A 58-year-old man with a history of a “funny-looking” left eye presents with a complaint of reduced vision and increased glare in that eye. In the past, the patient was told by an eye care professional that he was likely to experience a complication if he ever underwent cataract surgery on his left eye. He is seeking advice on how to improve the vision in that eye.
On examination, UCVA is 20/25 OD and 20/40 OS. Glare testing reduces his visual acuity to 20/80 OS. Pinhole testing does not improve visual acuity beyond 20/40 OS. No afferent pupillary defect is evident on examination, but the pupil in each eye is irregularly shaped. Extraocular motility is full. IOP is within normal limits in each eye.
A slit-lamp examination of the right eye is significant for an inferior iris defect but is otherwise normal. In the left eye, the cornea is clear, the anterior chamber is deep and quiet, and an inferior iris coloboma is present. The lens shows nuclear sclerotic changes and significant vacuole formation. An area of zonular loss is evident in the same quadrant as the iris coloboma, leading to an irregularity in the contour of the lens capsule. A retinal examination finds a small, peripheral, inferior coloboma that does not extend to the vascular arcade (Figure 1).
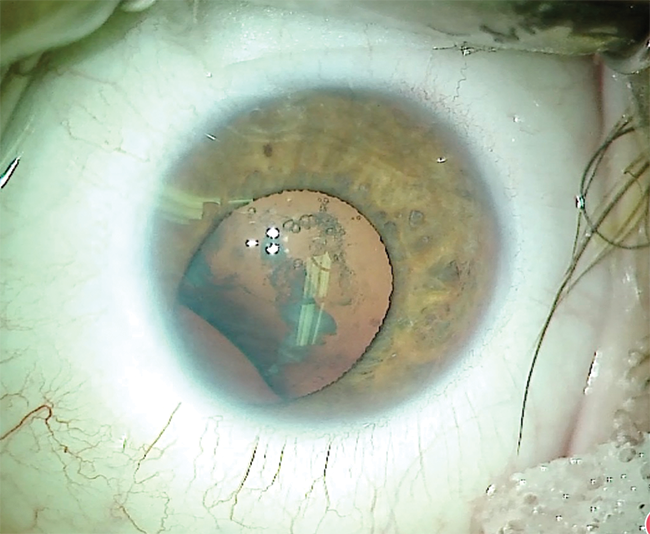
Figure 1 | Preoperative appearance of the left eye. The iris has a large inferior coloboma. The lens is cataractous with an irregular equator, indicating loss of zonular fibers in the quadrant of the coloboma.
How would you manage the cataract and anterior segment of this patient’s left eye?
—Case prepared by Brandon D. Ayres, MD

SIMONETTA MORSELLI, MD
I would perform phacoemulsification with the patient under local anesthesia and mild sedation or general anesthesia, depending on the patient’s psychological condition. I would instill a cohesive OVD in the area of the coloboma to prevent hydration of the vitreous with balanced saline solution. I would perform the capsulorhexis centered on the capsular bag, followed by careful hydrodissection and phacoemulsification using a karate chop technique and a low level of infusion with balanced saline solution. In case of vitreous loss, I would perform an anterior vitrectomy. In anticipation of possible collapse of the capsular bag, I would inject a capsular tension ring (CTR) before performing irrigation and aspiration. I would implant either a one- or a three-piece IOL. I would cover the inferior coloboma with a partial aniridia ring (Morcher).

GREGORY S.H. OGAWA, MD
There are two key points to bear in mind when considering cataract surgery on a patient with a congenital iris coloboma: (1) The optic of the IOL is only about half the diameter of a natural lens; and (2) the sides of the iris coloboma contain pupillary sphincter muscle. For a satisfactory postoperative result, the pupil must be reasonably centered, and the iris defect should be closed.
