Poor air quality, as measured by the Air Quality Index (AQI), has adverse effects on several vulnerable patient groups. People with pulmonary conditions such as asthma, chronic obstructive pulmonary disease, chronic bronchitis, chronic sinusitis, or pneumonia as well as premature infants are at risk. However, patients with chronic dry eye disease (DED) also experience worse symptoms in environments with poor air quality and should be considered a vulnerable group.
BACKGROUND
Air pollution has been shown to cause ocular irritation, thereby contributing to or exacerbating DED, Meibomian gland disease, blepharitis, and conjunctivitis.1 In a Chinese report, patients with conjunctivitis presenting to an eye care specialist were found to have symptoms associated with increased levels of CO2 and SO2 in the air on the days before and on the day of presentation. Diesel engine exhaust has been shown to increase cytokines and chemokines in conjunctival and epithelial cell cultures.2
Other research has shown that city living is associated with lower Schirmer test scores and tear film breakup time (TBUT),3 and NO2 is associated with long-term retinal vascular changes.4 Poor AQI is associated with lung inflammation via mitogen-activated protein kinase mechanisms,5 and matrix metalloproteinase 9 (MMP-9) in lung parenchyma correlates with cigarette smoking.6 Serum inflammatory mediators have been shown to be elevated in forest firefighters during the on season compared with the off season.7
The AQI scale (Figure 1) is a method for quantifying the pollution load. In Delhi, India, the AQI has been reported to reach as high as 270—a level considered very unhealthy—but problems with air quality are widespread. Whether dealing with smog in Los Angeles or Beijing, smoke from forest fires in the west, or volcanic smog in Hawaii, patients can reference the AQI to better understand and potentially minimize their symptoms related to exposure to unhealthy air conditions.
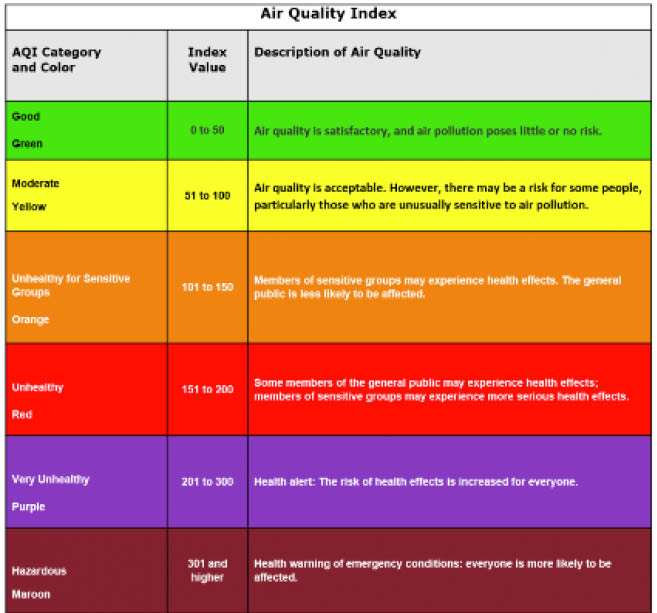
Figure 1 | Air Quality Index.
PREMISE
In September 2017 and September 2018, several forest fires broke out in the Pacific Northwest, where I practice. When performing intense pulsed light (IPL) treatments for DED during that time, I observed that patients continued to improve in their Ocular Surface Disease Index score, lid appearance, and osmolarity, as expected; however, during this time of exceptionally poor air quality, the MMP-9 results did not follow the previously predicted improvements. Instead, patients had a sudden leveling off of the MMP-9 response to IPL during the periods of poor AQI.
Later that month, while on a flight to Nashville, I noticed the massive forest fire smoke load across the entire west that cleared after crossing the Mississippi River. I had an aha moment that was the basis for explaining the aberrant data. My hypothesis was that, during an interval of poor AQI, patients had an environmentally induced increase in the tear film MMP-9 load due to poor air quality. It made sense—most campers have experienced ocular irritation and redness from campfire smoke, and the forest fires affected everyone.
To test the hypothesis, my colleague and I performed a retrospective analysis of tear osmolarity and MMP-9 in response to IPL treatment. We reexamined existing data, plotting the results against the AQI as published on www.airnow.gov. The retrospective chart review included 72 consecutive patients. Excluded were patients with no MMP-9 test before first treatment, patients with fewer than two observations, and patients whose MMP-9 score was negative at baseline. We adapted Brujic and Kading’s numerical score to evaluate the MMP-9 test results (Figure 2).

Figure 2 | The MMP-9 Grading Scale. (Adapted from Brujic M, Kading D. Making matrix metalloproteinaise-9 levels more meaningful. Presented at: Global Specialty Lens Symposium; 2016.)
We applied the random effects model to account for multiple sources of variability and various starting MMP-9 scores. The results showed that, for every one-level increase in AQI at a fixed IPL session number, MMP-9 increased by 0.338 (95% CI, 0.06–0.62). We concluded that patients with chronic DED had an increased MMP-9 burden due to poor AQI values caused by forest fires, as compared with healthy volunteers (Figures 3 through 7). Patients with DED also had increased staining with fluorescein and lissamine green.
