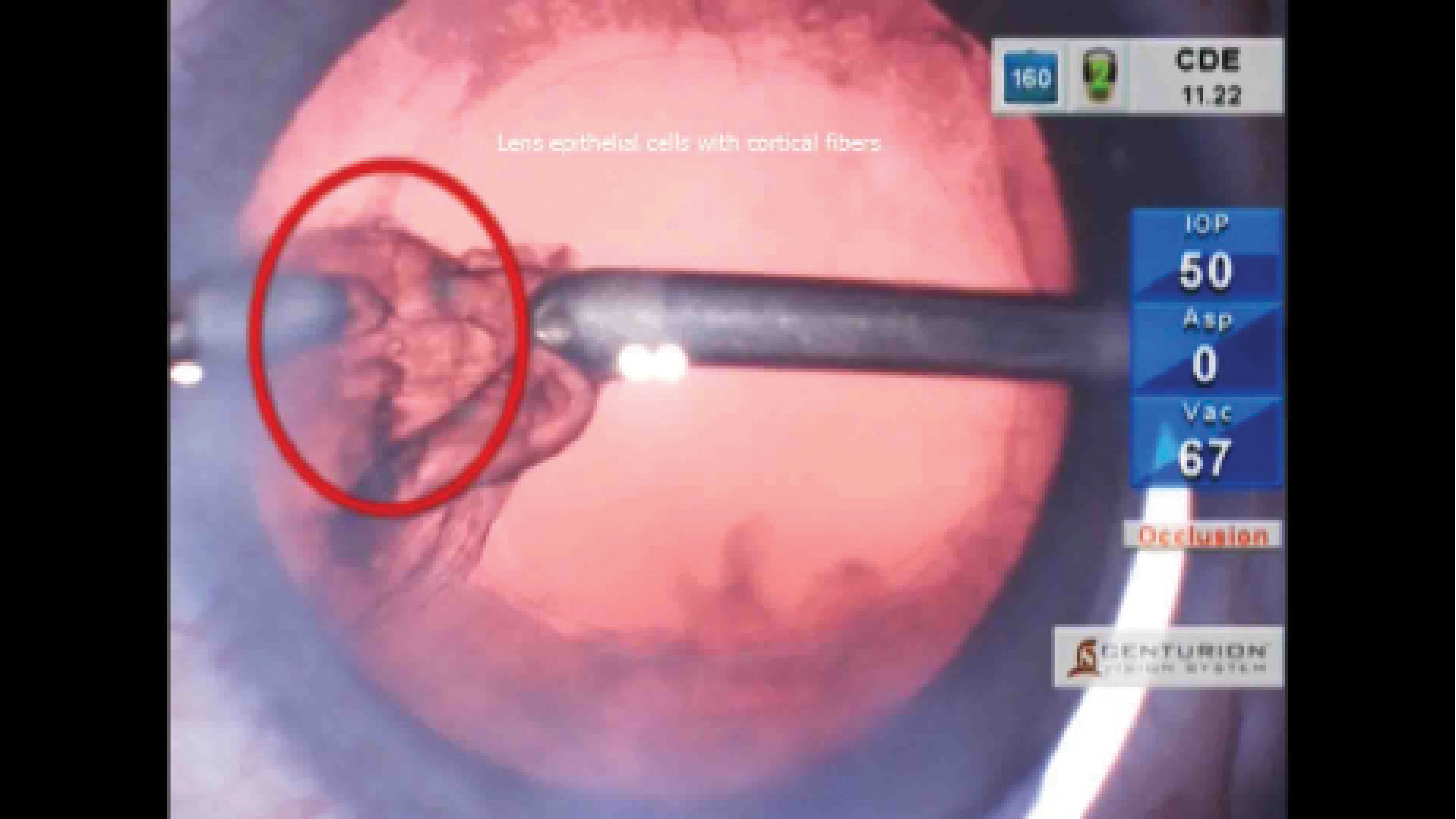
Figure 2. LECs (red circle) are removed along with cortical fibers during irrigation and aspiration.
LEARNING CURVE
We have found the POPS technique to be suitable for both beginner and experienced surgeons. The learning curve for the technique is short, but it is important to note that both the posterior displacement and side-to-side swiping movements should be performed only after there is occlusion at the aspiration port. The POPS technique can be useful in eyes with cortical-capsular adhesions,13 zonular weakness, pseudoexfoliation, or posterior capsular rupture if cortical removal is being performed with an I/A probe or a vitrector.
It is worth noting that the POPS technique can also be a useful option in patients undergoing laser cataract surgery. Cortical removal can be different in these eyes compared to those undergoing phacoemulsification because a femtosecond laser creates a sharply cut cortical edge. The POPS technique may therefore offer an advantage over a conventional radial pulling technique because the aspiration port is placed underneath the bulk of the cortical fibers.
1. Apple DJ. Influence of intraocular lens material and design on postoperative intracapsular cellular reactivity. Trans Am Ophthalmol Soc. 2000;98:257-283.
2. Werner L, Apple DJ, Pandey SK. Postoperative proliferation of anterior and equatorial lens epithelial cells: a comparison between various foldable IOL designs. In: Buratto L, Osher R, Masket S, eds. Cataract Surgery in Complicated Cases. Slack; 2000:399-417.
3. Werner L, Pandey SK, Escobar Gomez M, Visessook N, Peng Q, Apple DJ. Anterior capsule opacification: a histopathological study comparing different IOL styles. Ophthalmology. 2000;107:463-467.
4. Werner L, Pandey SK, Apple DJ, Escobar Gomez M, McLendon L, Macky T. Anterior capsule opacification: correlation of pathological findings with clinical sequelae. Ophthalmology. 2001;108:1675-1681.
5. Gayton JL, Apple DJ, Peng Q, et al. Interlenticular opacification: clinicopathological correlation of a complication of posterior chamber piggyback intraocular lenses. J Cataract Refract Surg. 2000;26:330-336.
6. Werner L, Apple DJ, Pandey SK, et al. Analysis of elements of interlenticular opacification. Am J Ophthalmol. 2002;133(3):320-326.
7. Fine IH. Cortical cleaving hydrodissection. J Cataract Refract Surg. 1992;18(5):508-512.
8. Peng Q, Apple DJ, Visessook N, et al. Surgical prevention of posterior capsule opacification. Part II. Enhancement of cortical cleanup by focusing on hydrodissection. J Cataract Refract Surg. 2000;26(2):188-197.
9. Vasavada AR, Singh R, Apple DJ, Trivedi RH, Pandey SK, Werner L. Efficacy of hydrodissection on intraoperative performance: randomized study. J Cataract Refract Surg. 2002;28(9):1623-1628.
10. Vasavada AR, Raj SM, Johar K, Nanavaty MA. Effect of hydrodissection alone and hydrodissection combined with rotation on lens epithelial cells: surgical approach for the prevention of posterior capsule opacification. J Cataract Refract Surg. 2006;32(1):145-150.
11. Nakano CT, Motta AF, Hida WT, et al. Hurricane cortical aspiration technique: one-step continuous circular aspiration maneuver. J Cataract Refract Surg. 2014;40:514-516.
12. Vasavada AR, Goyal D, Shastri L, Singh R. Corticocapsular adhesions and their effect during cataract surgery. J Cataract Refract Surg. 2003;29(2):309-314.