Figure 1 shows suboptimal pupillary dilation, so I would place two or three iris retractor hooks to better visualize the lens. After creating the capsulorhexis, I would place a broad-tipped capsule retractor (MicroSurgical Technology [MST]) in the area of absent zonules to minimize the chance of vitreous prolapse during phacoemulsification. In cases such as this one, I avoid using epinephrine or phenylephrine in the infusion bottle. After cataract removal, I would place a CTR and position the ends of the ring well away from the area of absent zonules. Next, I would place the IOL in the bag and orient the haptics about 90º away from the lens coloboma to decrease the chance of superotemporal IOL decentration. After OVD removal, I would inject acetylcholine (Miochol-E, Bausch + Lomb) into the anterior chamber.
I would place a 23-gauge limbal infusion cannula and use a 23-gauge vitrector (60 cuts per minute, low flow, low vacuum) to gradually remove the iris sphincter muscle from the sides of the coloboma. I would close the defect by apposing the ends of the normal pupillary sphincter and securing them with a 10-0 polypropylene suture, then work peripherally with subsequent interrupted sutures, each tied with an Ogawa intraocular knot.1
ZACHARY ZAVODNI, MD
Eyes with congenital iris and zonular coloboma can be challenging, but managing them well can be deeply satisfying for the surgeon and the patient. Prior to surgery, I would counsel this patient regarding his increased risk of vitreous loss and the need to use a zonular support device. I would also recommend iris coloboma repair at the time of cataract surgery as a means of reducing glare symptoms, minimizing pseudophakic dysphotopsias, and improving cosmesis.
During the cataract procedure, I would be extra cautious to avoid IOP fluctuations by keeping the anterior chamber formed at all times to minimize disruption of the anterior hyaloid face. I would carefully center the capsulorhexis on the lens capsule, not the pupil. Depending on the amount of intraoperative pupillary dilation, centering the capsulorhexis may require the placement of iris hooks to adequately expose the lens material opposite the coloboma. I would judge zonular strength while creating the capsulorhexis and performing hydrodissection. My expectation is that placement of a capsular hook will be required in the quadrant of missing zonules. I would disassemble the lens nucleus with zonule-friendly chopping techniques.
Before implanting the planned IOL, I would place a CTR to redistribute and equalize centrifugal forces on the bag. Based on my experience in eyes with a coloboma, I would expect the bag to center nicely after the placement of a CTR alone. In the rare instances when a bag has not centered well with just a CTR, I have placed a capsular tension segment to pull the bag back toward the quadrant of missing zonules.
After completing the cataract portion of the surgery, I would turn my attention to repairing the iris defect. My preferred technique is similar to that popularized by Robert Cionni, MD.2 In eyes with a coloboma, one cannot just directly close the defect because the iris sphincter is connected to the peripheral iris base, so direct closure will result in a severely eccentric pupil upon constriction that is pulled in the direction of the colobomatous quadrant. The solution is to separate the central iris sphincter tissue from the abnormally located peripheral sphincter tissue. To do this, I would first inject acetylcholine chloride intraocular solution into the anterior chamber and then, under an OVD, cut the pupillary sphincter in the midperiphery using intraocular scissors (MST, Figure 2). These incisions are typically 1.5 to 2 mm long (cut length is proportional to the size of the coloboma defect). Next, with a 10-0 polypropylene suture (Prolene, Ethicon), I would bring the central sphincter tissue leaflets together using a modified Siepser-type knot (Figure 3).