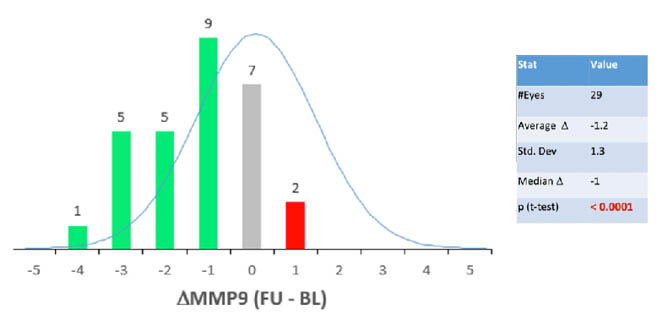
Figure 3 | The original study evaluating tear MMP-9 and osmolarity response to IPL treatment.

Figure 4 | MMP-9 levels before IPL and after IPL.
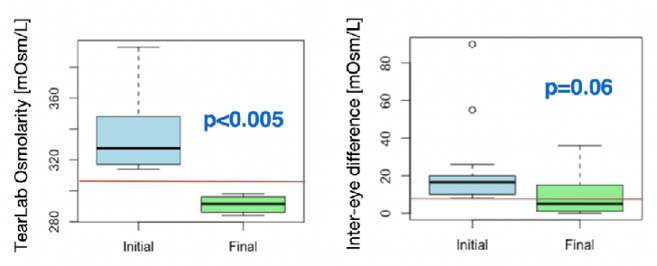
Figure 5 | Restoration of tear osmolarity: < 308 mOsm/L and inter-eye difference < 8 mOsm/L.
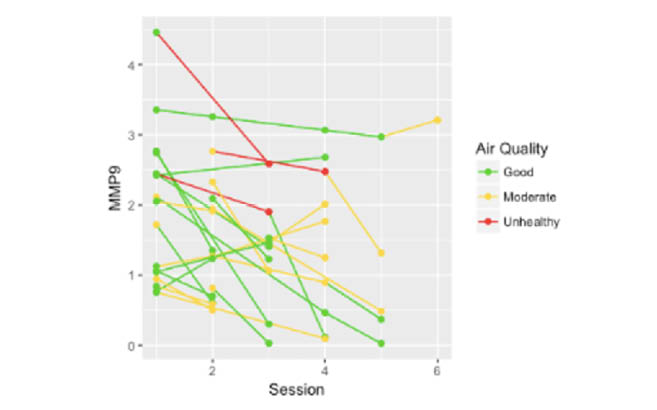
Figure 6 | MMP-9 plotted by session number across subjects and AQIs.
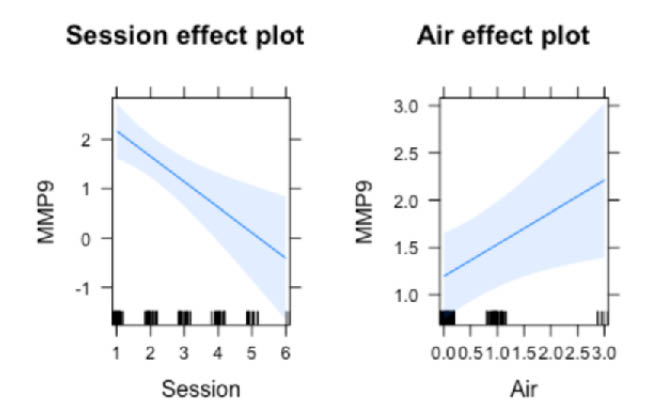
Figure 7 | Model of MMP-9 versus session number (A). Model of MMP-9 versus AQI (B).
CONCLUSION
The application of a series of IPL treatments in patients with DED or Meibomian gland dysfunction is consistently associated with statistically significant improvements in osmolarity and MMP-9. Even though patients felt better (improved OSDI scores) and had improved osmolarity, our ad hoc analysis showed that poor air quality at the time of treatment was associated with less robust improvement in MMP-9 levels for DED patients receiving IPL treatments. This is the first report to describe persistence of elevated tear film MMP-9 despite IPL therapy during periods of poor AQI.
1. Latka P, Nowakowska D, Nowomiejaska K, Rejdak R. How air pollution affects the eyes—a review. Ophthalmology. 2018;3(2):58-62.
2. Fujishiima H, Satake Y, Okada N et al. Effects of diesel exhaust particles on primary cultured healthy human conjunctival epithelium. Ann Allergy Asthma Immunol. 2013; 110(1): 37-43.
3. Saxena R, Srivastava S, Trivedi D, et al. Impact of environmental pollution on the eye. Acta Ophthalmol Scand. 2003;81(5):491-494.
4. Adar SD, Kelin R, Klein BEK, et al. Air pollution and the microvasculature: a cross-sectional assessment of in vivo retinal images in the population-based multi-ethnic study of atherosclerosis (MESA). PLoS Med. 2010;7(11)e1000372.
5. He M, Ichinose T, Yoshida S, et al. PM2.5-induced lunch inflammation in mice: differences of inflammatory response in macrophages and type II alveolar cells. J App Toxicol. 2017;37(10): 1203-1218.
6. Kang MJ, Oh YM, Lee JC, et al. Lung matrix metalloproteinase-9 correlates with cigarette smoking and obstruction of airflow. J Korean Med Sci. 2003;18(6):821-827.
7. Gianniou N, Giannakopoulou C, Dima E, et al. Acute effect of smoke exposure on airway and systemic inflammation in forest firefighters. J Asthma Allergy. 2018;99:81-88.



