
My Favorite MIGS Pearls
Michael Greenwood, MD
When it comes to MIGS, it’s all about the view.
1. “Choke up” or hold the handle of the gonio prism close to the lens itself so that you can rest your hand on the patient’s head and float the prism on the surface of the cornea. This helps to avoid unintended pressure and corneal striae, which can limit the view.
2. After filling the anterior chamber with cohesive viscoelastic, place some dispersive viscoelastic just inside the main incision. The dispersive viscoelastic is less likely to burp out, so you will maintain the anterior chamber and limit any corneal striae that could hinder your view.
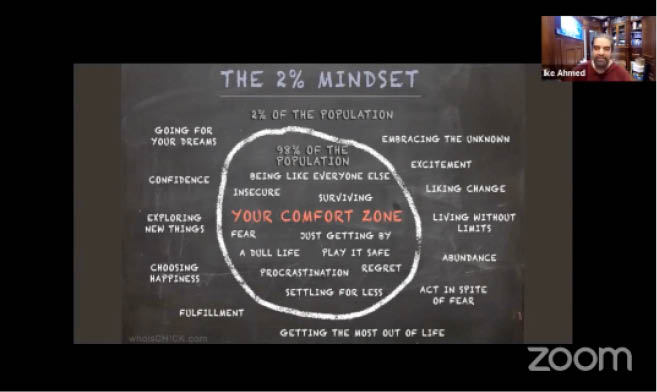
Webinar: Out of the Comfort Zone
Host Iqbal Ike K. Ahmed, MD, FRCSC, leads panelists in a discussion on the importance of stepping outside of one’s comfort zone. Dr. Ahmed and guests also touch on a range of hot topics related to glaucoma, including measuring IOP outside the office, setting more aggressive target IOPs, exploring the role of MIGS globally, and more.

My Favorite MIGS Pearls
Larissa Camejo, MD
There are so many valuable MIGS pearls to share, but here are a few of my favorites.
1. Combine MIGS with complementary mechanisms of action. For example, combining MicroPulse laser treatment (Iridex) and the Omni Surgical System (Sight Sciences) has served me well in achieving target IOP in patients who were not good candidates for conjunctival surgery. Both procedures used on their own or combined can help lower IOP effectively in patients with prior tube shunts who have above-target IOPs. More recently, I have combined Omni 360° viscodilation with implantation of the Hydrus Microstent (Ivantis) and have seen positive results.
2. Determine the best type of steroids for each MIGS procedure. For goniotomy procedures, such as the Kahook Dual Blade (New World Medical), Trabectome (MicroSurgical Technology), or Omni, I tend to prefer steroids that carry a lower chance of inducing a steroid response, such as loteprednol formulations. On the other hand, for patients undergoing Xen Gel Stent (Allergan) implantation, I use stronger formulations such as difluprednate ophthalmic emulsion 0.05% (Durezol, Alcon) and have patients start at a lower dose a few days before surgery.
3. Understand the concept of benefits and risks as it relates to MIGS. The task of balancing benefits and risks is a bit different when it comes to MIGS. For example, in my hands, the Xen stent is highly efficacious and can decrease IOP into the low teens. However, it also has the potential to scar and require needling, and although uncommon, it can cause choroidal effusions, like conventional surgery. Nevertheless, the benefits afforded to patients can be outstanding, including the ability to discontinue all (four or five) medications and stop glaucomatous progression with minimal to no postoperative discomfort. Being comfortable with bleb management is advisable for those who use the Xen device.
MIGS Unplugged: For Mentors
Educating the Next Generation of Surgeons
Iqbal Ike K. Ahmed, MD, FRCSC; Arsham Sheybani, MD; and Kelly Muir, MD
MIGS Unplugged: For Mentees
Advice on Learning to Perform MIGS Procedures
Iqbal Ike K. Ahmed, MD, FRCSC; Valentina Lozano, MD; and Jeb Ong, MD