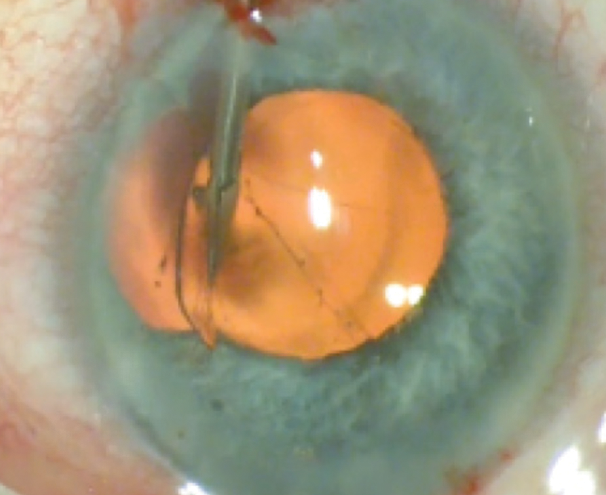
Figure 2. In a separate case, the surgeon cuts the pupillary sphincter in the midperiphery with intraocular scissors.

Figure 3. The surgeon uses a modified Siepser-type knot to bring the central sphincter tissue leaflets together.
I would then close the large remaining peripheral iris defect. This part can be challenging because, in order to bring the two edges together, one must gently pull and stretch the peripheral iris tissue centrally using intraocular micrograspers (MST, Figure 4). Doing so can create small iris defects and can frequently cause some angle bleeding. Once the peripheral iris tissue is more mobile, one can pull it centrally, close to the point where the sphincter suture was placed. Next, the peripheral defect can be fully closed with one or two modified Siepser knots (Figure 5). With this technique, the pupil ends up centralized and round, and its position shifts minimally upon constriction.

Figure 4. With intraocular micrograspers, the surgeon gently pulls the peripheral iris tissue centrally.

Figure 5. The peripheral defect is fully closed.
WHAT I DID: BRANDON D. AYRES, MD
After I had a long discussion with the patient about the risks and benefits of cataract surgery in an eye with a coloboma, he decided to proceed with surgery, which, I explained, would include cataract surgery and iris repair as well as a possible anterior or posterior vitrectomy.
Surgery began with the placement of flexible iris retractors to give me better access to the anterior capsule. I then performed a continuous curvilinear capsulorhexis (Figure 6). Next, I placed a capsular support hook in the area of zonulopathy to act as an artificial zonule. With the equator of the lens capsule supported, the lens was removed using phacoemulsification, and the cortical material was removed with bimanual irrigation and aspiration. All precautions were taken to ensure that surgery did not worsen the zonulopathy (Figure 7).
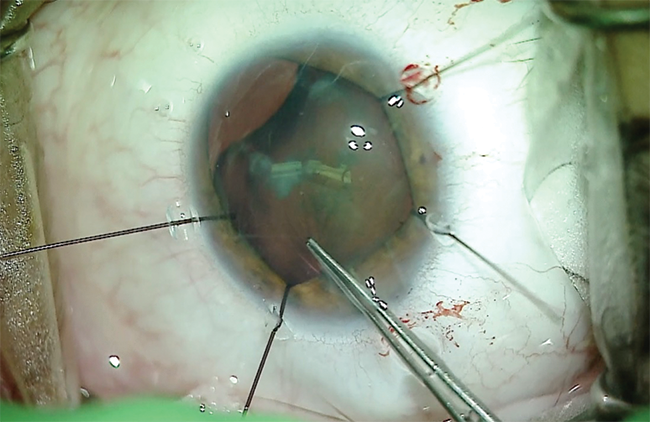
Figure 6. In this case, flexible iris retractors provide enough exposure of the anterior capsule to allow the surgeon to create a capsulorhexis.
Courtesy of Brandon D. Ayres, MD
Figure 7. A capsular support hook acts as an artificial zonule and prevents worsening of the zonulopathy. The surgeon uses bimanual irrigation and aspiration and performs tangential stripping to remove cortical material without exacerbating zonular weakness.
I was able to remove the lenticular material without extension of the zonulopathy or evidence of vitreous prolapse into the anterior chamber. I then filled the capsular bag with an OVD and placed a CTR (Figure 8). I implanted the IOL and removed the capsular and iris hooks from the eye (Figure 9).
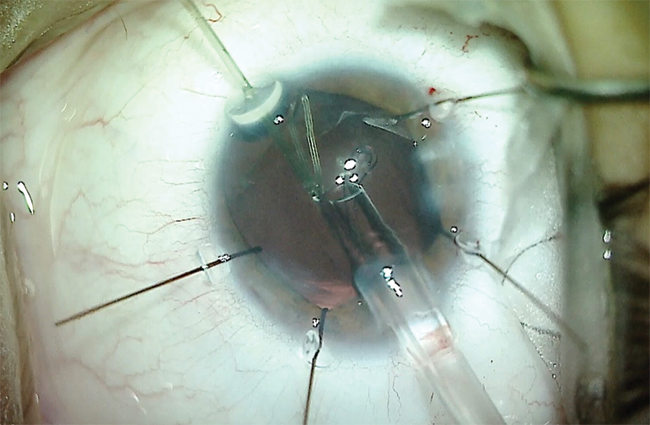
Figure 8. A CTR is placed in the capsular bag to help restore normal equatorial forces on the bag and prevent capsular phimosis.
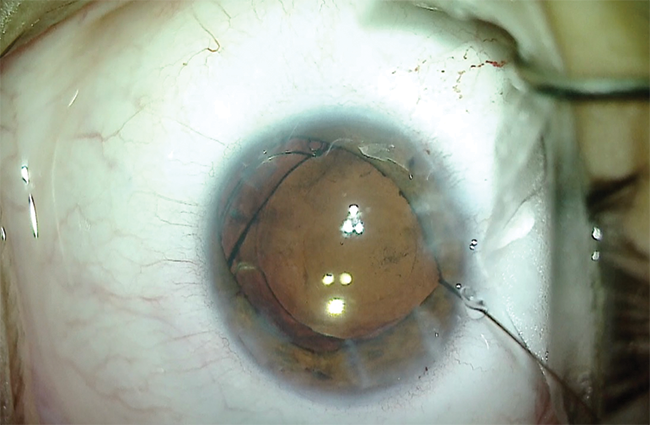
Figure 9. After implanting the IOL, the surgeon removes the capsular support hook and flexible iris retractors.
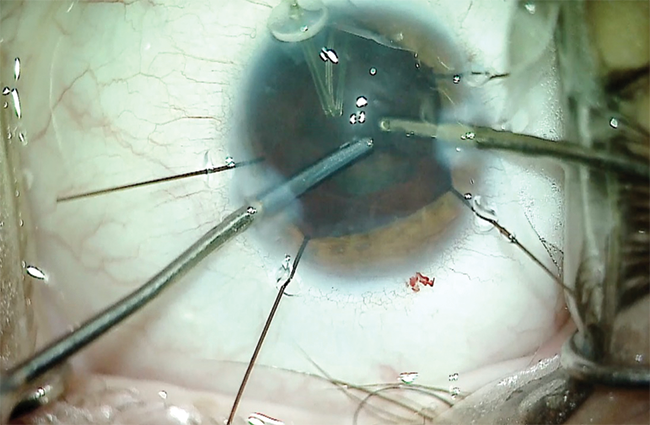
I then turned my attention to the iris defect. The goal of an iridoplasty is to cover the edge of the optic so as to prevent edge glare and leave the patient with a cosmetically acceptable pupil. The repair began with instillation of a miotic agent in the anterior chamber. The inferior iris defect was then approximated using a 10-0 polypropylene suture on a long, curved needle. The suture was tied with a sliding knot that brought the two sides of the coloboma together. Suture placement closed the inferior defect but caused significant distortion and decentration of the pupil (Figure 10).
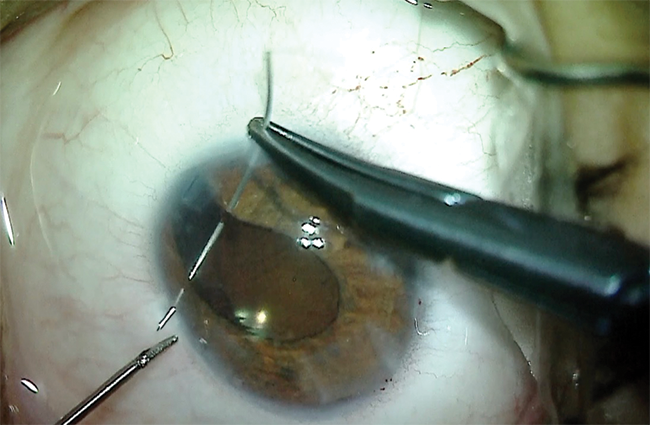
Figure 10. The coloboma repair starts with approximation of the iris tissue. The goal of the iridoplasty is to cover the edge of the optic so as to prevent postoperative glare.
I used microscissors to create several small incisions in the iris sphincter, which relaxed the shape and position of the pupil. I performed intraocular diathermy to shape and position the newly created pupil (Figure 11). The combination of relaxing incisions and intraocular cautery produced a satisfactorily sized, shaped, and centered pupil. I removed the OVD from the eye and sealed the incisions (Figure 12).
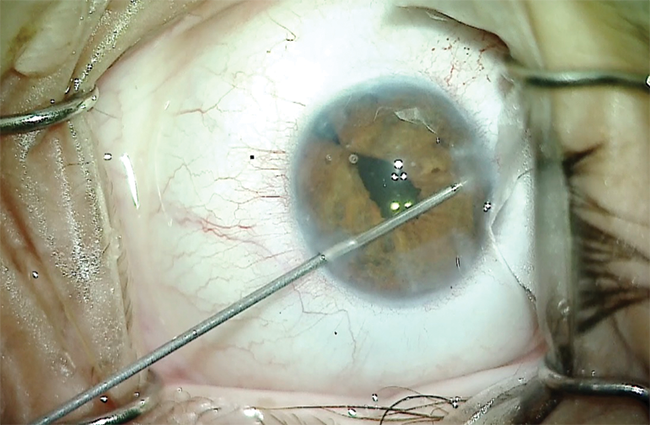
Figure 11. A combination of sphincterotomies and intraocular diathermy is used to shape and position the pupil.
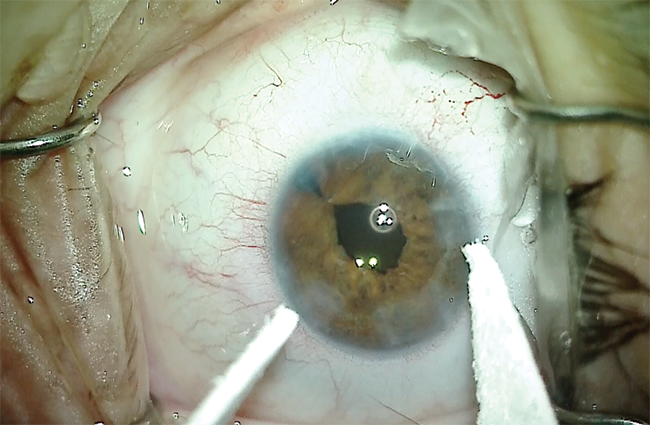
Figure 12. Final appearance of the pupil after the iris repair.
One day after surgery, UCVA was 20/50, and there was mild corneal edema and 2+ pigmented cell in the anterior chamber. After 3 weeks of therapy with topical steroids and NSAIDs, UCVA improved to 20/30, and symptoms of glare decreased dramatically. The patient was very happy with the cosmetic appearance of the eye.
1. Ogawa GSH, O’Gawa GM. Single wound, in situ tying technique for iris repair. Ophthalmic Surg Lasers. 1998;29(11):943-948.
2. Cionni RJ, Karatza EC, Osher RH, Shah M. Surgical technique for congenital iris coloboma repair. J Cataract Refract Surg. 2006;32(11):1913-1916.


